Bacteria - structure, way of life and diseases
introduction
Bacteria (singular: bacterium or bacterium) are microorganisms that consist of only one single cell. They belong to the "prokaryotes", which in contrast to the eukaryotes (the cells that occur in human, animal and plant organisms) do not have a real cell nucleus.
The word “prokaryote” means something like nucleus replacement: Instead of the cell nucleus typical of eukaryotes, which is separated from its surroundings by a double membrane, bacteria are referred to as a nucleus equivalent.
The heritage (DNA), which is found in the nucleus of other organisms, lies freely in the cell water of bacteria (cytoplasm) in front. In bacteria, this DNA is a strand-like molecule, the bacterial chromosome.
Often, however, it doesn't just swim around, but is attached to the cell membrane. Cell membrane, cytoplasm, DNA and the ribosomes (the smallest protein structures necessary for protein biosynthesis) can be found in every bacterial cell.
Other organelles, which are only found in some bacteria, are a cell wall, an outer one Cell membrane, Flagella (for locomotion), Pili (for attachment to interfaces), Plasmids (small DNA fragments that can be exchanged among bacteria and thus make an important contribution to the development of resistance and gene transfer), a Mucous covering and Vesicles (Vesicles) that contain gas.
In addition to bacteria, fungi are also important potential pathogens for diseases. Please also read our article on this Mushrooms.

Illustration of bacteria

bacteria (Bacteria)
- DNA
- Pilus
- Nucleoid
- Cell wall
- Cell membrane
- Flagellum
- capsule
- cytoplasm
- Mesosome
- Plasmid
- Ribosome
To shape:
a - spherical
Cocci (Micrococcus)
b - rod-shaped
(Bacillus)
c - thread-like
(Streptomycetes)
You can find an overview of all Dr-Gumpert images at: medical illustrations
construction
Bacteria are small microorganisms with a size of around 0.6 to 1.0 µm.
They can have a wide variety of external shapes such as spherical, cylindrical or helical.
However, in their internal structure they are all similar. Bacteria only consist of a single cell. In this cell is that Bacterial chromosome, which is the genetic make-up of the bacterium that DNA, represents. This DNA is around 1.5 millimeters long and ring-shaped. The DNA swims freely in the cell water, the Cytosol.
Bacteria do not have a real cell nucleus and therefore become the so-called Prokaryotes counted.
There are other structures in the cell water that are known as Cell organelles designated. Cell water and cell organelles are collectively referred to as cytoplasm. Cell organelles are for example Ribosomes and Plasmids.
A ribosome is a protein that the bacterium needs to produce additional proteins. A plasmid is a small DNA fragment that contains additional genetic information, for example resistance genes.
Bacteria can exchange plasmids with one another and thus transfer their DNA to other bacteria.
The cell water is through a Cell wall limited. The outer shape of the bacterium is maintained by the cell wall and protection against external influences (other bacteria, bad environmental conditions) is guaranteed. For further protection, some bacteria are additionally supported by a capsule surround. The bacterial cell wall consists to a large extent Murein, a complex sugar with a network-like structure. The network of several layers of Murein envelops the entire cell. Some bacteria also carry other substances in their cell wall, such as certain proteins and fatty acids. These can have a disease-causing effect on the human body and trigger a fever, for example.
The inside of the cell wall is lined with a cell membrane. Invaginations of this cell membrane are called Mesosome and serve to increase the surface area. Cell appendages, the so called Pili out. Pili are used by the bacterium to attach to other bacteria or cells. Some bacteria carry twisted threads of protein called them to move Flagella. When they consume energy, they move like a propeller. Depending on the type of bacteria, there may be more than 12 flagella.
Read more on the subject at: Cell membrane
Multiplication
Bacteria can (unlike viruses) multiply on their own. This is done by a simple asexual division into two parts, usually through transverse division, budding or sprouting.The two newly created cells then each grow into a full-fledged bacterium.
However, since this reproduction takes place asexually, i.e. two clones identical to the previously existing bacterium always arise, bacteria have to use other mechanisms in order to achieve a gene transfer.
A distinction is made here between three forms.
On the one hand, there is conjugation, which the Gram-negative bacteria (see below) in particular make use of. This type of bacteria use the so-called "Sexpili". These proteins can be used to form a bridge between two bacteria, via which DNA can be transferred directly from one bacterium to the other.
Gram-positive bacteria are more likely to practice transduction, a method in which the bacteria take advantage of certain viruses called bacteriophages. These take up bacterial DNA and then pass it on to another bacterium.
The transformation, which can only be found very rarely, is based on the direct uptake of naked DNA.
classification

Bacteria can be classified according to various criteria.
1: Due to their external shape (morphoplogy).
