Antibody therapy
What is Antibody Therapy?
Antibodies are protein molecules made by the B cells in the human body.
They play an important role in the immune system, as they mark invasive pathogens or damaged endogenous structures and can thus lead to elimination by other defense cells.
The specific recognition site to which the antibody binds is called an antigen.
Each antibody usually only recognizes a single antigen.
But not only pathogens or damaged endogenous structures carry antigens: some cancer cells also have tumor antigens on their surface and can therefore be marked for degradation by antibodies.
Antibody therapy makes use of these properties of antibodies.
In the laboratory, cells are grown that produce a certain type of antibody that is specific for an antigen.
If, for example, an antibody is produced that binds to an antigen that is specific for a certain type of cancer, then there is a good chance that the antibodies can be used to effectively treat the disease.
Read more about the topic under: Antibodies
What diseases is antibody therapy used against?
The two most important groups of diseases for which antibody therapy is used are cancer and autoimmune diseases.
Cancer therapy with the aid of antibodies takes advantage of the fact that many cancer cells have very specific molecules on their surface that healthy cells in the body do not have.
Subjecting the patient to therapy with an antibody that specifically recognizes these antigens is a promising approach for improving the course of the disease without significant side effects (since the antibody “leaves the healthy cells alone”).
Read more on the subject at:
- Tumor diseases
- Autoimmune Diseases- What is it?
How can you tell if you are eligible for antibody therapy?
In order to determine whether you are suitable for antibody therapy, you should of course first find out whether specific antibodies exist at all for the disease you are suffering from. If it is a cancer or autoimmune disease, the chance is high.
Particularly in the case of cancer, however, detailed medical and laboratory technical information may be required to identify the exact type of cancer (the expert speaks of a cancer entity) and thus to find out whether a suitable antibody therapy exists.
Once this first step has been taken and it has been established that specific antibodies are available that promise an improvement in the course of the disease or even a cure, it must be weighed whether your body would allow this antibody to be used.
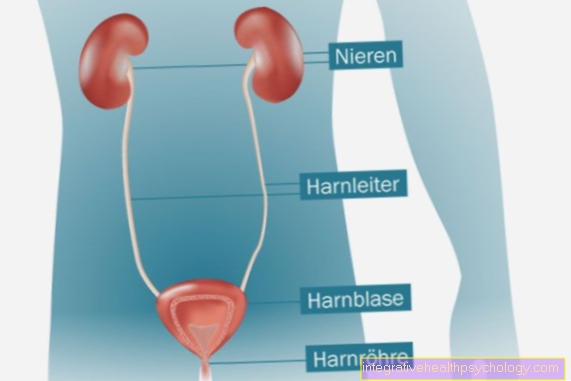
Each antibody has its own side effect profile. An example: You have had kidney damage for a long time and recently developed cancer.
There is a specific antibody for the type of cancer you have, but this often causes side effects in the form of impaired kidney function.
In such a case, a thorough risk-benefit analysis should be carried out with the treating doctor before deciding on antibody therapy.
The central question: does antibody therapy offer such good prospects for an improvement in cancer that a further deterioration in kidney function can be accepted?
In addition, there are special step schemes for the treatment of many diseases. This means that different therapy methods are used depending on the stage of the disease. These schemes are based on many years of experience and studies on the best possible individual treatment method.
On the basis of these schemes, it is possible that there is a specific antibody therapy for your disease, but this is not used at the stage of the disease in you.
If this is the case for you, your doctor has usually not forgotten about the antibody therapy, but has decided on a different form of treatment based on the scheme.
The therapy
If the decision for antibody therapy has been made in connection with an illness, a few preliminary examinations must first be carried out. These should rule out health problems that would speak against the implementation of the antibody therapy.
The antibodies are given in the form of syringes or infusions, often in combination with drugs to prevent an allergic reaction.
If the therapy takes the form of injections (i.e. syringes), this can also be carried out independently by the patient at home. The administration takes place several times and, depending on the disease and depending on the antibody, at intervals of one or more weeks.
