ACE inhibitors
Synonyms in a broader sense
Angiotensin converting enzyme inhibitors
definition
This group of drugs comes mainly from used in the treatment of high blood pressure (arterial hypertension). Taking ACE inhibitors reduces the incidence of cardiovascular disease and lowers the mortality rate from high blood pressure.
application areas
ACE inhibitors are primarily used in 3 indications, these are:
- High blood pressure (hypertension)
- Heart failure (heart failure)
- Heart attack and stroke prophylaxis.

How ACE inhibitors work
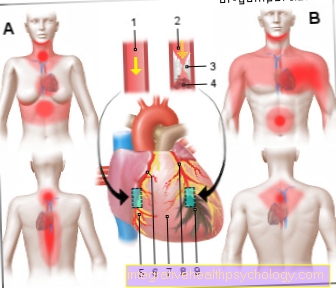
The Renin-Angiotensin System, abbreviated RAAS, is used to regulate blood pressure by producing certain hormones.
Does the Blood pressure or if the blood volume decreases, the system reacts by releasing Renin into the blood. Renin is a protein that makes the hormone Angiotensinogen activated. The activated angiotensinogen is then called Angiotensin 1.
A protein called a name acts on this hormone ACE (English: A.ngiotensinC.onverting-E.nzyme), which produces the hormone angiotensin 2.
Angiotensin 2 causes a general activation of the stress-mediating nervous system, this in turn leads to blood vessel constriction and an increase in blood pressure. Irrespective of the nervous system, the hormone leads to a constriction directly in the vessels, which also leads to an increase in blood pressure. In addition, more aldosterone is released into the bloodstream. The body holds more thanks to the aldosterone sodium and thus more water back, the blood volume and blood pressure rise.
The ACE inhibitors intervene in this finely tuned system of blood pressure control: ACE inhibitors block the action of the protein called ACE, so that less angiotensin 2 is formed.
The effect of the blockade is to lower the blood pressure, because less angiotensin 2 leads to vasodilation. In addition, the release of aldosterone decreases so that less fluid is retained in the body and the heart has less volume to pump. The lowering of blood pressure is greater, the more active it is Renin-Angiotensin-Aldosterone System and thus the higher the blood pressure before treatment.
How exactly do the ACE inhibitors work?
The effect of this class of drugs is in the Lowering the vascular resistance, which contributes significantly to the level of blood pressure. The vascular resistance is the pressure that the vascular system applies to the heart.
The mechanism of action of ACE inhibitors is that decreased formation of
Angiotensin 2, a hormone that causes blood vessels to constrict. This lowers blood pressure by preventing the blood vessels from narrowing.
In addition, the breakdown of vasodilating hormones, the Kininen, inhibitedso that in addition to the above mechanism, vasodilation is promoted.
Another effect of the ACE inhibitors is to lower blood pressure:
Angiotensin 2 leads to the release of Aldosterone, which holds back sodium (part of table salt) and water in the body and thus increases the amount of fluid in the vascular system. ACE inhibitors, on the other hand, reduce the amount of aldosterone in the body, which results in a lower volume in the vessels and thus lower blood pressure.
ACE inhibitors also protect the heart from the effects of stress hormones, which increase blood pressure and the heart's oxygen consumption.
When are ACE inhibitors prescribed?
ACE inhibitors are valuable drugs in the therapy of high blood pressure.
The Combination of an ACE inhibitor with a diuretic is recommended because an additional increase in effectiveness can be achieved and better blood pressure values can be set. It is important that the patient is informed that in the first phase of therapy, drug side effects such as Fatigue and exhaustion occur, but mostly disappear again in the course of therapy and as the body gets used to lower blood pressure values.
Patients with a functional impairment of the heart, the so-called heart failure, preferably receive ACE inhibitors, as these have a protective and relieving effect on the heart. The course of the disease in this group of patients can be positively influenced.
The recommendation for the administration of ACE inhibitors also exists for the follow-up treatment of patients with Heart attack as well as for diabetes patients in whom as a result of Diabetes kidney dysfunction (diabetic nephropathy) is present:
Modifications on Heartthat take place after a heart attack or with high blood pressure can be inhibited by the medication, so that e.g. a thickening of the Heart muscles regresses.
In diabetics with kidney damage, the ACE inhibitors prevent the rapid progress of the kidney disease and reduce the excretion of proteins.
Diabetics also benefit from therapy with ACE inhibitors in that the drug group has a beneficial effect on the fat and sugar metabolism in the sense of lowering sugar and fat values.
ACE inhibitors group of drugs
The ACE inhibitors include the following active ingredients with the corresponding trade names of the preparations. The trade names are the names of the pharmaceutical companies for their preparations with a special active ingredient from the group of ACE inhibitors.