On the one hand, there are spherical bacteria, the cocci. These can either be present individually or together. Most often one finds cocci in large numbers clustered like a cluster (staphylococci), in a long row (Streptococci) or in pairs (Diplococcie.g. Gonococci) arranged. More rarely, cocci come in four (Tetrads) or groups of eight (Sarcines) in front. In addition to the cocci there are also the rods.
These bacteria are elongated or cylindrical or plump (coconut) and have rounded, pointed or rectangular ends. The helical bacteria or spirils (e.g. the spirochetes) can be identified under the microscope thanks to their many easily recognizable convolutions. Finally, there are thread-like bacteria such as streptomycetes.
If an infection with group A streptococci is suspected, a rapid test can easily be carried out at home. For more information on this topic, we recommend the article: Streptococcus rapid test
2: The bacteria can also be differentiated based on their staining behavior.
The so-called Gram stain is used for this purpose. In this method, the bacteria are first treated with a blue dye, which is then tried to wash out again with the help of an alcohol preparation. Those bacteria that fail to do this have a thick cell wall in which the blue dye has practically settled. These, now blue bacteria, are called Gram-positive. After the decolorization with alcohol, another dye, this time a red, is used. The bacteria without a cell wall, from which the blue dye was therefore previously washed out, now stain red and are called Gram-negative.
3: In addition, the different bacteria show different behavior towards oxygen.
Some bacteria can only exist in the presence of oxygen because they absolutely need it to consume it. These bacteria are called aerobic bacteria or aerobes.
The opposite are the so-called anaerobic bacteria or anaerobes, which can only survive in an oxygen-free environment. In between are the facultative anaerobes. These facultative anaerobic bacteria do not need oxygen, but can tolerate it (there is another subgroup here, namely the microaerophilic bacteria, which prefer a very low concentration of oxygen in their environment).
4: Last but not least, the different types of bacteria can be classified according to their endowment with goats (flagella).
There are bacteria that have no flagella at all, some only have a single flagella (they are monotrich), others have exactly two flagella, which lie on opposite poles (amphitrich), several flagella, which, however, are only located on one pole of the cell (lophotrich) and still others are covered with flagella all around (peritrich)
Some bacteria are able to form spores. These spores are resistant permanent forms of the bacteria, which can be developed under poor living conditions in order to ensure survival. Spores reduce their metabolism to the bare minimum, which means they can withstand extreme conditions such as heat or cold, drought, radiation, chemicals or food shortages.
As soon as the external conditions become more friendly again, the spores can transform themselves back into their normal, "active" bacterial form.
transmission
The transmission of bacteria can take place in three different ways: Either through direct contact (Body contact, food, or infected objects), through the air through a so-called droplet infection (for example through sneezing or coughing) or through body fluids such as blood, sperm or vaginal secretions.
Medical benefit
In medicine, knowledge of bacteria and their properties is extremely important, as they play a major role in both health and disease.
Some bacteria are vital for humans. For example, there are bacteria in the large intestine that make an important contribution to normal digestion and the human immune system.
Almost 99% of the bacteria that can be found in the human body live in the intestine, which makes their importance clear at this point.
It is estimated that there are around 1014 bacteria in the human intestine. There is also a large number of bacteria in the entrance of the female vagina that prevent pathogens from entering through this body opening. Various bacteria also live in the mouth and throat area and on our skin, but they do not harm humans and ensure that no potentially disease-causing bacteria can spread there.
On the other hand, there are also a myriad of bacteria that are responsible for a wide variety of diseases, some of which are life-threatening. Bacteria cause inflammation of practically all organs (bladder infections, pneumonia, inflammation of the periosteum, etc.), can infect wounds or even blood poisoning (sepsis) trigger.
treatment

Once infection with a bacterium has taken place, there are now a large number of means of combating it. These are summarized under the umbrella term antibiotics, of which there are now an apparently infinite number.
The best known and still one of the most effective antibiotics is penicillin, which was developed in 1945. The different antibiotics attack the bacteria in different places, for example on their cell wall or on their protein synthesis.
A problem today is the frequent, sometimes too generous use of antibiotics, which makes bacteria increasingly resistant to these active ingredients, which means that they can no longer be killed by them.
Occurrence
Bacteria in the stomach
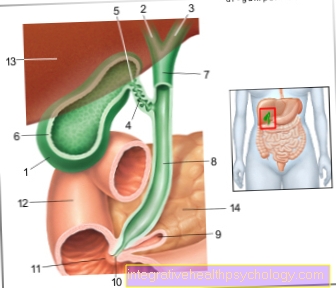
The stomach is a Part of the digestive tract. As Hollow organ can the stomach die temporarily store ingested food and start them with his strong muscle layer too crush. The stomach also produces one acidic gastric juice with which the Food mixed up and further decomposed becomes. This acidic gastric juice prevents bacteria from surviving in the stomach and therefore offers protection against infection. It is therefore In principle, bacteria cannot grow in the stomach.
