Disc herniation at the level of C5 / 6
introduction
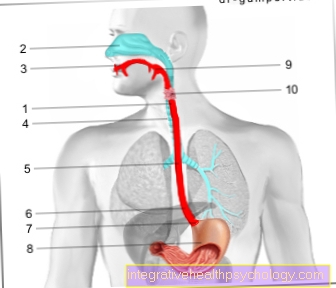
The cervical spine consists of seven cervical vertebrae. The intervertebral discs lie between two vertebral bodies of the spine and are responsible for the mobility of the spine. An intervertebral disc consists of two parts of an outer zone, the Annulus fibrosus and a gelatinous core, the Nucleus pulposus.
In the context of a herniated disc, the core of the disc shifts (Nucleus) in the direction of the spinal canal or a nerve root and breaks through the outer zone of the intervertebral disc. The spinal cord or the affected nerve root are compressed by the emerging spinal disc nucleus and the classic symptoms such as pain, sensory disturbances or even paralysis of certain muscles occur.
More detailed information on the topic "Intervertebral disc" can be found at:
- L5 syndrome
- Figure intervertebral disc
- Figure herniated disc
- Intervertebral disc

therapy
A herniated disc does not always have to be treated immediately. A conservative attempt at therapy should always be made first.
In the case of existing paralysis or more severe neurological disorders, treatment-resistant pain or worsening symptoms, an operation is necessary after 4 months at the latest (usually after about 6 weeks).
Read more on the topic Therapy of a herniated disc of the cervical spine
Conservative therapy
If the clinical examination confirms the suspicion of a herniated disc, conservative therapy should always be used first if the symptoms are minor. Pain relievers such as ibuprofen are recommended to reduce the pain. Muscle relaxants or warmth from a hot water bottle or patch can also help.
Physiotherapy is also prescribed. Resting is not called for, sport, movement and special back exercises that are learned in physiotherapy, on the other hand, make sense. Immobilization of the neck using a neck brace can be indicated especially at night, but should not be done over a longer period of time. The herniated disc can regress independently within a few weeks with these therapeutic measures.
Additional information at: Physiotherapy for a herniated disc
Exercises for a herniated disc of the cervical spine
In order to learn the correct movement of the cervical spine and to fully restore mobility, a physiotherapeutic treatment can be started. This is useful both in conservative treatment and after an operation.
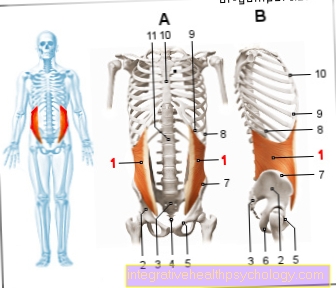
The physiotherapist performs specific exercises together with the patient and also shows exercises that can be performed alone at home. It is important that the exercises are continued at home regularly after learning. The therapy program and the exercises are individually tailored to the patient and his symptoms. The aim is to strengthen the muscles in the back and neck area and to relieve the cervical spine, for example through posture exercises.
More about this at: Exercises for a herniated disc of the cervical spine
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Exercise after a herniated disc of the cervical spine

Sport can be very useful for strengthening the back. Exercise is generally recommended after a herniated disc. Depending on the choice of sport, however, this should be discussed with the treating doctor. Going for a walk, swimming or special back training and gymnastics are recommended.
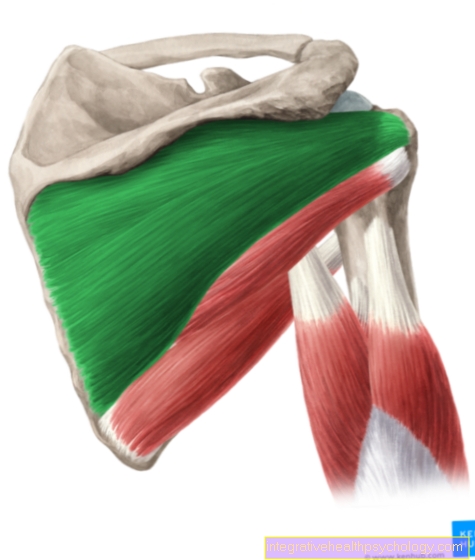
Fitness training for the shoulders and chest muscles is particularly suitable.
Sports that put a lot of strain on the cervical spine, such as tennis, should be avoided.
Read more on the topic Exercise after a herniated disc
physical therapy
Physiotherapy is the most important factor in treating a herniated disc. On the other hand, restraint may only take place briefly in acute cases or at night with increased movement. The herniated disc can recede almost completely through targeted slight movement and muscle building of the spine. Physiotherapy is also essential after an operation in order to maintain the success of the therapy and to prevent further spinal problems. The primary goal of the exercises is to restore movement after an acute herniated disc and to strengthen the muscles in the neck in the long term in order to relieve the intervertebral discs. The exercises must be learned with a professionally trained physiotherapist and continued independently at home.