ACE inhibitors drug group and their trade names
- Benazepril, e.g. Cibacen®, Benzepril Hexal®, Benazepril Beta®
- Captopril, e.g. Coronorm®, Lopirin®, Ace inhibitor ratio. ®, Adocor ®, Captohexal ®, Core tensobon ®, Jucapt ®
- Cilazapril, Dynorm®
- Enalapril, e.g. Enadura®, Xanef®, Corvo®, Benalapril®, Enadura®, Jutaxan®, Enahexal®, Enalapril-ratio®
- Fosinopril, e.g. Dynacil®, Fosinorm®, Fosinopril Basics®, Fosinorm®, Fosino Teva®
- Imidapril, Tanatril®
- Lisinopril, e.g. Acerbon®, Coric®, Acerbon®, Coric®, Lisidigal®, Lisidura®, Lisihexal®, Lisigamma®
- Moexipril, Fempress®
- Perindopril, e.g. Coversum®
- Quinapril, e.g. Accupro®, Quinapril Beta®, Quniapril Hexal®, Quinapril Stada®
- Ramipril, e.g. Delix®, Ramicard®, Delix®, Rami-Q®, Ramicard®, Vesdil®, Ramipril-Ratio. ®, Ramipril Hexal ®
- Spirapril, Quadropril®
- Trandolapril, Udrik®
Combination treatment of high blood pressure
ACE inhibitors can be used as so-called monotherapeutic agents, which means that the ACE inhibitor is the only drug used to lower high blood pressure.
The following dual combinations, consisting of an ACE inhibitor and another drug, are recommended for high blood pressure: ACE inhibitor and calcium channel blocker, ACE inhibitor and diuretic.
Calcium antagonists lower blood pressure by acting on the blood vessels in the sense of vasodilation and also affect the heart in part. A diuretic is a drug used to increase the amount of water excreted in the urine. This group of drugs is often referred to as "water tablets".
If none of the two-fold combinations is effective, a triple combination can be prescribed. This can consist of:
Diuretic and ACE inhibitor and angiotensin-2 antagonist, diuretic and ACE inhibitor and calcium channel blocker.
Angiotensin-2 antagonist is a drug whose effects are similar to that of ACE inhibitors:
It influences the RAAS and lowers blood pressure through vasodilation and reduced water retention in the body.
Side effects of ACE inhibitors
At the beginning of the therapy there may be a sharp drop in blood pressure with dizziness, which is why a low starting dose is recommended. If there is a sharp drop in blood pressure, the patient is given fluids via the vein (infusions) and his upper body is laid flat, while the legs are raised so that more blood can flow back into the upper half of the body.
The typical side effects of ACE inhibitors are dry, irritating cough in 10-15% of patients. When taking ACE inhibitors, potassium, a blood salt, increases because less aldosterone is formed, which is responsible for the excretion of potassium. What is known as angioneurotic edema can also occur: the lips and oral mucosa can swell.
Less common side effects are allergic skin reactions, a decrease in red blood cells (anemia) or white blood cells (leukopenia).
Since the drug is eliminated from the body in the urine through the kidneys, it is possible that kidney function may deteriorate. This side effect occurs mainly in patients who are through arteriosclerosis have damaged kidney vessels.
to cough
One of the main side effects from the ACE inhibitors is dry cough. This can be explained by the functions of the Angiotensin converting enzyme. In addition to the function of converting angiotensin 1 to angiotensin 2, it also has a so-called function Kinase function. This means that the enzyme also breaks down tissue hormones, the so-called kinins, such as bradykinin and substance P. These tissue hormones play an important role in inflammation. Together with other natural factors in the body, they cause blood vessels to dilate. This is important in inflammatory situations so that the immune cells can gain access to the diseased tissue. In addition, they ensure pain awareness. These functions are normally adequately regulated by the angiotensin converting enzymes as they break down tissue hormones. The breakdown of bradykinin and substance P is inhibited by the ACE inhibitors. This means that the tissue hormones are increasingly available. The advantage is that, in addition to the antihypertensive effects of ACE inhibitors, the blood vessels dilate. This in turn reduces blood pressure.
Also read: Bradykinin
The disadvantage is that these tissue hormones can trigger symptoms of inflammation. They can irritate nerve endings by sensitizing them to pain. In the context of treatment with ACE inhibitors, they prefer to do this in the throat. In addition, increased potassium levels caused by the ACE inhibitors can intensify these processes.This can lead to a dry cough, which can develop into other more threatening symptoms. The vascular hormones can also cause edema. This mainly happens in parts of the body where there is a lot of cancellous tissue. This is the case in the neck area. This can lead to edema from the ACE inhibitors. There is thus a risk of a life threatening Angioedema developed. Therefore, the side effect of irritable cough must be taken very seriously. In some patients, the dry cough appears right at the beginning of therapy, while in other patients it is noticeable several weeks after the start of treatment. If a dry cough is noticed, the doctor should be informed immediately. Life threatening situations are rare but can occur. These can be avoided by acting early. Usually, this is followed by a switch to another drug to lower blood pressure, a so-called angiotensin 2 receptor blocker.
