Pancreatitis - How Dangerous Is It?
Synonyms
Medical: Pancreatitis
Inflammation of the pancreas
English: pancreatitis, inflammation of the pancreas
Definition of pancreatitis
(Pancreas = pancreas)
Under one Pancreatitis (Pancreatitis) one understands an inflammation of the pancreas.
Inflammation of the pancreas can have several causes. It can be a one-time event (acute pancreatitis) or occur repeatedly (chronic pancreatitis).
In addition to a disease of the biliary tract, for example, the abuse of alcohol a significant role.

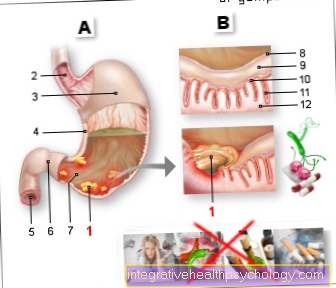
causes
A distinction is made between acute and chronic pancreatitis. The most common causes of the disease are correspondingly different.
Acute pancreatitis, which occurs suddenly and which heals completely with appropriate treatment, is in the majority of cases triggered by diseases of the bile duct system. Particularly noteworthy are stones that get stuck in the duct of the biliary system and, in addition to pain, can also lead to outflow disorders in this system. A corresponding back pressure can lead to an acute pancreatitis.
The second important cause is alcohol abuse, which can lead to acute pancreatitis (see also: Abdominal pain from alcohol). It is a little rarer than the above-mentioned biliary tract diseases but still quite common at around 35%. Even more rarely, an inflammation of the pancreas can be triggered by medication or by an examination method to visualize the bile duct system, which is also known as ERCP (endoscopic retrograde cholangiopancreatography). Since contrast agent is injected into the bile duct, inflammatory changes in the pancreas can occur in some not uncommon cases.
Chronic pancreatitis, which does not heal properly and keeps coming back, is mainly caused by chronic alcohol abuse. This makes up about 80% of the cases. Regular use of medication can also lead to chronic inflammation. The drugs include Beta blockers or ACE inhibitors blood pressure medications, water medications, some antibiotics, some anti-seizure medication, and some chemotherapy drugs.
In addition to the medication, elevated blood lipid levels that are chronically present can also lead to inflammation of the pancreas. The reason is seen in the fact that the pancreas must constantly try to produce fat-splitting enzymes in order to lower the increased blood lipid level and this leads to an overload.
Overactive parathyroid gland can also lead to chronic inflammation of the pancreas. However, the frequency is rather rare compared to the causes mentioned above. Even more rarely, genetic defects lead to congenital and recurring inflammations in the pancreas. In the Asian population in particular, such inflammations can also occur due to autoimmune diseases. The exact reason has not yet been clearly clarified, but other autoimmune diseases are usually present in such cases.
In addition, papillary carcinomas also lead to the development of pancreatitis. Read more about this under: Optic disc carcinoma
Illustration of the pancreas

- Body of
Pancreas -
Corpus pancreatis - Tail of
Pancreas -
Cauda pancreatisauda - Pancreatic duct
(Main execution course) -
Pancreatic duct - Duodenum lower part -
Duodenum, inferior pars - Head of the pancreas -
Caput pancreatis - Additional
Pancreatic duct -
Pancreatic duct
accessorius - Main bile duct -
Common bile duct - Gallbladder - Vesica biliaris
- Right kidney - Ren dexter
- Liver - Hepar
- Stomach - Guest
- Diaphragm - Diaphragm
- Spleen - Sink
- Jejunum - Jejunum
- Small intestine -
Intestine tenue - Colon, ascending part -
Ascending colon - Pericardium - Pericardium
You can find an overview of all Dr-Gumpert images at: medical illustrations
Depiction of the pancreas and gallbladder
- Gall bladder (green)
- Pancreatic cancer (purple)
- Pancreatic duct (yellow)
- Pancreatic head (blue)
- Body of the pancreas (Copus pancreaticus) (blue)
- Pancreatic tail (blue)
- Bile duct (ductus cysticus) (green)
How dangerous is the inflammation for me as a patient?
