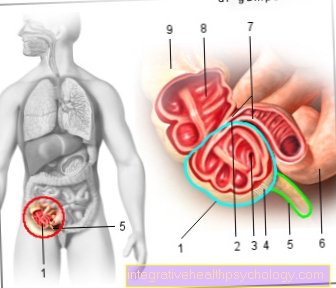
Abscess in the genital area
introduction
An abscess is an encapsulated collection of pus in the tissue that is caused by a local inflammation. Abscesses can form anywhere:
In the mouth or nasal cavity, in the face area (Read about this: Abscess on the face), on the back but also in the anal and genital areas.
Strictly speaking, every blackhead is already a small abscess.
The pus is made up of cells from the human immune system, remnants of dead cells, and bacteria. The body protects itself against further spread of the infection by surrounding the abscess cavity with a capsule.

A abscess can arise in a variety of ways. On the body surface can Bacteria of the normal skin flora, this includes, for example, the so-called Staphylococci, migrate into deeper skin layers through the smallest injuries and multiply there.
Also along the hair germs can penetrate the skin and affect the Hair roots find perfect conditions for their growth. Sebum collects under clogged skin pores, this also provides a breeding ground for bacteria. A pimple develops which, through repeated manipulation, empties into the surrounding tissue and there leads to greater inflammation and Abscess formation can lead.
Causes of an abscess in the genital area
Abscesses tend to develop particularly on warm and humid parts of the body with thick hair and a high density of sebum glands.
This preferably applies to the anal and intimate regions. In the genital area, where many germs naturally settle, abscesses develop primarily on the hair roots.
The risk factors that promote the occurrence of abscesses include smoking and poor personal hygiene, diseases such as diabetes, a weak immune system and skin diseases such as neurodermatitis.
Underwear that is too tight and chafing as well as poorly cared for injuries also increase the likelihood of developing an abscess.
In women, the paired so-called Bartholin's gland can also be the starting point for the formation of large and extremely painful abscesses in the genital area. With such bartholinitis, consultation with a gynecologist and surgical rehabilitation are required.
Read more on the topic: Clogged sebum - what to do?
Abscess in the genital area after shaving
Smallest skin injuries from shaving are a common trigger of abscesses in the genital area. The damaged skin surface allows bacteria to reach deeper layers of the skin, where they can lead to inflammation and even abscesses. The triggering bacteria are mostly staphylococci, which colonize the skin surface even in healthy people without causing damage. Only when they overcome the surface of the skin through small injuries, such as when shaving, can they lead to inflammation and abscesses in the genital area. Overly tight underwear made of non-breathable material, inadequate intimate hygiene, smoking and a weak immune system (e.g. due to cortisone or diabetes) also promote infection and abscess formation. In order to minimize the risk of skin cuts when shaving, care should be taken to always use fresh and sharp razor blades. Shaving foams or gels can also make the razor glide more easily over the skin, so that the risk of injury is reduced. If a cut occurs anyway, the wound should ideally be disinfected and covered; further manipulations should be avoided.
Learn more about how to properly shave your genital area to prevent abscesses from developing: Pubic hair removal with instructions.
Enzyme peels can also help to ensure the purity of the skin and allow the pores to breathe. One example of this is the Dr. Severin enzyme peeling from the pharmacy.
Symptoms of an abscess in the genital area
A skin abscess, as it also occurs in the genital area, is easy to recognize even for the medical layperson. It is a reddened, usually slightly raised area that is painful, whereby the pain intensifies with light pressure on the diseased tissue. In the case of locally advanced findings, the skin in the immediate vicinity feels very warm. Occasionally a white head is visible.
Abscesses usually grow slowly, although after rough and improper manipulation, more brilliant courses with rapid increase in size can be observed.
Read more on this topic at: Abscess symptoms.
Pain from an abscess in the genital area
An abscess in the genital area is usually accompanied by severe pain, which can make sitting and walking very uncomfortable. The pain may be throbbing and worsen when you press or touch it. They are caused on the one hand by the inflammation in the tissue and on the other hand by the tension from the accumulation of pus. Medicines such as ibuprofen, Novalgin or aspirin can be taken against the pain, and even a slight cooling can have a decongestant and pain-relieving effect. A pronounced abscess should also be punctured or cut open, which often brings immediate relief and pain relief.
