Treatment of a herniated disc through physiotherapy
Treatment plan for a herniated disc

The treatment plan consists of passive therapeutic techniques and an active exercise program.
From the beginning, the patient should observe certain rules of conduct and perform the exercises they have learned at home several times a day, alternating with phases of relief.
Therapeutic options and self-help for acute herniated discs in the lumbar spine:
The following self-exercises are learned with the help of the therapist and can then be continued at home.
You might also be interested in this topic: Exercise after and after a herniated disc
Perception exercises for the home
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Objective:
- Body awareness training
- Pain relief
- Improving stability as a long-term goal
Since the body perception of the patient is disturbed by the pain, special emphasis should be placed on teaching exercises for perception training at the beginning of the physiotherapeutic treatment. With simple tension exercises for the deep, stabilizing postural muscles in the pain-free area, the patients learn, with the help of the therapist, to feel their muscles and their spine again and to experience muscle tension and spinal column movement as something positive again without fear. The exercises listed in the topic Physiotherapeutic treatment of spinal instability are particularly suitable for this.
Read more on the topic: Physiotherapy for a herniated disc and exercises after a herniated disc of the lumbar spine
Traction (train)

Objective:
- Pain relief
Starting position: The patient is placed in a symmetrical supine position that is as symptom-free as possible, with legs raised.
Therapeutic technique: The physiotherapist uses a certain belt fixation to carefully pull the spine lengthways
Practice at home

Starting position: symmetrical supine position with as few symptoms as possible with legs raised
Execution of the exercise: The patient pulls his lumbar spine slightly apart by pushing his arms against the thighs, which are positioned as close as possible to the groin. During this exercise, you should feel a slight stretch in the lumbar spine.
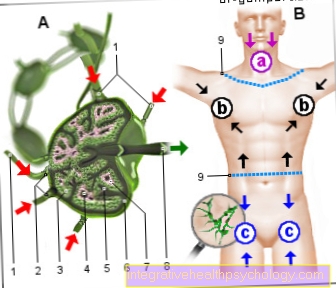
By pulling on the spine, the "creating space" between the vertebral bodies relieves the load on the intervertebral disc and the emerging nerve. The patient's posture is reduced.
The traction option in the sling table should only be carried out after careful trial treatment and in intermittent form. Cave = caution: the pain symptoms known to the patient must not be caused when performing the traction. There should be a feeling of relaxation and pain relief.
Nerve mobilization
Goals and impact:
- Raising the pain threshold
- Reduction of muscle tension and relieving posture
- Improve metabolism
Starting position: the patient lies on his back, as symptom-free as possible, with his legs outstretched, the hip joint turned outwards.
Therapeutic technique: The physiotherapist brings the leg into the internal rotation position of the hip joint approx. 20-30 times and leads it back to the starting position. Patient This technique can only be used if the patient can lie in this position for a while.
Practice at home

Starting position: as with the therapeutic technique
Execution of the exercise: The patient independently rotates the leg inside and returns it to the outside rotation about 20 times every hour.
Cave: the pain symptoms known to the patient must not be caused when the nerve mobilization is carried out. There should be a feeling of relaxation and pain relief.
Passive muscle relaxation techniques
Goals and impact:
- Relaxation of the muscles
- Improve metabolism
- Pain relief
Cave: I consider classic massage therapy to be contraindicated!
The patient's posture resulting from the reflexive tension of certain muscle groups is an important protective function for the affected spinal column segment. A passively induced decrease in tension in the muscles can possibly lead to increased reflex activity and thus possibly increase the pain symptoms, especially if the massage is performed with high intensity.
However, depending on the individual pain findings, myofascials (myo = Muscle tissue, Fascial = Connective tissue) soft tissue techniques, careful targeted trigger point treatment or muscle energy techniques are carried out. Relaxation, especially in the gluteal muscles, usually relieves pressure on the sciatic nerve and thereby reduces pain.
Active muscle relaxation exercises
For the following muscle relaxation exercises, pain-free sitting must be possible. The exercises must not trigger the typical pain. There should be a feeling of relaxation, which, if possible, continues after the exercises are finished.
Practice at home
Starting position: sitting on a chair
Execution of the exercise: In the seat, the upper body is slightly bent forward until shortly before the painful position occurs and turned to the affected side. The hands grip the thighs from the outside.
Tension application: stretching and rotating the upper body to the opposite side, holding tension for approx. 10 seconds. , then place particular emphasis on relaxation.
Self-exercise at home:
Starting position: sitting on a chair, affected side on the left
Execution of the exercise: In the seat, the upper body is slightly bent forward until shortly before the painful position occurs and turned to the affected side. The hands press against the thigh from the inside.
Tension application: stretching and rotating the upper body in the twisted direction, maintaining tension for approx. 10 seconds, then placing particular emphasis on relaxation.
Combination of active and passive relaxation technique