Inflammation of the pancreas can occur acutely or manifest as a chronic clinical picture. In addition to nausea and vomiting, symptoms include belt-shaped pain around the abdomen. Upper abdominal pain is typical.
The most common cause of acute inflammation is obstruction of the outflow of digestive juices by a gallstone, whereas the chronic form develops mainly in connection with years of alcohol abuse.
The released digestive juices, which are intended, among other things, to break down fats, pose a certain risk potential. On the one hand, these can attack the pancreas itself or, on the other hand, damage surrounding structures. For example, if the duct is obstructed by gallstones, the relatively aggressive secretion backs up into the pancreas and induces inflammation of the organ through digestion.
When the acute inflammation is present, the permeability of the tissue barriers within the pancreas increases significantly, which leads to large amounts of fluid escaping from the vessels into the inflamed pancreatic parenchyma and surrounding tissue. This results in a lack of fluid within the vessels, which causes typical side effects such as low blood pressure, fast heartbeat, fatigue or even headaches.
In addition, calcium is often withdrawn from the blood, which is bound by the released fatty acids and is therefore no longer available to the rest of the body. This can be seen in the regular blood tests to be carried out in terms of calcium deficiency (Hypocalcemia), which is regarded as an indication of a more serious course of the pancreatic inflammation, since only such relevant amounts of fatty acids arise through the destruction of the tissue.
The increasing destruction of the organ releases large amounts of inflammatory substances, which are secondary to systemic inflammation (sepsis) and as a result can cause a life-threatening clinical picture.
If chronic pancreatitis is present, the primary symptoms are often non-specific and only develop over a long period of time. Deficiencies as a result of insufficient fat digestion and absorption as well as secondary vitamin deficiencies occur much more frequently. With increasing loss of tissue, the so-called endogenous pancreatic functions within the framework of the sugar metabolism also fail (occurs with more than 90% tissue loss).
For treatment, the missing enzymes and hormones can easily be replaced with drugs; one speaks here of a substitution.
The chronic inflammation of the pancreas is a relevant risk factor for the development of cancer of the pancreas. In general, it is always associated with a significantly reduced life expectancy, which is usually due to the other diseases of the person concerned.
Course of acute pancreatitis
Of the course Acute pancreatitis (inflammation of the pancreas) has three phases:
- Due to swelling and dying tissue of the pancreas there is an increase in pancreatic enzymes, the parameter of inflammation CRP and the white blood cells in the blood. These changes can be based on the Laboratory values be diagnosed.
- The second phase consists of healing.
- If the pancreas has partially converted into dying (necrotic) tissue, inflammation of these areas is possible.
In serious cases there is even one Blood poisoning (sepsis) possible.
Chronic pancreatitis
This refers to a chronic inflammatory process that affects the area around the pancreas without much relief or healing. In almost all cases, the causes can be seen in chronic alcohol consumption. Alcohol addicts are at greatest risk for this condition, also known as chronic pancreatitis. In addition, some medications (blood pressure medication, antibiotics, anticonvulsants and chemotherapy drugs) can lead to chronic inflammation.
In addition to an increase in the blood lipid level, an overactive parathyroid gland can also be considered a cause. Despite extensive medical research, no exact cause can be found in about 15% of cases.
The diagnosis of chronic pancreatitis is made by means of ultrasound on the one hand, but also through blood tests on the other, in which pancreatic values are examined. If these are greatly increased (lipase), this indicates an inflammatory process. In the ultrasound calcifying structures (whitish visible in the ultrasound) or a cloudy abolition of the normal structure of the pancreas would indicate inflammation. But whether it is an acute process or a chronic one would only be determined by the duration and the relapses that have already occurred. If it is an initial illness, the process would be more likely to be called acute, while a course that is repeated over and over or never completely interrupted would be counted as a chronic pancreatitis.