Differences between men and women
The causes of an abscess in the genital area do not differ significantly between men and women. In both sexes, minor injuries lead to the penetration of bacteria (staphylococci), which cause an abscess through capsule formation. Favorable factors such as smoking, an immunodeficiency, diabetes and poor intimate hygiene have both sexes in common. In both men and women, an abscess is noticeable as a circumscribed, pus-filled swelling. The surrounding skin is often overheated, reddened and very painful.
Only the location of the abscess differs in both sexes. In men, an abscess is often localized in the perineal area, the area between the genitals and the anal region. Painful abscesses can also occur on the scrotum or anal area. In women, on the other hand, an abscess can develop in the area of the labia, especially in the area of the Bartholin gland. The paired Bartholin's gland is located at the rear end of the vaginal outlet and can become infected with various bacteria. The result can be a pronounced, very painful abscess. Abscess formation in the perineum or anal region is also conceivable in women. The treatment of abscesses in the genital area is basically the same for men and women.
Do you have an abscess on your testicle? Learn more about it here: Abscess on the testicle - what are the risks?
Diagnosis of the abscess in the genital area
The doctor can usually diagnose an abscess based on the typical signs of inflammation, redness, warmth, pain and swelling. The typical localization on the face, neck or neck or in the anal and genital areas also helps him to make a diagnosis.
In order to differentiate a large abscess from other diseases, ultrasound diagnostics can help to substantiate the suspicion in individual cases. More rarely, attempts are made to puncture the abscess with a cannula in order to remove pus with a syringe. However, sample material obtained in this way can then be examined microbiologically in order to obtain information about the type of pathogen.
Read more on this topic at: Abscess diagnostics.
Which doctor is responsible for an abscess in the genital area?
If you suspect an abscess in the genital area, the first thing you should do is see your doctor. This can confirm the suspicion and assess the severity of the disease.
As a rule, initial measures such as the prescription of ointments or antibiotics can also be carried out by the general practitioner.
In the case of recurring abscesses or multiple findings at a time, the dermatologist can be consulted to clarify a chronic disease or to optimize the treatment.
Easily accessible superficial abscesses can be opened by the experienced family doctor or dermatologist. A surgeon must be called in for larger or poorly accessible locations.
If the disease affects the genital organs, you should definitely see a gynecologist or urologist.
Therapy of abscess in the genital area
The treatment of an abscess depends on its size and location.
In mild cases, a pull ointment is sufficient. If the abscess is already advanced, the doctor can prescribe a local antibiotic.
If the disease threatens to spread further or if the finding is very large, an antibiotic must be taken.
Surgical intervention may then be necessary. The doctor cuts the abscess under local anesthesia with a scalpel so that the pus can drain away. The resulting wound is then thoroughly cleaned and disinfected.
So that an abscess does not immediately form again in the same place, the doctor will decide not to close the wound first, but rather to insert a drain. This is either a special rubber flap on which newly formed pus can drain off or a gauze tape soaked in an antibacterial solution. The abscess can slowly heal from the depths.
Should you express the abscess?
Under no circumstances should you manipulate an abscess in the genital area yourself. Any opening by means of pointed or sharp objects must be carried out by the doctor, observing strict hygiene measures.
Pushing around on the abscess must also be avoided. There is too great a risk that the abscess capsule will not open on the surface of the skin but into the surrounding tissue. The penetration of the germs in the abscess into the tissue or even into blood vessels can lead to an expansion of the inflammation or, in the worst case, blood poisoning.
Pull ointment / Ilon ointment for an abscess in the genital area
A draft ointment (e.g. Ilon® ointment) is an ointment that primarily promotes blood circulation and has an anti-inflammatory effect on the skin. In addition, it usually has resorption and phagocytosis-promoting properties. This means that foreign substances in the skin are absorbed more quickly by cells of the immune system.
Read more on the topic: Ilon® ointment
Draw ointments are mostly made from oil shale and, more rarely, on a plant basis. The most commonly used active ingredient is that made from oil shale Ammonium bituminous sulfonate.
A pulling ointment essentially contributes to the faster maturation of the abscess, so that it can be opened on the body surface or emptied by itself.