A exception represents a certain bacterium, the so-called Helicobacter pylori, represents. This is a small rod-shaped bacterium, which due to an endowment with certain substances the neutralize acidic gastric juice and thus the Gastric mucosa colonize and survive in the stomach can. Colonization of the stomach with Helicbacter pylori is not uncommon. In Germany wears every fourth adult the bacterium in itself. Helicobacter pylori infection is thus one of the most common bacterial infections.
Symptoms
A patient with Helicobacter pylori infection is often symptom-free for years. In the long run, however, it can become a severe irritation of the gastric mucosa come, because this is exactly where the bacterium settles and continues to multiply. The persistent irritation can lead to a Inflammation of the lining of the stomach come, a so-called gastritis. Typical complaints with such an inflammation of the gastric mucosa are Pain in the upper abdomen, as well as a Sensation of pressure or fullness in the upper abdomen. Furthermore, it can be too nausea, Vomit and Loss of appetite come. With persistent inflammation of the gastric mucosa, also increases the risk of developing a stomach ulcer. Furthermore, infection with Helicobacter pylori favors the Development of stomach cancer. In order to prevent inflammation of the gastric mucosa, any suspicion of Helicobacter pylori infection should be clarified in detail.
diagnosis
With the help of a Sampling of gastric mucosa of the patient, the bacterium can be detected directly. Furthermore, various tests in the patient's blood, stool and exhaled air can indicate an infection with the bacterium in the stomach.
therapy
The goal of treating Helicobacter pylori infection is that complete elimination of the bacterium in the stomach. This is done with a Combination of two antibiotic preparations and a drug that inhibits the production of acidic gastric juice called a Acid blockers. Treatment of the bacterium in the stomach is therefore also made Triple therapy called. This triple therapy is the most common form of therapy and is successful in around 70 percent of the cases.
Bacteria in the gut

The intestine is an important part of the digestive tract. In addition to digestion, the intestine also plays a role in the water balance. It also produces various cells that are important for the human immune system. In adults, the intestine is around eight meters long and its entire length is more or less colonized by bacteria. The entirety of these bacteria in the intestine is called Intestinal flora designated.
The colonization of the intestine with bacteria begins during birth and increases with age. The intestinal flora of an adult is then characterized by a large number of different types of bacteria. These bacteria in the intestine are of great importance to humans, as they protect the intestines from other, pathogenic bacteria.
In addition, the bacteria in the intestine support the digestion of food components, stimulate intestinal activity, supply the intestine with vitamins and energy and have an influence on the immune system. If the intestinal flora is changed, however, in the sense of over- or under-colonization with intestinal bacteria, complaints can occur.
Symptoms
These complaints are generally expressed as abdominal pain, food intolerance, flatulence and diarrhea.
diagnosis
A stool sample can be used to determine whether there is a change in the intestinal flora. The so-called H2 breath test can also provide indications of incorrect colonization of the intestine.
causes
Damage to the healthy intestinal flora can occur, for example, if a patient has to take antibiotics due to another disease. As an undesirable side effect, the patient's intestinal flora is also damaged, so that the pathogenic bacteria can spread better. This can lead to diarrhea. In the case of chronic intestinal inflammation, such as ulcerative colitis or Crohn's disease, in addition to genetic impairment and environmental influences, bacterial colonization of the intestine is also assumed.
therapy
The treatment depends on the underlying disease or on the cause of the colonization failure of the intestine and includes measures such as simple medication up to operations.
Read more on the topic: Bacteria in the gut
Bacteria in the blood
Spread from a local focus of disease Bacteria in the Bloodstream off, it comes to one sepsis. Colloquially this is referred to as Blood poisoning. In sepsis, bacteria enter the entire body via the bloodstream and can then potentially damage any organ.
causes
Usually that's human immune system able to fight invading bacteria and curb the further growth of the bacteria. In some cases, however, the function of the immune system is limited or the pathogens are simply too aggressive that the Defense mechanisms fail. The body fails to limit the infection to the place of origin and the pathogens can spread through the bloodstream.
diagnosis
Whether pathogens have passed into the blood can be determined with the help of a Blood culture determine. During this examination, blood is drawn from the patient and this is transferred to various nutrient media. The growth of the bacteria is then observed. Depending on the nutrient medium on which the bacteria then grow, it can be assigned which bacterium is in the blood. Thus can treated in a more targeted manner become. Furthermore, the blood can so-called Inflammation parameters to be examined. These include, for example White blood cell count or Sedimentation rate. However, these are unspecific and only give an indication of whether an infection is present or not.
