Basalioma on the face
introduction
The basalioma will also Basal cell carcinoma called. It is a form of skin cancer that starts in the bottom layer of the skin.
In contrast to the malignant black skin cancer (malignant Melanoma), which affects the pigmented cells of the skin, the basalioma is classified as semi-malignant (semi-malignant) designated. Basalioma is also referred to as light or white skin cancer. Basalioma most commonly affects areas that are exposed to a lot of sun, such as the face.
Like most cancers, basalioma can spread to surrounding tissues. However, metastases are very rarely formed.

Frequency of basal cell carcinoma on the face
The basalioma on the face makes up about 80% of all basaliomas. It mostly affects older people aged 60 and over.
However, younger people are developing skin cancer as the number of people visiting tanning beds and traveling to countries with strong sunlight increases. Every year around 100,000 people in Germany develop basalioma. Overall, men get sick more often than women.
Symptoms of basalioma on the face
First, nodules form in the skin on the affected area. A thickening can then be felt here. At the edge of this thickening, more and more fine red veins can be seen Telangiectasia to be named.
In the course of the disease, a glassy tumor with a bulging skin often develops. This form of skin cancer is called nodular basalioma designated.
There are also some other forms of basalioma. Some types look like a scar; others can look like an encrusted wound. Some grow in depth, others remain rather superficial.
Most of them show the typical red veins in the edge area, but there are also species in which these are missing. A hardening can usually be felt in all forms, only the external appearance is different.
As a rule, a basalioma on the face does not cause any symptoms other than the cosmetic impairment. There is no pain or itching.
Read more on this topic at: Signs of a basalioma
Where does basalioma occur on the face?
Basalioma usually occurs as a result of excessive exposure to sunlight for decades. The risk of occurrence increases with the amount of ultraviolet light absorbed. For this reason, a basalioma on the face occurs most frequently in areas that are particularly exposed to sunlight. These include the forehead, nose, ears and lips. These areas of the face are therefore also referred to as "Sun terraces”.
In people who spend a lot of time in sunlight for professional reasons, such as sailors, fishermen or gardeners, basaliomas most often develop in the aforementioned areas on the face. However, basal cell carcinoma can generally occur anywhere on the face, so a complete examination of the entire skin is necessary to identify or rule out the disease.
You might also be interested in: Basalioma on the ear
Basalioma on the nose
Basalioma is particularly common on the nose. Since this protrudes from the rest of the face, it is exposed to particularly high levels of UV exposure in sunlight. In addition to a basalioma, other consequences of excessive sunlight, such as sunburn, occur particularly frequently or in a pronounced manner on the nose.
In addition, this part of the face is often left out when sunscreen is applied, which in the long term also increases the risk of developing a basalioma on the nose. In general, people with a larger or more protruding nose with the same skin type are more at risk than those with a smaller nose.
Learn more at: Basalioma of the nose
Basalioma of the eye
In general, a basalioma can develop in all areas of the face and thus also in the eye. The area above the eye is more often affected, as this is where the UV light from the sun is more exposed. However, any other area of the skin around the eye can also be affected.
The treatment is a specialty of a basalioma on the face in the area of the eye, because surgical removal is often more complex and it can be difficult to maintain the required safety distance if the basalioma is very close to the eye. With a timely diagnosis, the treatment is nevertheless successful in most cases.
Read on below: Basalioma of the eye
Treatment of a basalioma on the face
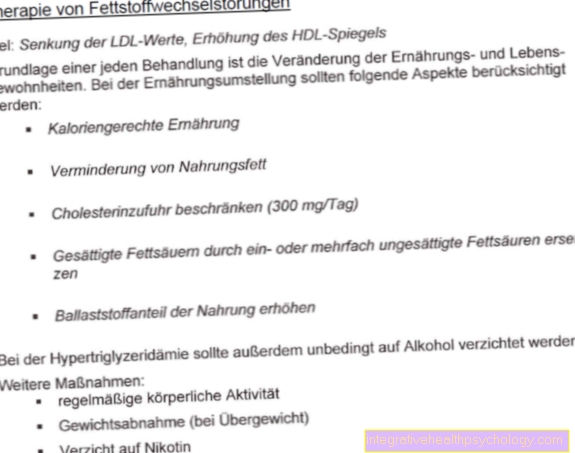
There are several options for treating a basal cell carcinoma. This depends on the size and location of the basalioma and on the patient's condition.