Also read general information on the topic Physiotherapy / physiotherapy
Operative therapy
In the treatment of herniated discs, the trend today is in the direction of operating less often. The development is correct, since operations rarely bring about an improvement in the symptoms and operations are still carried out too often. The surgery can be either to replace or remove the disc. It has been shown, however, that adequate pain therapy and targeted exercise and muscle building also provide lasting relief from symptoms. An operation only makes sense if an acute herniated disc shows signs of paralysis and obvious nerve damage. If there are signs of irreversible damage to the nerves and the spinal cord, an emergency operation should relieve the nerve to minimize the damage. Even after long and unsuccessful physiotherapy and pain therapy, surgery can be considered if conservative measures are obviously of no use.
Imaging to prove the herniated disc must be performed prior to surgical therapy. Only if the location of the herniated disc and the clinical symptoms match does an operation make sense.
The standard procedure is the ventral discectomy, since when access is from behind, the spinal cord is always in front of the vertebral body and could be injured. The intervertebral disc is not accessed from behind via the neck / back, but from the front via the neck. The advantage of this procedure is that, in addition to the constriction caused by the intervertebral disc, bony constrictions can also be removed (e.g. through bony attachments to the vertebral bodies). With this technique, after a small incision in the neck, surrounding structures such as vessels, muscles and the windpipe are carefully pushed aside to expose the affected section of the cervical spine. The affected disc space is opened and the disc is removed completely. To stabilize the spine, a so-called cage made of titanium is inserted into the disc space. One disadvantage is that the spine stiffens in the affected area and this can restrict movement.
Nowadays there are also special intervertebral disc prostheses that can be used instead of a cage. The structure of the prosthesis is based on an intervertebral disc and maintains the mobility of the spine in the affected area. However, it can only be used in young patients who do not have degeneration of the spine. In addition, the prostheses are not optimal because of the high stress on the cervical spine.
The dorsal foraminotomy is another possible surgical technique. However, this is only used for lateral herniated discs or if there are several herniated discs that compress only one nerve root. Access is via the neck. The back muscles are gently pushed to the side in order to reach and remove the intervertebral disc at the affected level. However, this procedure is inferior to the procedure from the front for bony attachments.
Read more on the topic Surgery for a herniated disc of the cervical spine
Complications during surgery
As with any operation, this procedure also involves risks. In addition to bleeding in the surgical area, infections or wound healing disorders, nerves or spinal cord injuries can also occur. This manifests itself in sensory disturbances or disturbances of movement up to paralysis. Injury to nerves, however, is very rare. Furthermore, surrounding structures such as the windpipe, thyroid or esophagus can be injured. There may be a temporary hoarseness after the operation, but this normally disappears.
Can Osteopathy Help?
Osteopathy is an area of alternative medicine that can be used in addition to conservative or surgical therapy. In osteopathy, all areas of the body and organs are examined in order to uncover conflicts in the body and other causes of the herniated disc. The treatment includes certain manual grips and exercises that are intended to activate the body's self-healing powers and eliminate any imbalances in the body. Osteopathy can be a useful addition to acute therapy, but should not be the sole therapy for pain or symptoms that suggest nerve involvement.
You might also be interested in: Osteopathy in cervical spine syndrome
How important is acupuncture?
Acupuncture can also be a useful addition to pain and movement therapy and to surgery after a herniated disc. It originates from traditional Chinese medicine and is used in particular for protracted pain. Targeted needles that are inserted into the skin at certain points are intended to set processes in the body in motion that activate self-healing powers. Even acupuncture should not be the sole treatment for an acute herniated disc with symptoms, as its therapeutic options are limited.
more on the subject "Acupuncture" you'll find here
How long is the total healing time?
The duration of the herniated disc can vary widely and depends on various factors such as the severity of the symptoms, the involvement of other body structures, the choice of therapy method and personal response to the therapy. With a suitable conservative therapy, slight herniated discs can be healed within a few days to a few weeks, or they can be completely symptomatic. In other cases, the nerve involvement can be so severe that complete healing is not achieved and symptoms remain chronic. The therapeutic success of the physiotherapy often sets in within a few weeks, so that a decrease in symptoms is achieved on average after 4-6 weeks.
forecast
Overall that is forecast a herniated disc of the cervical spine Well. For most of those affected, the symptoms and the herniated disc recede with conservative therapy.In the case of advanced symptoms, surgery cannot guarantee that the symptoms will completely regress, but the symptoms can improve.
causes
With age, the intervertebral disc also ages, it loses height and the load capacity of the intervertebral disc decreases. This degeneration of the intervertebral disc can lead to fiber tears in the intervertebral disc, which can then lead to a herniated disc if the load continues. The inner core of the intervertebral disc emerges through the tear of the annulus fibrosus and leads to compression of the nerve root. The tear in the annulus can be in different places, so that the nucleus emerges either to the side (most common shape) or in the middle of the fibrous ring. This subdivision is important because, depending on the type of exit, other symptoms can be observed: A lateral exit leads to compression of the exiting nerve root, while a central exit can result in compression of the spinal cord. The occurrence of a herniated disc due to a single trauma, on the other hand, is rarely observed.
