Underactive pancreas
definition
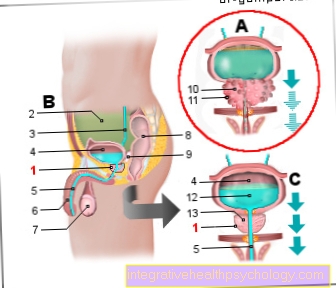
The human pancreas (the pancreas) is made up of two parts known as exocrine and endocrine.
The exocrine part of the pancreas produces digestive enzymes and bicarbonate and releases its secretion into the small intestine through an outlet duct. The enzymes are used to break down the nutrients, while the bicarbonate neutralizes the gastric acid contained in the food pulp.
The endocrine system produces either insulin or its counterpart glucagon, depending on the current blood sugar level. These hormones are not released into the intestines, but into the blood.
If one of the two or both parts of the pancreas is impaired in its function, the expert speaks of a pancreatic hypofunction or a pancreatic insufficiency. Often only one of the two parts shows an impairment, so that one speaks of an exocrine or endocrine hypofunction of the pancreas.
The latter term is rarely used, however, because it is simply a question of diabetes mellitus (limited insulin production).

causes
The causes of an underactive pancreas are extremely diverse. If only the endocrine (insulin-releasing) part is affected, this hypofunction is related to a diabetes mellitus disease.
The insulin-producing pancreas cells are either “worn out” due to age (type 2 diabetes) or are attacked by autoantibodies (type 1 diabetes).
It is different with exocrine pancreatic hypofunction. If it already occurs in childhood, it is usually the result of cystic fibrosis. In adults, the most common cause by far is acute or chronic inflammation of the pancreas (pancreatitis).
Acute inflammation most commonly results from obstruction of the common duct of the gallbladder and pancreas by a gallstone. This causes the secretion to build up and the enzymes it contains attack the pancreas itself.
Chronic inflammation mostly arises from chronic alcohol consumption.
diagnosis
With regard to the diagnosis of an underactive pancreas, a distinction must be made between the exocrine and endocrine parts of the organ. In the case of both diseases, the doctor can use the medical history (patient interview) and physical examination to estimate how likely the presence of an underactive pancreas is.
If endocrine hypofunction, i.e. diabetes mellitus disease, is suspected, various tests are carried out to assess functionality. They are all based on examining the extent to which the pancreas is able to keep the blood sugar level within the normal range.
The measurement of the blood sugar level on an empty stomach in the morning, the determination of the HbA1c value and the implementation of an oGTT test (oral glucose tolerance test) are suitable for this.
With the latter, the test person receives a special sugary drinking solution and one or two hours afterwards his blood sugar is measured.
To diagnose possible exocrine pancreatic insufficiency, the concentration of the digestive enzyme elastase-1 and chymotrypsin in the stool is usually measured. A reduced occurrence of these enzymes in the stool suggests an impaired production in the pancreas.
This examination is associated with relatively little effort and generally delivers satisfactorily reliable results. A secretin-pancreozymin test may be necessary in isolated cases. After the administration of these hormones, the secretion capacity of the pancreas is checked with a probe pushed up to the small intestine.
What is an elastase anyway? To do this, read the article: Elastase
Symptoms of an underactive pancreas
An endocrine pancreatic hypofunction has very variable symptoms depending on the cause.
If the hypofunction is based on the destruction of the endocrine cells by autoantibodies (diabetes mellitus type 1), the symptoms often appear suddenly and sometimes develop into a life-threatening situation within hours.
Those affected usually complain of sweating, a greatly increased urge to urinate and such strong thirst that they sometimes drink more than five liters of fluid a day!
Since acute endocrine pancreatic hypofunction can lead to a diabetic coma and ultimately even death, emergency medical help must be called immediately if symptoms of this kind are present. If, on the other hand, the endocrine hypofunction of the pancreas is the result of an age-related weakening of the organ, it is usually a long-term process that takes months and years.
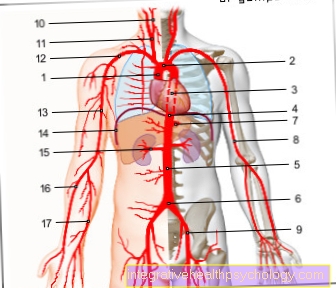
The tricky thing about it is that those affected usually do not feel any symptoms, while the increased blood sugar level due to the hypofunction can cause harm (e.g. damage to blood vessel walls or nerves).
Since digestive enzymes are no longer produced in sufficient numbers in the case of exocrine hypofunction of the pancreas, parts of the nutrients supplied with food are excreted undigested.
The undigested fat, for example, is excreted with the stool, making it unusually light and smelly. This is known as a fatty stool.
Sometimes there is also chronic diarrhea, abdominal pain and flatulence. In addition, fat in food often causes nausea and nausea.
Since not only fat but also the other nutrients cannot be completely digested, there is ultimately weight loss or, in children, insufficient weight gain ("failure to thrive").