The most frequently used and most successful method is to surgically remove the basalioma under local anesthesia.
This is where the likelihood of the basalioma recurring is lowest. After removing the affected area of the skin, a tissue sample is taken from the edge area and examined microscopically to ensure that there are no tumor cells left there.
If the basal cell carcinoma is too large to be surgically removed, or if an operation is not possible or too risky due to the patient's age or previous illness, patients can be treated with soft X-rays (see also: Radiation therapy) or basalioma can be combated with freezing (cryotherapy).
Even if the location of the basalioma is unfavorable for an operation, for example on the eyelid, other forms of therapy are preferred.
Photodynamic therapy is another treatment option. Here, light-sensitive substances are introduced into the tumor tissue and these cells are then destroyed by light irradiation.
Creams can also lead to healing. There are creams with the active ingredient Imiquimodwhich can be applied regularly for several weeks in the case of superficial basaliomas. Topical chemotherapy using a cream can be used for superficial basal cell carcinomas. That's where the active ingredient is 5-fluorouracil contain. This cream should also be used for several weeks to reduce the basalioma.
Read more on the topic: The best therapy for a basalioma
What scars are there after removal?
The scars that appear on the face after the removal of a basalioma depend on the one hand on the location and on the other hand on the extent of the tumor that is being removed. Often the spread of the basalioma cannot be clearly identified in advance, as the tumor does not always clearly separate itself from the healthy skin.
If a basalioma on the face is still very small and is removed in good time, usually only a very small scar is formed. In the case of larger plants, a larger part of the skin must also be cut out and clearly visible scars may remain.
If a basal cell carcinoma is recognized or treated very late, it may have spread to the face to such an extent that a large defect arises after removal. This must be covered by a procedure to cover defects, for example by transplanting skin from other parts of the body. In the worst case, this leaves a scar after the removal of a basalioma that disfigures the face.
The same applies if the tumor has grown very deep and tissue may have to be removed there as well. Therefore, if you have a basalioma, you shouldn't wait too long to have it removed.
This could also be of interest to you: Scar care
Prognosis for basal cell carcinoma
As a rule, there is a good chance of recovery from a basal cell carcinoma, as in most cases no metastases form. The chances of recovery are given as around 90 to 95%.
In 5 to 10% of cases there is a recurrence of the basalioma, a so-called one develops Relapse.
In these cases it must be removed again. It is very important to have regular check-ups by a dermatologist after treatment for a basal cell carcinoma in order to detect new or recurring basal cell carcinomas in good time.
If organs are already affected in the course of the disease, the prognosis worsens.
Read more on the topic: Prognosis of basalioma
Causes of a basalioma on the face
By far the most common cause of a basalioma is intense sun exposure over a long period of time. For this reason, the face and neck area are most often affected, as there is usually no clothing available to protect them.
Basaliomas can also arise from scars in rare cases. In addition, albinism or the hereditary disease Xeroderma pigmentosum, the so-called moonlight disease, can be causes for the occurrence of a basalioma.
How do you prevent a basalioma on the face?
To protect yourself from basal cell carcinoma, or from skin cancer, it is very important to use sun protection throughout your life. It does not matter whether through clothing or through UV protection from a sunscreen. It is important not to let the harmful UV rays of sunlight on the skin excessively.
Skin cancer screening by a doctor is also useful. While it does not protect against developing skin cancer, it does help to identify it in time and start therapy. Skin cancer screening is covered by health insurers every two years from the age of 35.
You might also be interested in: Initial stage of basalioma
Risk groups for basalioma on the face
The risk group includes people with a light skin type and blue eyes who quickly get sunburned when exposed to the sun. Mostly these are blonde or red-haired people.
But people who are exposed to sunlight for a long time because of their job also have an increased risk of developing basalioma.
This includes, for example, farmers. In addition, the risk is increased if you have already had a basalioma in your life.
Here it is important to have yourself checked regularly.
Diagnosis of basalioma on the face
The diagnosis of a basalioma on the face can usually be made by the dermatologist on the basis of the typical appearance.
Nevertheless, a tissue sample (biopsy) and examined microscopically to confirm the diagnosis.
Read more on the subject at: How do you recognize skin cancer?
Recommendations from the editorial team
- Basalioma
- Skin changes
- Skin cancer screening
- UV radiation
- Melanoma





















.jpg)