Pelvic vein thrombosis
What is pelvic vein thrombosis?
Pelvic vein thrombosis is the narrowing or closure of one of the pelvic veins by a blood clot. Blood clots are caused by changes in blood composition or flow rate and are typically located in the deep leg and pelvic veins. Pelvic vein thrombosis can cause pain, swelling, and bluish discoloration of the skin on the leg.
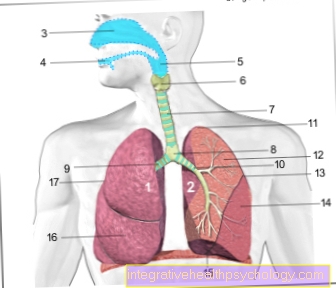
Pulmonary embolism is a dreaded complication of pelvic vein thrombosis. This is where the blood clot detaches from the leg and gets stuck in the pulmonary vessels, causing shortness of breath.
First read the main page on Thrombosis for general information: What is a thrombosis?

I recognize a pelvic vein thrombosis by these symptoms
Pelvic vein thrombosis can have very few symptoms and is often overlooked for a long time. Symptoms that may occur will show up on the leg of the affected pelvic vein.
This can lead to strong feelings of tension and heaviness on the skin. The leg may be swollen and the skin may look shiny. Pain in the leg is particularly typical when exercising, patients often report pain when they put pressure on the calf muscles.
However, a pelvic vein thrombosis can only show up when the dreaded complication of pulmonary embolism has occurred. This is where the clot separates from the pelvic vein and is transported along the bloodstream into the blood vessels of the lungs and gets stuck there. This leads to shortness of breath and chest pain. Without treatment, pulmonary embolism can be fatal. So, if you are after a long flight or a long bed rest, e.g. If you notice changes and pain in your leg after an operation, or if you suddenly find it difficult to breathe, you should urgently seek medical attention.
A thrombosis in the body can lead to pulmonary embolism, a disease that can be quickly fatal. For this reason, it is all the more important to detect a thrombosis quickly enough to initiate the necessary measures. If there is already a suspicion of a thrombosis, you can confirm this using the following article: This is how you can recognize a thrombosis
Pain in the groin with pelvic vein thrombosis
Since the pelvic veins are anatomically located in the groin area, it can initially be assumed that the closure of a pelvic vein leads to groin pain. Although this is entirely possible, it is by no means typical. Pelvic vein thrombosis often has very few symptoms and is more likely to be shown by swelling and feelings of tension in the leg. However, pain can occur anywhere on the leg, from the sole of the foot to the groin, but it is by no means essential.
Typical causes of pain in the groin are, for example, hernias, tendon or muscle injuries or joint diseases (e.g. hip arthrosis).
However, if the groin pain occurs as part of an increased risk of thrombosis (e.g. after operations, long-haul flights or in the context of cancer), this symptom should urgently be clarified by a doctor in good time.
Groin pain is rather untypical for a pelvic vein thrombosis. Find out what could actually be behind the groin pain: Pain in the groin - these are the most common causes
Causes of a pelvic vein thrombosis
Thrombosis, i.e. the closure of a blood vessel by a blood clot, often occurs primarily in the deep leg and pelvic veins. The cause for this is usually either a change in the composition of the blood or the flow rate.
One of the most common causes of a pelvic vein thrombosis is immobilization, i.e. restricted movement and strain on the leg. This often occurs in the context of operations and infections with bedridden but also in the context of long flights or car trips.
Due to the lack of movement of the leg muscles, the blood in the veins is pumped back towards the heart in a reduced amount and collects in the leg veins. This is a risk of developing a clot.
If the blood composition is changed, the blood can clot more easily (so-called hypercoagulability), which consequently leads to an increased risk of thrombosis.
The cause of increased coagulability can usually be found genetically. Here, factors in the blood that are responsible for a balance of blood clotting and anticoagulation are reduced or have no function. A well-known example of the disease is factor V deficiency.
A deficiency in anticoagulant blood components can also develop in the course of life and is particularly typical of liver weakness.
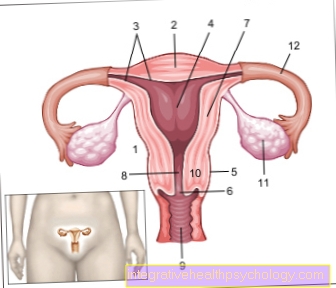
Further risk factors for a blood clot are an increased influence of estrogen (e.g. from taking birth control pills or during pregnancy) and damage to the blood vessel walls (e.g. from smoking for many years and increased blood lipid levels).
You can also find detailed information on the causes under: Causes of Thrombosis
Course of the disease in pelvic vein thrombosis
The course of a pelvic vein thrombosis can be very different. Many pelvic vein thromboses proceed without major physical discomfort and can remain inconspicuous over a long period of time.
Symptomatic symptoms often lead to a feeling of tension in the leg. Pressure-dependent pain can also be added. These symptoms should improve quickly with appropriate therapy. For the coming months, the doctor's instructions should be strictly followed in order to prevent a new thrombosis.
If a so-called post-thrombotic syndrome occurs, the course of the disease can be prolonged and pain, skin changes and swelling can be present over a longer period of time. In some cases these symptoms only recede very slowly and may persist for years.
Duration and prognosis of pelvic vein thrombosis
The duration of a pelvic vein thrombosis is very individual and depends on the selected therapy option.
In most cases, pelvic vein thrombosis is treated with a blood thinner. This must be taken for at least six months. If individual risk factors such as cancer are added, the anticoagulant therapy can be extended. This should be determined in consultation with the attending physician and urgently adhered to in order to prevent a new thrombosis.
The prognosis of a pelvic vein thrombosis is good if it is recognized and treated early.