Read more on the topic: Lipase increased
If the diagnosis of chronic inflammation is made, all alcohol consumption should definitely be stopped and a longer period of food abstinence should be carried out. This is the only way to guarantee that the pancreatic cells will recover. Attempts at conservative treatment, such as rest, painkillers and, if necessary, antibiotics under close supervision of the patient, should definitely be tried first. However, if there is no improvement, a surgical approach should also be considered. The inflamed area is inspected endoscopically and surgically removed. This procedure should be chosen, especially if there are areas of cells that have already died. Extensive inflammation must be treated with sterile irrigation solutions. Chronic or severe pancreatitis can also be fatal in some cases. This mainly affects patients who, despite recurring attacks, do not refrain from consuming alcohol.
Symptoms
In pancreatitis, there are so-called key symptoms:
- Upper abdominal pain and
- an increase in pancreatic enzymes in the blood and urine (e.g. trypsin)
Key symptoms are symptoms and characteristics that are typical and usually always appearing for a certain illness.
The majority of patients (90%) with pancreatitis have an acute onset with severe abdominal pain that can radiate to the side. Often the pain is like a belt around the body.
Other symptoms of pancreatitis are nausea and vomiting, a bloated stomach and paralysis of the intestines (ileus). Fever, low blood pressure and changes in the EKG are also observed.
If the condition is chronic, it often leads to fatty stools - this means excretion of fat that could not be absorbed through the intestines due to insufficient pancreatic secretions, weight loss and diarrhea.
Food intolerance also occurs. So fatty foods are poorly tolerated and lead to nausea, vomiting and pain. The main symptom here is the recurring pain that is not colicky but can last for hours and days.
Signs
Inflammation of the pancreas can be acute or chronic and depending on the form, the signs through which it is noticeable also differ.
An acute inflammation of the pancreas (pancreatitis) is often noticed initially by sudden, severe pain in the upper abdomen, which can also radiate into the back in a belt shape. In addition, there is often nausea and vomiting. In addition, a Intestinal obstruction (Ileus) are present, so that there is stool retention.
The chronic form of pancreatitis usually starts first symptomless. Symptoms such as acute pancreatitis can only appear at a later stage. The pain in the upper abdomen is usually not that intense, but it occurs repeatedly.
As the disease progresses, the pain may increase or persist. If the pancreas is increasingly destroyed by the chronic inflammation, a progressive one occurs Loss of function and the digestive enzymes are produced in insufficient quantities and released into the intestines. This can cause diarrhea and greasy stools (Steatorrhea).
In addition, gas and abdominal cramps can occur. The patient takes more and more weight over time from. Because the pancreas for the Insulin production who is responsible, diabetes mellitus can develop in the case of chronic inflammation. If the inflammation is very advanced, the biliary tract can also be narrowed and one Yellowing of the skin (Jaundice) can occur.
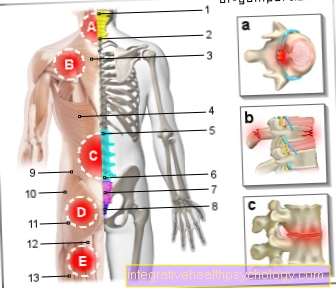
Pain
A so-called Leading symptom the inflammation of the pancreas is the painwhich usually lets the patient go to the doctor sooner or later. In about 90% of the cases pancreatitis patients complain of one moderate but increasing pain in the area of the central upper abdomen. He is called permanent and can thus be clearly distinguished from colic pain in biliary colic. He can Days to weeks can be felt and usually leaves at no time of the day. Rather, a reinforcement is described as a tendency. He is considered by the patient as a Deep pain felt, which has its origin far away from the abdominal surface. For this reason, he is at the medical examination often triggered only after deep palpation (An exception is the very acute inflammation of the pancreas, which may also be associated with peritonitis. In this case, a light touch of the middle upper abdominal area is often sufficient). The indicated pain occurs often intensified after eating on, but different from gallbladder inflammation for a long time after eating. Rather, one can say that the Basic pain if you have inflammation of the pancreas present all day is but impressed by the ingestion of food in the form of a sharp peak of pain.