In order to intensify the effect of the ointment, the application of heat can additionally support the abscess maturation.
Possible areas of application of a pulling ointment are abscesses in the genital area as well as those that are found in other parts of the skin or in the context of the Acne conglobata have formed.
Infected foreign bodies such as thorns or splinters that have penetrated the skin can also be transported to the surface of the skin more quickly by using a pulling ointment.
Applying a pull ointment is easy. The affected skin area is generously smeared with the ointment and covered with a plaster. Contact of an oil-slate-based ointment with clothing or other textiles should be avoided as stubborn stains can form.
Although pull ointments are freely available in pharmacies, consultation with the attending physician should be made before use. If the skin is irritated or severely damaged, an ointment should not be used.
It should also be noted that during the application an apparent worsening of the clinical picture can initially occur, since the abscess can swell as it matures and appears reddened.
Betaisodona for an abscess in the genital area
The Betaisodona ointment must be distinguished from the pull ointments. This is an antiseptic ointment based on iodine, which is used for open wounds and ulcers, especially for pressure sores or leg ulcers (ulcus cruris).
In addition to being used for inflammation of the nail bed, it can also be used in the context of infections of the oral cavity or fungal infections of the vagina.
In the treatment of abscesses, betaisodona ointment can be used as antiseptic (germicidal agent) can be used after opening them.
The type of application is similar to that of the pull ointment. The very tough betaisodona ointment is applied to the affected area of the skin and carefully covered with a plaster due to the possible formation of stains on textiles
Find out more about the topic here:
- Betaisodona® ointment
- Betaisodona® solution
- Betaisodona
Home remedies for an abscess in the genital area
In the case of small, easily accessible and superficial abscesses, the application of heat can accelerate maturation and contribute to faster emptying of the skin surface.
Sacks with hot porridge made from oat groats or linseed are suitable for this. Hot porridge made from fenugreek seeds spread on a gauze bandage and applied for about 20 minutes has a similar effect.
Warm onion slices or garlic have a circulation-promoting effect due to the heat effect and the essential oils they contain and are suitable for supporting abscess maturation.
Chamomile has antiseptic properties, so a compress soaked in chamomile tea can be used after the spontaneous opening of an abscess.
Nettle tea and daisy tincture can accelerate the healing process and are to be used locally on a suitable carrier such as cotton or gauze.
Read more on this topic at: Home remedies for an abscess
forecast
Becomes a abscess is recognized and treated in time Good prognosis. With professional therapy, healing usually occurs quickly and without complications.
However, abscesses, especially those in the genital area, tend to return. If this is the case, further examinations should be initiated by the family doctor Precautionary measures be seized.
Duration of healing
If an abscess in the genital area is adequately treated early on, it will usually heal without consequences. If, on the other hand, there is no treatment, the spontaneous course can extend over weeks, as the pathogen is protected by a capsule and thus escapes the body's defense system. In the worst case, the pathogen can spread via the bloodstream and thus lead to blood poisoning (sepsis). Antibiotics, which should always be used in the case of an abscess, usually achieve a significant improvement after 3 to 5 days at the latest. If there is no improvement or if the finding is pronounced, an operative procedure is also appropriate. Immediate relief is achieved by puncturing or cutting open the abscess, and the supportive administration of antibiotics should allow the abscess to heal completely within a few weeks.
prophylaxis
To step Abscesses in the genital area often on, that can be a sign of a weakened immune system or one Diabetes disease be.
The family doctor can carry out targeted examinations and advise those affected accordingly. Generally applies to healthy eating pay attention to strengthen the body's defenses.
The consistent compliance with hygiene measures, In particular regular intimate hygiene can prevent the development of abscesses as well as avoiding too tight-fitting and abrasive underwear.
Is an abscess in the genital area contagious?
An abscess in the genital area is often caused by staphylococci, which colonize the skin surface even in healthy people without causing discomfort.Intestinal bacteria such as E.coli, which can be found in the intestine of healthy people, are also conceivable as triggers for abscesses in the intimate area. Both species can e.g. are transmitted to the partner during sexual intercourse, but usually do not cause any damage, but colonize the skin peacefully. Only when they overcome the surface of the skin through small skin injuries can they cause skin infections and abscesses.


















.jpg)