According to the patient's state of health and the side effect profile of the antibody, controls are carried out at the individual appointments to monitor the body's reaction to the therapy and the occurrence of side effects.
Find out about the individual antibodies that are used for therapy: Biologics
The duration of antibody therapy
The duration of antibody therapy varies depending on the disease to be treated, the antibodies used and the course of the disease under the therapy.
Sometimes it is only a few months, while the treatment of breast cancer with trastuzumab is designed for one to two years. The duration of the individual appointments is also very variable, depending on the antibody used and the type of application: While injections (syringes) are done very quickly, infusions can take several hours. In the latter case, you should take some activity with you to pass the time.
What are the side effects?
Depending on which disease is treated with antibody therapy and which antibodies are used, various side effects can occur.
Especially in the initial phase of treatment, for example, symptoms that resemble those of a flu-like infection can occur, such as fever, fatigue or aching limbs.
application areas
For breast cancer
The antibody trastuzumab (trade name Herceptin®) has been approved for the treatment of breast cancer in the early stages for several years.
Trastuzumab binds to HER2 / neu, a molecule on the surface of breast cells.
This molecule is only present in small numbers in healthy female breasts and regulates cell growth. “Degenerate” mammary gland cells, i.e. breast cancer cells, have a much higher number of HER2 / neu molecules on their surface in around 20-25% of cases; this is referred to as overexpression.
This leads to uncontrolled growth of the tumor. By binding to the HER2 / neu molecule, trastuzumab prevents its growth-promoting effect and marks the breast cancer cell for the body's own immune system. This initially leads to a blockade of tumor growth and then to a defense reaction of the body against the tumor.
To find out whether antibody therapy with trastuzumab is even an option for a breast cancer patient, the HER2 / neu status of the tumor must first be determined.
This means nothing else than examining whether the tumor actually has an above-average number of HER2 / neu molecules on its surface, because only then does therapy with trastuzumab make sense.
The simplest procedure for this consists of removing a tiny piece of tissue from the tumor (biopsy) and then staining it, which makes the HER2 / neu molecules visible.
The more molecules there are, the stronger the color reaction, so that the result can be expressed in the form of a scale. 0 and 1 stand for a non-excessive presence of HER2 / neu, while 3 means that trastuzumab therapy is an option.
If the value is 2, a genetic test (FISH) must be carried out in order to clarify whether trastuzumab therapy makes sense. However, this does not mean that trastuzumab therapy is unreservedly recommended for all patients with overexpression of HER2 / neu; Other factors such as the extent of the disease or existing secondary diseases play an important role (for example, an unrestricted pumping function of the heart is a prerequisite for the use of trastuzumab), so that a decision about trastuzumab therapy should always be made on the basis of an individual assessment by a specialist.
Trastuzumab is given as an infusion with the first infusion taking about 90 minutes and about 30 minutes each subsequent infusion. The infusions take place either weekly or every 3 weeks. As a rule, antibody therapy is not viewed as an alternative to chemotherapy, but rather as a supplement:
The surgical removal of the tumor is followed by chemotherapy and then antibody therapy at an interval of about 3 months.
The antibody bevacizumab (Avastin®) is used to treat advanced breast cancer.
The antibody prevents the effect of VEGF, a growth factor for the formation of new blood vessels in tumors, and thereby practically “starves” the tumor.
It is used in advanced breast cancer patients to inhibit the growth of metastases, in conjunction with the chemotherapy drug paclitaxel.
Cetuximab, pertuzumab and denosumab are currently in the final phase of clinical trials and could be included in the therapy regimes for the treatment of breast cancer in the coming years.
Read more on the subject at:
- Chemotherapy substances
- Breast cancer therapy
For lung cancer
The antibodies atezolizumab and nivolumab represent a new, promising option for the treatment of lung cancer.
The antibodies bind to a specific surface molecule of lung cancer cells and mark these cells for degradation by the body's own defense cells. It should be noted that antibody therapy with acetolizumab or nivolumab is not suitable for all cases of lung cancer: So far, the indication (area of application) has been limited to advanced and / or metastatic non-small cell lung cancer (NSCLC), i.e. to late stages of a certain type of lung cancer.