Furthermore, the intervertebral disc is subject to high pressure during life, which can be up to 4 times as high as your own body weight when lifting heavy objects. Since most of the body's weight rests on the lumbar spine (62%), there is greater wear and tear in this area, so a herniated disc is more likely here than on the cervical spine.
At 36%, a large part of the weight also rests on the cervical spine. The thoracic spine only bears about 2% of the weight, so herniated discs are rare here.
The narrowing of the spinal canal can not only come from a herniated disc. In the cervical spine, bony additions to the vertebral bodies are often responsible for the narrowing. The disc between the cervical vertebrae C5 and C6 is most frequently affected in the cervical spine.
Symptoms
Numbness
In addition to the motor part of the nerve root, the part responsible for sensitivity can also be affected by the herniated disc. There is then a feeling of numbness in the skin area that supplies the affected nerve root. When the C6 nerve root is compressed, numbness occurs on the upper arm and on the forearm, pulling the thumb up to the thumb.
Also read: Numbness from a herniated disc
Pain
In addition to motor failures and numbness, pain in the affected area of the arm can also occur.
Disc herniation pain is caused by acute damage to the nerves emerging from the spinal cord. Pressure, irritation, and damage to nerves typically produce tingling sensation, mild numbness, pain later, and finally complete numbness and paralysis. The pain often has a pulling, carrying, and electrifying character. This form of pain is also known as "radicular" pain. Due to the irritation of the nerve root on the spine, the pain is drawn into all supply areas of the affected nerves, although the actual problem is not located there. In the case of a severe herniated disc, the pain can spread to the fingertips or toes.
The cervical vertebrae 5 and 6 are located in the lower area of the cervical spine. Immediately above these vertebrae are the nerves that move the diaphragm and enable breathing. At the level of vertebrae C5 and C6, however, there are motor nerves that supply parts of the shoulder, upper arm and forearm. In the case of failures caused by a herniated disc, the internal rotation of the shoulder, the flexion of the elbow joint and the rotation of the forearm can be restricted. Pain also occurs along these areas and extends from the shoulder over the outside of the arm to the thumb. Typically, the functional restrictions and sensitive failures only occur on one side. Bilateral complaints are rather rare in a herniated disc.
More symptoms
If the herniated disc is located in the middle and compresses not only the nerve root but also the spinal cord, incomplete paraplegic syndromes can be observed: In addition to paralysis of the arms and legs, disorders in the bladder and intestinal area can also be observed. However, this form of herniated disc is rare.
Additional information here: Symptoms of a herniated disc of the cervical spine
Identification muscles
Identifying muscles are those muscles that are only supplied by a corresponding nerve root. If a key muscle fails, it can therefore be precisely determined which nerve root must be restricted. You can therefore deduce the exact amount of the herniated disc. The nerve root C6 emerges from the cervical spine between the cervical vertebrae C5 / C6 and can then be compressed in the event of a herniated disc.
The identification muscles for the C6 nerve root are, on the one hand, the brachioradialis muscle, which is responsible for weak flexion in the elbow joint and the inward and outward rotation of the forearm (Pronation and Supination) responsible is. And on the other hand, the M. biceps brachii, which also causes flexion in the forearm and at the same time acts as the strongest muscle in the outward rotation of the forearm (Supination) applies. Associated reflexes are the radius periosteal reflex and the biceps tendon reflex, which can then also be weakened or even not triggered.
diagnosis
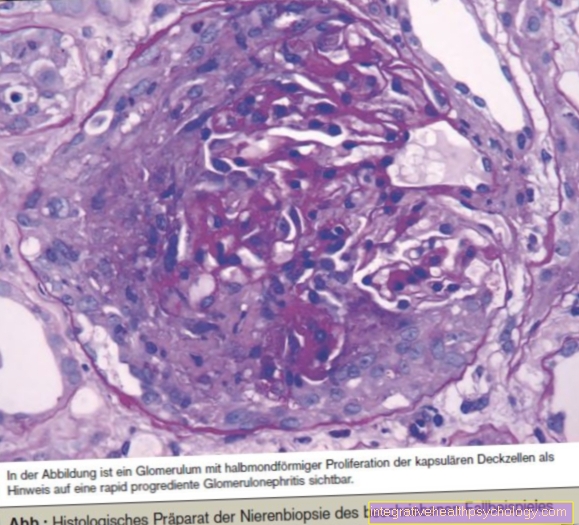
First there is a precise clinical-neurological examination including a strength test, testing of the reflexes and a precise determination of existing paralysis and numbness. If the examination confirms the suspicion of a herniated disc, computed tomography (CT) or magnetic resonance imaging (MRI) can be performed for further diagnosis. MRI is usually preferred, as it is easier to visualize soft tissue and the intervertebral disc. On the other hand, CT can better assess bones and bony attachments. However, an imaging examination is not always necessary. No imaging is required for a conservative therapeutic approach, which is preferred before surgery. Imaging is only mandatory if the symptoms persist, neurological disorders or surgery.
Further information can be found at: Diagnosing a herniated disc