Over time, some people have an increased tendency to bleed, such as frequent nosebleeds or a tendency to abnormally large bruises. It is due to the reduced absorption of vitamin K. Since an exocrine hypofunction of the pancreas is often triggered by an inflammation of the pancreas (pancreatitis), some people affected also feel the symptoms of this inflammation first: a belt-shaped upper abdominal pain that can radiate into the back is typical.
More on this: Symptoms of abdominal insufficiency
treatment
The treatment of endocrine pancreas hypofunction (diabetes mellitus) aims to normalize blood sugar levels.
In the case of type 2 diabetes, oral therapy in the form of tablets is often possible; the most commonly used drug is metformin.
In the meantime, however, there is a wide range of orally applicable diabetes drugs, so that an individual decision about the selection of the most suitable active ingredient should be made together with an internist (diabetologist).
In more advanced cases, as well as with type 1 diabetes mellitus, injecting insulin is unavoidable. There are various schemes for this, from which the most suitable one should be selected together with the doctor. Schemes with very clearly defined injection times and quantities do not require the patient to think too much, but they greatly restrict them in terms of nutrition and physical exercise.
Hence, such schemes are often used by the elderly. Younger patients, on the other hand, are often happier with so-called “intensified” schemes, which require more organizational effort, but also offer greater flexibility.
In the case of exocrine pancreatic hypofunction, the removal of the cause is of the greatest importance.
So alcohol consumption should be reduced as much as possible or, best of all, stopped.
If a gallstone is present, it must first be removed with suitable measures. The subsequent treatment is based on the replacement of the insufficiently produced digestive enzymes. For this purpose, a mixture of enzymes called pancreatin is obtained from the pancreas of pigs. Alternatively, there are also herbal preparations.
In addition to the enzymes, fat-soluble vitamins A, D, E and K must also be replaced in more severe cases.
Please also read:
- Therapy of diabetes
- Medicines for diabetes mellitus
Nutrition for an underactive pancreas
If you are affected by an underactive endocrine pancreas (diabetes mellitus), the essential nutritional rules result from the therapy plan, which you should draw up together with your diabetologist.
It goes without saying that the monitoring of carbohydrate intake is particularly important, as this increases the blood sugar level particularly quickly and strongly.
Consequently, the consumption of sugary food should be reduced as much as possible and, ideally, monitored by self-monitoring of blood sugar levels.
Since proteins and fats raise the blood sugar level more slowly and less strongly, their share in the total diet should be increased compared to healthy people. In addition, several smaller meals a day are more advisable than a few large meals.
With exocrine pancreatic hypofunction, many patients experience relief from their symptoms by reducing the amount of fat in their diet. The undigested fat is the main reason for the unpleasant manifestations of illness (foul-smelling diarrhea, stomach pain, flatulence).
However, the consistent supply of substitute enzymes before meals is of decisive importance for the development of the disease in order to prevent malnutrition and vitamin deficiency.
Please also read: Diet in Diabetes
Course of disease
An existing underactive pancreas can no longer be reversed, regardless of whether it is an endocrine or exocrine impairment.
But even if those affected see themselves grappling with the disease for the rest of their lives, most of the course of the disease can be influenced very positively with the means available today.
Especially in the case of endocrine hypofunction (diabetes mellitus), the symptoms can usually be reduced to an absolute minimum and the actual stress on the patient is limited to the immensely important therapeutic discipline.
Nonetheless, over time there is usually a gradual deterioration in the functioning of the organ. In order to be able to monitor these and their possible consequences, consistent compliance with the regular check-ups is strongly recommended.
consequences
The treacherous thing about endocrine pancreatic hypofunction (diabetes mellitus) is the fact that it usually remains without any symptoms for a long time and yet sometimes causes serious consequential damage, which sometimes leads to life-threatening events.
The consequences of endocrine hypofunction include vascular calcification (which can later lead to heart attacks or strokes), kidney damage (diabetic nephropathy), impaired vision (diabetic retinopathy) or damage to nerve tracts (diabetic neuropathy). Another episode of the
Disease is the diabetic foot in which wound healing is impaired due to diabetic vessel and nerve damage.
In severe cases, this secondary disease can even make it necessary to amputate individual toes or even limbs.
Disciplined adherence to the therapy guidelines and regular check-ups by various specialists (especially diabetologists, ophthalmologists, neurologists) can significantly slow down the progression of these sequelae!
An underactive exocrine pancreas often leads to weight loss over time if the therapy guidelines are not followed adequately (e.g. irregular intake of substitute preparations before meals).
While weight loss itself is not that inconvenient for some sufferers, many underestimate the negative effects of long-term malnutrition: Not only is less energy absorbed by the body, but the absorption of the fat-soluble vitamins A, D, E and K is also restricted, weight loss is accompanied by a vitamin deficiency.
Depending on the functions of the individual vitamin classes, this can lead to increased susceptibility to infections and reduced visual acuity (vitamin A), brittle bones (vitamin D) or increased tendency to bleed (vitamin K).
You may also be interested in this topic: Vitamin deficiency