Both antibodies are given as an infusion.
Read more on the subject at: Lung cancer therapy
With a lyphoma
The term lymphoma encompasses a huge spectrum of different malignant diseases of the lymphatic system and just as many different therapeutic strategies.
There are currently three antibodies that are approved for the treatment of some types of lymphoma from the non-Hodgkin lymphoma category:
Rituximab, obinutuzumab, and ofatumumab.
All three antibodies develop their effect by docking onto the CD20 molecule on the surface of the lymphoma cells, whereby the cells are marked for breakdown by defense cells.
Rituximab is used to treat follicular lymphoma and diffuse large B-cell lymphoma. It is used either alone or in combination with chemotherapy as part of the R-CHOP scheme (the R stands for rituximab and CHOP for the first letters of the chemotherapeutic agents used). Obinutuzumab and ofatumumab are used in chronic lymphocytic leukemia, which is also a subtype of non-Hodgkin lymphoma, and in follicular lymphoma.
The prerequisite for antibody therapy with one of the antibodies is not only the assignment of the lymphoma to one of the two classes mentioned, but also the biotechnological detection of the CD20 molecule on the cells of the tumor. For this purpose, a tissue removal (biopsy) must be carried out.
Read more on the subject at:
- Therapy for lymphoma
- Hodgkin lymphoma
For colon cancer
For advanced colorectal cancer, intravenous (i.e., infused) antibody therapy with cetuximab or panitumumab may be an option.
Both substances block the binding site of the growth factor EGF on the surface of the cancer cells and thereby stop tumor growth.
The antibodies can either be given directly as a supplement to the standard therapy according to the FOLFOX or FOLFIRI regimen or alone after the standard therapy if this has not shown sufficient success.
The prerequisite for the administration of cetuximab or panitumumab is firstly the presence of the EGF binding site on the cancer cells (this is the case in> 90% of colon cancer cases) and secondly the absence of a K-Ras mutation.
This mutation makes cetuximab and panitumumab practically ineffective, so that such a mutation must be ruled out before starting therapy with these antibodies.
Antibody therapy can usually be carried out on an outpatient basis, with weekly (cetuximab) or 14-day (panitumumab) infusions, each of which takes about half an hour to two hours.
Therapy will continue as long as it is effective and does not have excessive side effects.
An alternative to the treatment of advanced colorectal cancer with metastases is the antibody bevacizumab. This is directed against the vascular growth factor VEGF, thereby inhibiting the vascular growth of the tumor and "starving" it out.
Bevacizumab is administered as an infusion and mostly in combination with chemotherapy in the form of 5-fluorouracil.
Read more about this: Colon cancer therapy
For stomach cancer
In the case of advanced gastric cancer, antibody therapy may be an option.
This option is usually chosen when the cancer has progressed to the point that surgery is no longer possible, or when chemotherapy and radiation have not shown sufficient results. The antibodies trastuzumab and ramucirumab are approved for this application.
Trastuzumab stops cancer cells from growing and is used in combination with chemotherapy for metastatic gastric cancer. It is given as an infusion every three weeks and therapy can be continued as long as the drug is effective.
However, this antibody is only effective in the part of gastric cancer patients whose tumor cells have the specific target molecule of the antibody on their surface.
This must be clarified before starting trastuzumab therapy with the help of a tissue removal (biopsy). Another aspect that can make the use of trastuzumab impossible is the presence of heart damage. This will also be checked before starting therapy.
Ramucirumab acts against the vascular growth factor VEGF. This inhibits the formation of blood vessels in the tumor and "starves" the tumor.
The antibody can be administered in combination with a chemotherapeutic agent. The administration takes place in the form of regular infusions at two-week intervals and is continued as long as it is effective.
Read more on the subject at: Stomach cancer
Crohn's disease
Antibody therapy can be considered in patients with Crohn's disease if the standard therapy with cortisone preparations, aminosalicylates (5-ASA) and immunosuppressants (e.g. methotrexate or azathioprine) have not shown satisfactory effects or caused excessive side effects.
Infliximab or adalimumab can then be used.