Therapeutic technique:
Goals and Effect
- Heat development, improved blood circulation
- Relaxation of the lumbar muscles
- Slight traction of the lumbar spine
- Rapid improvement in flexion movement
Starting position: the patient is in the four-legged position = bench position on a treatment bench with overhanging feet - this makes it easier for the therapist - or at home on the floor with a towel under the back of the foot - this unfortunately makes it a bit more strenuous for the assistant.
Execution of the exercise: the therapist or the assistant at home stand behind the patient and place both hands above the sacrum near the back muscles located near the lumbar spine. Pressure is built down towards the abdomen and at the same time up towards the head. Against this pressure of the hands, the patient moves the spine into a "cat hump position" and then the buttocks towards the heels. As a result, the assistant's hands slide towards the head without reducing the pressure. Then the pressure is released and the patient returns to the starting position.
Alternative self-exercise at home if no helper is available:
Starting position: upright sitting on a chair with a backrest, 2 tennis balls in a knotted sock are on the right / left of the lumbar spine between the lumbar spine and the back of the chair. The arms are crossed in front of the chest.
Execution of the exercise: By pushing the feet against the floor and pushing the chest back, the pressure against the balls is increased. While maintaining the pressure, the spine is moved in flexion. This is followed by releasing the pressure and returning to the starting position.
Hands off therapy according to Mc. Kenzie
Goals and impact:
- Pain reduction
- Centralization i.e. Shifting the pain from the leg towards the spine
- Improvement of the mobility of the spine
Test movements: The therapist teaches the patient certain test movements that the patient performs several times in a row. It usually begins with movements in the direction of spinal extension, as these often lead to pain relief, while bending and turning movements are usually a pain intensifier. When performing the movements, changes in pain perception and sensitivity occur very quickly, which also persist after the test movement. Pain reduction and centralization, which means moving the pain out of the leg towards the spine, are the decisive criteria for continuing the test movement in a daily exercise program.
Test movement 1
in the prone position, the forearms are propped up and the spine is straightened up to the pain threshold.
Test movement 2

in the prone position, the hands are propped up and the spine is straightened up to the pain threshold
Test movement 3

in the supine position, the arms are crossed in the neck and the closed legs are moved from right to left up to the pain threshold
Test movement 4

In the supine position, the legs are pulled towards the body and the lumbar spine is brought into flexion in this way to the point of pain
Test movement 5

while standing, the spine is carefully straightened.
Test movement 6

When standing, the spine is carefully rolled, vertebra by vertebra, and slowly flexed until it is at the pain limit; when straightening up, bend the knee slightly
Home exercises for yourself
Depending on the patient's reaction, the test movements result in the selection of self-exercises (see photos / description under test movements) for at home. A maximum of one new movement per day is recommended as an extension of the home exercise program in order to maintain control over the eventual trigger if the symptoms worsen. Patients are instructed to monitor their symptoms and assess changes in symptoms.
Starting positions: see test movements
Exercise execution: see test movements
Dosage: the recommended exercises should be performed every hour with 10 repetitions, if the patient's situation allows.
Motivation: Since the reduction in symptoms is visible during and after the exercise with successful therapy, it is easy to motivate the patient to continue practicing.
Note: The continuation of the techniques and exercises only makes sense if the treatment is successful. After the first 5 therapy units and during this time continuous practice at home, it should be assessed whether the success of the treatment is satisfactory and whether the Mc.Kenzie therapy should be continued.