Biologics
introduction
The immune system is essential for the survival of every human being. In the course of evolution, this has developed into the so-called adaptive immune system in humans. This gives us the opportunity to react more differently and more effectively to bacteria and viruses. The immune system protects us. It helps us survive the battle with inflammation better. There are many different types of inflammation modulators. For example the so-called tumor necrosis factor-alpha, which is abbreviated as TNF-α. Together with other factors, this ensures that inflammatory and tumor cells are eliminated before they can trigger diseases.

But these “bodyguards” of our body can also become “criminals”. Because sometimes our immune system turns against us. In these cases autoimmune diseases develop that are difficult to treat with medication. This is where biologics come in. Biologics are also called biopharmaceuticals or biopharmaceuticals. These are drugs that are produced in genetically modified organisms using various means of biotechnology. Examples of these drugs are so-called "monoclonal antibodies" or so-called "fusion proteins". The TNF-α inhibitors, among them the TNF-alpha receptor antagonists, belong to this group of drugs.
A well-known biological is adalimumab, also known under the trade name Humira.
Indications
TNF-α receptor antagonists are used in inflammatory, chronic autoimmune diseases. This means that they are indicated for all diseases where the body's own immune system fights against the body instead of fighting for it. In this process, TNF-α often plays a major role. It ensures that certain cells begin to behave like so-called scavenger cells (macrophages) and thus destroy tissue, bones, cartilage and, depending on the disease, other body cells.
Specific indications are, for example, rheumatoid arthritis, so-called juvenile idiopathic arthritis, psoriatic arthritis, plaque psoriasis, ankylosing spondylitis, Crohn's disease or ulcerative colitis. Biological drugs, such as the TNF-α receptor antagonists, are used when no other drugs help with the diseases mentioned or cause too many side effects.
Biologics for ankylosing spondylitis
Bechterew's disease is an inflammatory, chronic autoimmune disease. It belongs to the rheumatic group of forms. It is one of the so-called spondylarthritis. In Bechterew's disease, the body's own immune system is directed against bone and cartilage cells in the pelvic and back area and destroys them. This can lead to joint pain and deformities in the corresponding areas of the body. Under certain circumstances, TNF-α receptor antagonists can also be used. They inhibit the messenger substance TNF-α. Since this messenger substance plays a major role in the inflammatory process, the disease process is blocked by the TNF-α inhibition. This can alleviate the symptoms and delay the progression of the disease.
Read more on the subject at: Therapy of ankylosing spondylitis
Biologics for psoriasis
The colloquial psoriasis is known in technical jargon as plaque psoriasis. It manifests itself as severe flaking of the skin with itching and burning pain. It can occur in various degrees of severity. In the case of moderate to severe severity, TNF-α receptor antagonists are sometimes used.
One speaks of this severity of the disease when more than 10% of the skin surface is affected or the skin changes show up in particularly visible parts of the body, such as hands or face. A very high level of suffering on the part of the patient is also a criterion for the classification of moderate to severe psoriasis. In some cases the biologics can already be used without all other active ingredients having failed or the presence of side effects having to be proven. The TNF-α receptor antagonists can curb the inflammatory reactions at the point where they arise and thus improve the quality of life for the affected patient.
In addition, secondary diseases that can result from psoriasis, such as depression, can be prevented to a certain extent.
Read more on the subject at: Psoriasis or psoriasis treatment
Biologics for ulcerative colitis
Ulcerative colitis is characterized by strong inflammatory, chronic, intermittent processes of the intestinal mucosa and the underlying connective tissue layer. In severe cases, ulcers form. In contrast to Crohn's disease, the colon is almost exclusively affected. In this type of autoimmune disease, too, TNF-α receptor antagonists can positively influence the course of the disease. A number of different biologics have now been approved for the treatment of ulcerative colitis.
Read more on the subject at: Therapy of ulcerative colitis
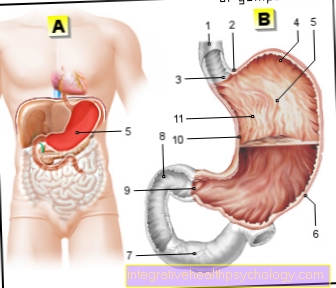
Biologics for Crohn's disease
Crohn's disease is a chronic inflammatory autoimmune disease. The body's own defense system is directed against cells of the digestive tract. This can affect the entire digestive system from the oral cavity to the anus. Here TNF-α plays a role in that it ensures that inflammatory processes and cell destruction occur. Therefore, TNF-α inhibitors can also curb the disease processes in the context of Crohn's disease and partially prevent consequential damage.