Symptoms
The focus of the disease can be in different parts of the body and thus bring about a wide variety of symptoms. If the infection spreads into the bloodstream, symptoms such as fever, chills, increase the Heart and respiratory rate, a Drop in blood pressure, Lack of oxygen, as well as a Brain damage. Those affected are seriously ill.
therapy
If the bacteria have spread in the blood and there is sepsis, those affected are treated in an intensive care unit, as the function of the organs can deteriorate at any time. It is about a potentially life-threatening situation. Decisive for the course are one early administration of infusions with liquid and a early antibiotic treatment. Depending on the extent of the organ damage, a artificial respiration and artificial nutrition will be required. The prognosis is bad. Despite therapy Today around 30 to 50 percent still die of those affected by organ failure.
Bacteria in the urine

Urine is produced in the kidneys and excreted through the urinary tract. It consists of over 95 percent water. Urine also contains substances such as uric acid, urea, salts and dyes. There are usually no bacteria in the urine. If bacteria are found in the urine, this can indicate infections of the kidneys and the lower urinary tract, especially if the patient reports additional symptoms and the number of bacteria in the urine is high. When urinating, however, the urine comes into contact with the skin, on which bacteria are found in every human being. It is possible that bacteria get into the urine of healthy people. The mere presence of bacteria in the urine therefore does not prove a urinary tract infection.
causes
A urinary tract infection occurs when bacteria (more rarely viruses) enter the urinary bladder via the urethra, causing the surrounding tissue to become inflamed. Cystitis develops. The pathogens can rise up into the kidneys and trigger inflammation of the kidney pelvis. In the worst case, a urinary tract infection spreads into the bloodstream and blood poisoning develops. Women are more often affected by urinary tract infections than men because the urethra is much shorter in women and bacteria therefore have to travel a much shorter distance. Congenital malformations of the urinary tract and changes in the hormonal balance can also promote the development of a urinary tract infection.
diagnosis
To find out if there is an infection of the kidneys or the lower urinary tract, the urine is examined. The urine is examined for the number of bacteria as well as for a substance that bacteria produce, the so-called nitrite. A number of more than 100,000 bacteria per milliliter is a sure sign of an infection. On the other hand, the presence of proteins, red and white blood cells in the urine is determined. If it contains proteins and white blood cells, this indicates kidney involvement.In most cases, the urine is examined with the help of urine test strips and, if necessary, the urine is examined under a microscope. In addition, a thorough questioning of the patient must be carried out.
Symptoms
Typical symptoms of a urinary tract infection are pain and burning sensation when urinating and an increased need to urinate. Fever and flank pain suggest that the kidney is also affected. In some cases, however, patients have no symptoms at all.
therapy
Various measures can be considered to treat a urinary tract infection. Adequate hydration should be ensured and the abdomen should not become cold. In addition, antibiotics such as co-trimoxazole can be used to kill the bacteria.
prophylaxis
Simple hygiene measures can significantly reduce the risk of urinary tract infections.
Read more on the topic: Bacteria in the urine
Teething troubles caused by bacteria
Teething diseases are contagious infectious diseases that most people already experience in childhood. These teething troubles are triggered by bacteria or viruses. Childhood diseases can be severe and even life-threatening. However, these severe courses have become much less common due to vaccinations and the option of treatment with antibiotics.
Transmission path
Many childhood diseases are transmitted by droplet infection. Another possibility of transmission is smear or contact infection. The disease is then transmitted to other children, especially in groups with many children (kindergarten, school). Transmission to adults is also possible in this way. The period in which sick children transmit the disease, i.e. are contagious, depends on the disease and can be very different. Children are often contagious when they do not feel sick themselves and they are still contagious when treatment for the childhood disease has already started.
Examples
Examples of typical childhood illnesses caused by bacteria are scarlet fever, whooping cough, and diphtheria.
Symptoms
Scarlet fever is characterized by a rash all over the body, the typical reddened tongue (Strawberry tongue), as well as fever, headache and sore throat.
Headache and sore throat can also occur with whooping cough. Characteristic of whooping cough, however, are the convulsive, barking coughing attacks mostly at night.
With diphtheria, symptoms such as fever and difficulty swallowing occur. A coating forms on the mucous membrane of the throat, which can lead to shortness of breath and even attacks of suffocation. This course can be fatal, but the vaccination has made it rare.
Therapy and prognosis
With antibiotics such as penicillin or erythromycin, bacterial childhood diseases can usually be treated and cured well.
prophylaxis
In the case of many childhood diseases, the one-time infection with the pathogen creates lifelong protection against this pathogen. Since some childhood diseases, especially in old age, can show severe courses with organ damage, the Standing Vaccination Commission (STIKO) recommends carrying out the usual vaccinations.
Recommendations from the editorial team:
Do you already know where bacteria can be found in the body?
Find out more here!
- Bacteria in the blood
- Bacteria in the urine
- Bacteria in the gut
- Antibiotic resistance
- Helicobacter pylori