Both active ingredients belong to the group of TNF-α antibodies. So they work against TNF-α, one of the decisive inflammatory substances that are involved in the development of chronic intestinal inflammation in Crohn's disease.
The antibodies are administered as a syringe directly into the blood or under the skin.
Another antibody for the treatment of Crohn's disease, vedolizumab, has existed since 2014.
Its area of application is limited to moderate to severe cases in adults when the standard therapies, including the TNF-α antibody therapy, were not sufficiently effective or had too many side effects.
The antibody prevents inflammatory cells from entering the intestinal tissue. In contrast to the TNF-α antibodies, vedolizumab is administered as an infusion lasting around 30 minutes.
You may also be interested in this topic:
- Therapy of Crohn's disease
- Diet in Crohn's Disease
psoriasis
In recent years, several antibodies have been developed that can be used in psoriasis.
They are mostly used as an alternative if the standard measures such as applying topical therapeutic agents, UV therapy or taking immunosuppressants have not shown sufficient effect or have caused excessive side effects.
The class of TNF-α antibodies is directed against the inflammatory factor TNF-α, which plays an important role in the development of psoriasis.
This group includes infliximab, etanercept, adalimumab, golimumab, and certolizumab. In addition, there are the antibodies ustekinumab, secukinumab, tildrakizumab and ixekizumab, which are directed against certain inflammatory messengers and thus prevent the activation of inflammatory cells in psoriasis.
Talk to your doctor about the possibility of antibody therapy.
Together with him, you can decide whether antibody therapy is an option for you and which antibody is best for you, especially with regard to the side effect profile. Regardless of the antibody selected, antibody therapy is often combined with administration of the immunosuppressant methotrexate.
The administration takes place, depending on the antibody, as an infusion or as a syringe.
Read more on the subject at: Psoriasis therapy
With neurodermatitis
Research into possible uses of antibody therapy for the treatment of neurodermatitis is still more or less in its infancy.
Dupilumab is intended to accelerate the healing of skin damage and has also been approved in Germany for moderate to severe atopic dermatitis since 2017. The antibody is administered regularly every 14 days in the form of an injection (syringe) under the skin. Another antibody, nemolizumab, is designed to specifically combat the itching that is often associated with the disease. The antibody is currently being tested in selected patient groups, but has not yet been approved for general use.
Read more on the subject at: Therapy of neurodermatitis
For rheumatism
Antibody therapy can be considered in rheumatism and rheumatoid arthritis if the basic therapeutic agents (pain relievers, cortisone preparations and DMARDs such as chloroquine, leflunomide, sulfasalazine or methotrexate) are unsatisfactory or have excessive side effects.
For example, TNF-α antibodies can be used, which fight the inflammatory process by intercepting the inflammatory factor TNF-α. The active substances adalimumab, etanercept, infliximab, golimumab and certolizumab belong to this class. In addition, the antibodies abatacept, rituximab and tocilizumab are approved, which also alleviate inflammation in various ways.
What all antibodies have in common is that they are often administered in combination with methotrexate in the treatment of rheumatism.
The onset of action with the antibodies usually takes place within a few days and thus significantly faster than with the above-mentioned basic therapeutic agents. In the first few weeks of administration, however, side effects can occur, which are usually expressed as a flu-like infection
Read more on the subject at: Therapy of rheumatoid arthritis
For osteoporosis
Two antibodies are currently available that can be used in osteoporosis.
Denosumab is approved for two situations: for osteoporosis in women after the menopause and in men after androgen withdrawal therapy as a result of prostate cancer. The antibody inhibits the activity of cells that break down bone substance, called osteoclasts.
Denosumab is given as an injection (syringe) under the skin every six months.
The antibody romosozumab has not yet been approved in Germany, but is currently the subject of intensive research. It is expected that it will have a particularly strong effect on women who have reduced bone density after the menopause as a result of hormonal changes. The antibody promotes the activity of those cells that are responsible for building the bone substance. These cells are known as osteoblasts and, to a certain extent, represent the opponents of the osteoclasts described above.
Read more on the subject at: Active against osteoporosis