Achilles tendon rupture
synonym
Achilles tendon tear
Tasks / anatomy
The Achilles tendon is the tendon of the Triceps surae muscle on the calcaneus.
The task of the muscle or the tendons is to pull the heel up and thus lower the foot.
This movement is essential when running and walking.
The Achilles tendon is the strongest tendon in the human body. It has a length of 10-12 cm and a diameter of 0.5-1 cm.
definition
Under one Achilles tendon rupture one understands a tear, caused by a traumatic or atraumatic event, or tear of the Achilles tendon adjoining the calf.

Causes / forms
In the case of Achilles tendon ruptures, a distinction is made between traumatic and atraumatic ruptures.
Traumatic ruptures:
Most of the traumatic ruptures are sports accidents and injuries. In some cases, the tendon tears or tears during normal running and walking in everyday life.
Most of the time there is a traumatic Achilles tendon rupture sudden stopping motion in which there is a sudden pull on the Achilles tendon.
In everyday life, a rupture can occur when walking downhill or when kinking the foot.
In the field of sports, such injuries usually occur in the many ball sports.
Here ball sports are particularly affected, where speed and often changing directions and speeds are required. To be mentioned here are e.g. Tennis or table tennis and basketball. Achilles tendon ruptures are relatively rare in hand or soccer ball games and are usually associated with kicks by the opponent in the area of the Achilles tendon.
The causes of traumatic Achilles tendon ruptures are a tensile or sudden increase in pressure or overstretching of the ankle. The Achilles tendon can then no longer withstand the load despite its stability and tears. It is often the case that torn tendons are already damaged and thinned out, so that a minor trauma is necessary to cause the tendon to tear.
Atraumatic ruptures:
The atraumatic rupture does not result in an accident, but in a sudden, unexpected tear and tear of the Achilles tendon. The atraumatic rupture occurs in all cases Previous damage are based or are degenerative processes available.
Even the atraumatic rupture does not just happen, but rather during movements that stress the Achilles tendon. Stopping (including light stopping) or going downhill can rupture the tendon.
The Achilles tendon ruptures are also divided into complete ruptureswith a tear about 2-6 cm above the heel bone and the less common partial tear.
Complete avulsions occur very rarely directly on the heel bone.
Appointment with an expert in Achilles tendonitis?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
Athletes (joggers, soccer players, etc.) are particularly often affected by the Achilles tendonitis disease. In many cases, the cause of the Achilles tendonitis cannot be identified at first. Therefore, the treatment requires a lot of experience. I focus on Achilles tendonitis.
The aim of every treatment is treatment without surgery with a complete recovery of performance.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Risk factors
There are numerous risk factorsthat can promote an Achilles tendon rupture.
Besides the chronic overload, in which the tendon is already damaged and the smallest, invisible cracks reduce the stability of the tendon, this is what counts gout (Increase in the level of uric acid in the blood) and the Rheumatoid arthritis a risk factor for an Achilles tendon rupture.
There are also drugs that can make the Achilles tendon more prone to rupture. The long-term use of Cortisone on the one hand, but also immunosuppressive drugs lead to an increased tearability of the tendon.
Also some Antibiotics the risk of Achilles tendon rupture is ascribed. Above all, antibiotics from the group of gyrase inhibitors should be mentioned here.
The drug causes are rare compared to the traumatic causes.
Symptoms
A complete rupture of the Achilles tendon often results in a loud whip-like noise described, which is based on the very tight Achilles tendon tearing and buckling upwards.
During the tear will also be strong pain described, but then quickly fade away again.
Above the tendon attachment point, there is usually a palpable dent due to the fact that the muscle is also buzzing together.
A short time after the rupture, it can become one swelling (edema) come.
It can also be used for Hemorrhage in the area of the tear come that through one Hematoma becomes visible.
After the rupture they are Movement impairments leading as a symptom. In most cases, the foot can no longer be bent downwards. Raising the foot, on the other hand, usually does not cause any problems.
diagnosis
A visual diagnosis is often enough to diagnose an Achilles tendon rupture.
Classic impairment of movement and a typical dent above the point of attachment often indicate an Achilles tendon rupture.
The patient is always asked about the event that took place and whether there was a whip-like noise.
The physical examination consists of palpation and passive and active movement of the foot.
The so-called Thompson test the calf is compressed while the patient is lying down. If the foot does not move as a result, an Achilles tendon rupture is likely.
The Ultrasonic first of all. A gap in the Achilles tendon can be seen, which corresponds to a rupture. In some cases an additional MRI of the Achilles tendon may be necessary to better assess the injury.
therapy
Today one is becoming more and more common conservative therapy applied.
It consists of one Immobilization of the leg in equinus position. This is usually done with a special shoe.
The prerequisite is that the tendon ends lie against each other and thus have the chance to grow together.
The immobilization should take place 24 hours a day for 6 weeks, then a further 2 weeks with a wearing time of approx. 12 hours a day.
A operative care was almost always carried out in the past. Today there is rarely an indication for this. During the operations, the tissue is opened up on the side of the Achilles tendon, the two tendon attachments are placed together and sutured again. After an operation, the foot is immobilized for a long time using a cast or special shoe.
Occurrence
Men are about 5 times more likely to be affected than women.
The main age of a rupture is between the ages of 30 and 50 and then again over the age of 50.
Approx. 20 people per 100,000 population suffer an Achilles tendon rupture each year.
Summary
A Achilles tendon rupture can either be traumatic e.g. after a sports accident (sudden stopping) or atraumatically (mostly due to degeneration).
The typical symptoms are
- whip-like buckles
- Hematomas
- Pain
- Swelling
- Movement impairments (the foot can no longer be brought into the equinus position).
A rupture is diagnosed by questioning (whip-like noise), examination (impaired movement) and by imaging using ultrasound (free area at the tendon site indicates a rupture)
Therapy is almost exclusively conservative today (immobilization of the foot in a pointed position in a special shoe for 6 weeks 24 hours, then for 2 months 12 hours, followed by training.
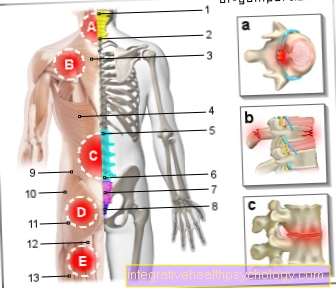
Figure pain ankle

Foot pain
- Achilles tendonitis /
Achilles tendon rupture - Broken bones - toes,
Metatarsus, tarsus
(here outer ankle fracture) - Ligament stretch / torn ligament
at the ankle - Lower and upper heel spurs
Calcaneus spur - Hammer toe and claw toe
(Deformities of the toe bones)
Digitus malleus - Plantar warts
Verrucae plantares - Hallux valgus -
(Deviation of the big toe
in the base joint) - Hallux rigidus -
(Joint wear of the
Metatarsophalangeal joint) - Inflamed nails / nail fungus
- Osteoarthritis / arthritis -
degenerative change of
Joints / inflammation of the joints
You can find an overview of all Dr-Gumpert images at: medical illustrations