That becomes characteristic Starting point of pain im middle upper abdomen specified. In many cases it spreads on both sides towards the flank and in some cases it will pulling up to the back specified. Described by the patient Upper abdominal painwho pull in the back, the examiner should always pay attention and carry out further examinations. The term of the belt-like pain used because it begins in the middle upper abdomen and then wraps around the body in a belt-like manner to converge at the back. This description of pain should suggest inflammation of the pancreas, however, the absence in no case means that no pancreatitis is present.
Of the Pain character will be in front abdominal area rather than dull to pulling described to the side and in the back but often as burning or biting. But also numerous mixed forms of pain have been described and rather the indicated localization as the type of pain should lead to suspicion of pancreatitis.
Complications
As with almost all diseases, it can also with the Inflammation of the pancreas complications arise. These include, for example, bacterial infections of the scarred tissue, circulatory shock, as well as encapsulated accumulations of pus in the pancreas (pancreas).
Duration
the treatment
The duration of treatment and the hospital stay for pancreatitis depends on the extent and progression of the disease. While with a mild form of inflammation some days If there is sufficient food abstinence before the diet can be started, it is a question of one more complicated course by a time interval of 2 to 3 weeks without solid food.
of hospitalization
This means that if the course is complicated, the patient will definitely about 3 weeks has to be in the hospital and also at the beginning of the diet he should be there so that he can be well monitored. If complications arise and the person concerned may have to undergo an operation, this time will of course be extended.
If the course is mild, the patient should be discharged from the hospital after about one to two weeks.
the sick leave
The duration of the sick leave depends on the individual course of the disease. With a mild course it is about two to three weeks, but is upwards almost unlimited, depending on the complications.
diagnosis
The diagnosis of pancreatitis is based on symptoms and medical history. The laboratory values and the ultrasound are also important.
Read more on the topic: Ultrasound of the abdomen
In a blood test, an enzyme is specific to the pancreas: lipase. With the help of this enzyme, the fat can be better absorbed by the intestine.
If this enzyme increases in the blood, the diagnosis is likely to be made.
The ultrasound can detect stones that block the ducts (gallstones). The swelling of the pancreas can also be seen on ultrasound.
When a stone actually obstructs the common bile duct (duct for secretions from the liver and pancreas), the transaminases (certain liver enzymes) in the blood rise.
Read more on the subject at: Lipase level
blood values
Since the tissues of the organ perish when the pancreas is inflamed, the enzymes that are produced there will be found in the blood to a greater extent than normal. It is the Lipase and the Amylase, with the lipase being the most telling. In addition, there are general signs of inflammation, especially in the acute form of inflammation, which can be detected in the blood. These include an increased CRP (C-reactive protein) level and an increased number of white blood cells (leukocytes). In very severe cases, the blood sugar level and the hematocrit value are also increased. This is a marker for the cell density in the blood.
The changes in the blood occur both at the acute form of inflammation, as well as a thrust of the chronic pancreatitis on.
Depending on what is causing the pancreatitis, Gallstones For example, the liver enzymes (GOT, Gamma-GT and alkaline phosphatase) and the bile pigment (bilirubin) may also be increased.
prophylaxis
The prophylaxis Pancreatitis consists in eliminating causes such as: E.g .: avoid alcohol and certain medications or remove gallstones from the biliary tract.
With recurring Gallstones Consider removing the gallbladder.