For more information, see: cough
Hyperlipidemia - increased blood lipids
Colloquially, hyperlipidemia corresponds to an increase in blood lipids. These play a role in high blood pressure and thus also in treatment with antihypertensive drugs such as ACE inhibitors. Both high blood pressure and increased blood lipids increase the risk of developing hardening of the arteries. In turn, hardening of the arteries increases the risk of developing heart and vascular diseases. These are among the most common causes of death in Germany. Various measures and medication are used to try to lower these risk factors. However, some measures and medications result in one risk factor being lowered while another is increased. There are various antihypertensive drugs that increase blood lipids - that is, one Hyperlipidemia being able to lead. As far as we know today, the ACE inhibitors are not included. This means that the risk of developing or exacerbating hyperlipidemia with ACE inhibitors is lower than with many other antihypertensive drugs.
Drug interactions
The antihypertensive effects of ACE inhibitors can be achieved by simultaneous treatment with other Blood pressure medication be reinforced.
This can be used for treating the high blood pressure be very positive, because the combined administration of additional medication can achieve an effective and permanent lowering of blood pressure.
Potassium-sparing diuretics
Due to the increased reabsorption of potassium, also through the ACE inhibitors in the kidney, the potassium level in the blood rise threateningly.
Insulin / oral anti-diabetic drugs
The effect of antihypertensive agents can be increased.
Cytostatics, immunosuppressants, glucocorticoids
Are all drugs that influence or suppress the immune system and thus greatly change the blood count, this blood picture-changing effect can be in combination with ACE inhibitors be reinforced.
ACE inhibitors and alcohol - are they compatible?
It is advised not to consume alcohol during treatment with ACE inhibitors. The main reason for this is the unpredictable effects on blood pressure and its consequences. A distinction must be made between the short-term and long-term effects of alcohol on blood pressure. Alcohol can cause blood vessels to widen in the short term. This may cause a drop in blood pressure. The ACE inhibitors also lower blood pressure. When this antihypertensive effect adds up, it can lead to mild to severe circulatory problems. Prolonged alcohol consumption can increase blood pressure. Individual factors play a role here, whether and to what extent this happens. If there is additional smoking or psychological stress and anger are present, the increase in blood pressure with alcohol consumption can increase further. Often the blood pressure increasing effects are permanently stronger than the blood pressure lowering effects of alcohol. Drinking alcohol would reduce the effect of the ACE inhibitors or make them largely ineffective. That could have fatal consequences. The risk of diseases associated with high blood pressure would increase enormously. This means that the risk of diseases that the ACE inhibitor is supposed to protect against, such as strokes and heart attacks, would increase.
Note: lowering blood pressure
It is therefore very important that the patient informs the attending physician of all medications that he takes regularly. This is because a sharp drop in blood pressure can occur if several drugs with antihypertensive effects are taken that are not coordinated with one another. Drugs that lower blood pressure include Beta-lockers, diuretics, sedatives, antidepressants, and alcohol.
Contraindications
The pregnancy and breast feeding period represent contraindications for the use of ACE inhibitors. Contraindications are circumstances that prohibit the use of the drug.
- Patients with narrowing of the renal artery (renal artery stenosis)
- Patients with only one kidney
- such with Liver dysfunction
or - a narrowing of the main artery (Aortic stenosis) must not take ACE inhibitors.
- Also, this group of drugs should not be used when the volume is reduced Vascular system or an increase in blood potassium before starting treatment.
forecast
ACE inhibitors are used in the treatment of high blood pressure, cardiac impairment, after a heart attack and in diabetics with kidney disease (diabetic nephropathy) and here they reduce patient mortality. The regression of structural changes in the heart after a heart attack and in diabetic nephropathy can be achieved with ACE inhibitors and thus improve the health prognosis of those affected.
What should be considered when stopping?The procedure for discontinuing ACE inhibitors is controversial. Some authors report that, for example Ramipril, an active ingredient from the group of ACE inhibitors, does not cause blood pressure to rise on discontinuation. They report that the so-called rebound phenomenon would not occur with this active ingredient. Discontinuing the drug would therefore be problem-free in consultation with the doctor. Gradual dosing would therefore not be necessary. Other authors strongly advise against discontinuing ACE inhibitors abruptly. According to these voices, switching to another antihypertensive drug can sometimes be useful. But sudden discontinuation increases the risk of complications that could be fatal. Nevertheless, patients often stop taking the drug on their own. This is mostly due to insufficient information and / or understanding. Patients are often symptom-free before taking the ACE inhibitor. If they then take the medication, it can cause symptoms such as dizziness. This has to do with the fact that the body has got used to the high blood pressure values. A (sudden) decrease causes discomfort. Therefore, it is only natural that this stimulates withdrawal from the drug.
When stopping, however, one should note that permanently high blood pressure values increase the risk of diseases such as stroke and heart attack enormously. As a rule of thumb, it is stated that an increase in blood pressure of 10 mmHg would cost 10 years of life. This means that even a symptom-free, permanent increase in blood pressure can be life-shortening. If the blood pressure lowering can be achieved with the ACE inhibitors, it does not mean that these values will stay that way on discontinuation. In most cases, stopping the antihypertensive drugs would raise blood pressure again. However, this also depends on what caused the increased blood pressure. It is advisable to consult your doctor. In most cases, an individually tailored, adequately creeping and, if necessary, gradually increasing therapy with ACE inhibitors appears to be effective.















.jpg)