The most important complication that can significantly worsen the prognosis is pulmonary embolism. This is where the blood clot detaches from the pelvic vein and is washed into the pulmonary blood vessels. If important pulmonary vessels are closed, it can lead to shortness of breath and circulatory failure. This is life threatening! Therefore, in the event of sudden leg pain or shortness of breath, especially after long flights or bed restraint, you should urgently consult a doctor in order to rule out a leg or pelvic vein thrombosis!
Diagnosis of pelvic vein thrombosis
If the typical symptoms of a pelvic vein thrombosis occur, such as a feeling of heaviness and tension, pain, swelling and blue discoloration of the leg, specific thrombosis diagnostics should be carried out.
Here, so-called color duplex compression sonography is the diagnostic standard. This is a special ultrasound scan of the leg veins that can show the blood clot and the decreased flow rate of the blood. This examination is painless and has no radiation exposure.
Furthermore, increased D-dimers can be found in the blood, a laboratory parameter that is typical for blood clots, but can also be increased in other diseases (such as cancer) and is therefore only of limited informative value.
If the blood clot is not clearly detectable in the ultrasound, an imaging examination with a contrast agent can also be used.
Treatment of pelvic vein thrombosis
If a pelvic vein thrombosis has been diagnosed, therapy must be started quickly in order to keep the risk of pulmonary embolism as low as possible.
The current therapy consists of so-called anticoagulation. This refers to the administration of medication that inhibits blood clotting and thus prevents further clots from forming.
Read more on the topic: Xarelto®
You can use several medications, also known as blood thinners in everyday life. Heparin is often used, which, depending on the preparation, can be given once or twice a day with a syringe under the skin (subcutaneously).
Alternatively, so-called direct oral anticoagulants, which are given in tablet form (e.g. Xarelto), can be used.
The duration of the blood thinning depends strongly on the cause of the pelvic vein thrombosis and is carried out for at least six months. This is primarily used as a preventative measure to prevent a new clot from forming. If the risk factors are increased, the duration of the blood thinning can be extended.
If the symptoms are very pronounced and especially in young patients, the blood clot can also be surgically removed. Blood thinning should also be done here to prevent further clots.
In addition, pressure treatment should be carried out using compression stockings for at least three months. It is also important that no bed rest is observed, but rather moderate physical activity is observed.
In addition to the briefly listed therapy options, you can also read the treatments in detail using the following articles:
- Drugs for thrombosis prophylaxis
- Compression stockings
- Measures for thrombosis prophylaxis
When is surgery necessary for pelvic vein thrombosis?
In many cases of pelvic vein thrombosis, surgery is not necessary. It is mainly used with very pronounced symptoms such as severe leg swelling and severe pain recommended. This applies in particular to younger patients, who are also most likely to meet the necessary requirements for an operation (e.g. healthy cardiovascular system).
Another indication for an operation is the highly dramatic form of venous thrombosis, which is known as "Phlegmasia coerulea dolens" designated. Here all venous vessels of a leg are closed and a blood flow can no longer be guaranteed. There is maximum pain and swelling in the affected leg. Only emergency surgery can prevent the leg from amputating. Fortunately, this maximum picture of a pelvic vein thrombosis is very rare.
Recanalization in a pelvic vein thrombosis
Recanalization is a surgical procedure in which the pelvic vein is freed from the thrombus and the venous canal is opened again, so to speak. A catheter (a thin tube) is usually pushed into the affected vein. At the end of the cathether there is a small balloon that can be inflated once it is behind the clot. This will allow the clot to be pulled out of the vein.
Alternatively, a highly concentrated amount of blood thinner can also be given locally on the clot via the catheter and the fragments of the clot that arise collect.
A competent doctor should determine in consultation with the patient whether recanalization is indicated.
Is it allowed to undergo lymphatic drainage with a pelvic vein thrombosis?
Many patients who suffer from water retention in the connective tissue (so-called edema) can benefit from lymphatic drainage.
This is a specific massage of the affected body region by physiotherapists, which causes excessive fluid to be removed again via the venous vascular system.
If you suffer from an acute thrombosis, lymphatic drainage on the legs should be avoided. The irritation from the massage and the supply of fluids to the venous system could loosen the clot and ultimately lead to pulmonary embolism.
Lymph drainage should only be resumed when the thrombus has grown firmly together with the vessel wall. This can take different lengths of time, as a rule 12 weeks should be expected.
In any case, you should get a doctor's approval before you start lymphatic drainage again.
Find out more about the "lymph drainage" therapy form at:
- What is lymphatic drainage?
- When does manual lymph drainage make sense?
What can be the long-term consequences of a pelvic vein thrombosis?
Pelvic vein thrombosis can also lead to long-term effects or complications. A dreaded complication is pulmonary embolism, in which the blood clot is flushed from the leg into the pulmonary vessels. It can lead to shortness of breath and circulatory failure.
The most common late sequela of pelvic vein thrombosis is the so-called post-thrombotic syndrome. This leads to chronic changes in the affected vein, which can lead to various problems such as leg swelling, varicose veins, skin changes and itching.
Another frequent long-term consequence is a renewed pelvic or leg vein thrombosis, especially if a genetic disease is responsible for the increased blood clotting. It is therefore always useful to determine the cause of a pelvic vein thrombosis.
Read more about the disease "Post-Thrombotic Syndrome" at: Post-thrombotic syndrome
Recommendation from the editor
We recommend that you also take a look at the following articles for more information on the subject of "thrombosis":
- Can a pelvic vein thrombosis also lead to a perianal vein thrombosis?
- Pain in the calf - what are some indications that I have a thrombosis?
- Thrombosis in the eye
- What are the dangers of heparin therapy ?: Heparin-induced thrombocytopenia
- Postoperative thrombosis prophylaxis