The risk of gallstones forming can be reduced by eating a balanced, low-fat diet.
therapy
If the diagnosis of pancreatitis is made, it should, if possible the triggering cause can be eliminated. In most cases this means that the Alcohol consumption stopped must become. Also appropriate Stonesfound in the bile duct and causing inflammation should be endoscopic or also, if necessary, be surgically removed. After that, the first attempt is usually made To fix inflammation conservatively. This is mainly done through a close control of the patient in the intensive care unit. Get medication Painkiller administered as well as on one balanced fluid balance respected. Also should close-knit laboratory tests carried out to make it clear whether the inflammation is worsening or tending to decrease. If the triggering cause has been eliminated, it is not uncommon for pancreatitis to heal completely with this conservative treatment. Conservative treatment also includes one appropriate nutritional leave as long as the patient still complains of pain. You can then slowly start building up your diet again.
Antibiotics can also be administered (both as a tablet and as an infusion) but should only then used when the pancreatitis is a necrotizing form or when An abscess near the pancreas could be seen. If conservative treatment is unsuccessful and the patient's health deteriorates, it must be considered surgical intervention to undertake. He will usually endoscopic carried out. Three devices are brought close to the inflamed area and severely inflamed tissue or already dead (necrotic) tissue is removed. If the inflammation is very advanced or if the anatomical conditions do not allow an alternative, then it must in exceptional cases the operation can be carried out openly. With very pronounced inflammatory findings, peritonitis (inflammation of the peritoneum) may also have occurred. In this case, a so-called lavage must be carried out in addition to the exposure and removal of the affected area. This procedure is a kind of rinsing of the abdomen with a sterile liquid, which is supposed to ensure that bacterial foci that are not immediately visible are cleared. In the case of very extensive findings, it may be necessary under certain circumstances that this rinsing process has to be repeated several times. Concomitant antibiotic treatment should also be considered in this case.
nutrition
Depending on how far the pancreatitis has progressed and how much tissue in the organ has already been destroyed, patients have to Enzyme lipase take in. This plays an important role in fat digestion. In addition, those affected should seek advice from a nutritionist on how to better deal with the disease by changing their diet.
If the inflammation of the pancreas is diagnosed, the pancreas should be the first relieved and the patient should not eat any food. The nutrients are supplied via the blood (parenterally).
In the case of a mild course of acute pancreatitis, these are usually included 3 to 5 days. After the symptoms have improved, the diet can be started. Initially, the patient should eat easily digestible carbohydrate foods consisting of rusks, white bread with jam, porridge and sweetened tea. If this is well tolerated, protein-rich, low-fat foods, such as low-fat milk and cheese, lean poultry, low-fat fish, vegetables and low-acid fruits, can be added.
The fat content of the food can then be increased slowly, but should be done in very small portions at first. Once all symptoms have subsided, the diet is complete and the patient can eat whatever he can tolerate.
If the inflammation is more severe, the patient may have to be fed artificially. This is done via a Small intestine probe and is usually maintained for about 2 to 3 weeks before slowly starting the diet. This takes place in the same stages as mentioned above.
Important is with any type of pancreatitis permanent to refrain from alcohol and nicotine.
forecast
Of the course one acute Pancreatitis is difficult to predict. For the prognosis it is crucial that the patient is regularly monitored and checked at short intervals.
This is necessary in order to recognize and treat possible complications quickly, or better to avoid them completely.
The mortality inflammation of the pancreas depends on the severity of the disease. If the dying tissue becomes infected, the prognosis is generally worse than with sterile = non-infected tissue.
Other topics that might interest you
- You Are Here: Main Subject: Pancreatitis
- Pancreatitis causes
- Pancreatitis Symptoms
- Pancreatitis therapy
- Pancreatitis duration of therapy
- Pancreatic Weakness - You Should Know That!
- pancreas
- Functions of the pancreas
- Upper abdominal pain
- Alcohol addiction
- Fat stool
- Abdominal pain
- Abdomen