Read more on the subject at: Therapy for Crohn's disease
Biologics for rheumatism
Many diseases are rheumatic. When rheumatism is used colloquially, it is usually rheumatoid arthritis. This is a chronic inflammatory autoimmune disease in which immune cells destroy cartilage and bone cells. There is joint pain and swelling. This often happens in the area of the metatarsophalangeal joints of the fingers and toes. Typical morning stiffness often occurs. Here too, the inflammation modulator TNF-α plays a major role. TNF-α receptor antagonists may be used in rheumatoid therapy if other measures fail.
Read more on the subject at: Therapy of rheumatoid arthritis
Active ingredient / effect
Most biologikas are proteins. There are different generations of biologics and therefore also of TNF-α inhibitors. The generations differ from the manufacture.
The ending of the name reveals how much mouse protein is still present in the active ingredients. With the ending –omab it is 100%, with the ending –ximab there is 25% mouse protein, with the ending - 5-10% is still available and with the ending –umab none at all. This plays a role in the tolerability of the drugs.
In addition, the TNF-α inhibitors can work in different ways. They can intercept TNF-α and thus prevent it from binding to its receptor. As a result, certain processes in the cell that would lead to the destructive immune reaction do not take place.Another possibility is that the TNF-α inhibitor blocks the binding site of the TNF-α to the receptor. The drug then acts as a so-called antagonist. It is also possible that TNF-α inhibitors act as so-called fusion proteins. These are also called decoy receptors. Decoy receptors are receptors that bind ligands but do not transmit signals. The TNF-α decoy receptors are soluble receptors that intercept TNF-α before it has reached its original destination. As a result, there is no longer any signal and the growth of the destructive immune cells is slowed down.
Enbrel®
The active ingredient Etanercept is present in the commercial preparation Enbrel®. It is a so-called decoy receptor or fusion protein. Enbrel® is used in particular for rheumatic arthritis, juvenile chronic arthritis, psoriatic arthritis and so-called spondylarthritis. Psoriatic arthritis is a special form of psoriasis that is associated with joint pain. Enbrel® acts as a TNF-α inhibitor in these diseases, as well as in some other autoimmune diseases. However, Enbrel® is not effective in Crohn's disease. As a rule, it is administered subcutaneously once a week with 50 mg or twice a week with 25 mg.
Read more on the subject at: Enbrel®
Remicade®
The active ingredient infliximab can be found, for example, in the commercial preparation Remicade®. Infliximab is a chimeric monoclonal antibody that blocks the activity of TNF-α. Since it is a chimeric monoclonal antibody, the main backbone is human and the antigen binding sites (25%) are mouse protein. This means that the effectiveness is higher than with so-called murine monoclonal antibodies, which consist of 100% mouse protein, and lower compared to humanized (5-10% mouse protein) or human monoclonal antibodies (0% mouse protein). Accordingly, the risk of allergies and intolerance is lower than with murine monoclonal antibodies and higher than with humanized or human antibodies. Remicade® is used for rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and other autoimmune diseases. In contrast to etanercept, the active ingredient infliximab is also effective in Crohn's disease. The dosage is 3-5 mg per kg of body weight, depending on the disease.
dosage
Since the bilogikas are usually proteins, they must be given parenterally (via an infusion). Oral ingestion is not possible because the body would then digest it and the active ingredients could not develop their effect. The dosage depends on the active ingredient and the disease present. The dose is usually in the one to two-digit milligram range and is administered 1-2 times a week.
price
The cost of the biologika is very high. Therefore, they are mostly only used as a last resort. That is, if all other active ingredients that are indicated for the respective diseases are unsuccessful. As a rule, two syringes cost around 1,600 euros a month.
Side effects
Under specialist treatment and observation, TNF-α blockers are relatively well-tolerated and safe drugs. However, as with any drug, side effects can occur. The side effects can be divided into those related to the application and those related to the interference with the immune system. Since the biologics have to be given parenterally (as an infusion), infusion reactions can theoretically occur. Compared to other biologics, this happens more often with the active ingredient infliximab. But with specialist treatment, these types of side effects can usually be well controlled. If Biologikas are given subcutaneously (under the skin), local skin reactions can be triggered. However, discontinuation of therapy has so far been very rarely necessary.
Side effects that occur as a result of the interference with the immune system are based on the additional suppression of physiological processes in our body. The messenger substance TNF-α is actually an important inflammation modulator. Even if it is partially directed against the immune system, it has important tasks relating to the immune system. If these important functions of TNF-α are permanently blocked by drugs, this can lead to corresponding side effects. The susceptibility to infections can increase and the risk of cancer can possibly also increase with long-term use. Damage to the liver, kidneys and heart can occur. In addition, the TNF-α inhibitors can reactivate inactive tuberculosis and herpes zoster.
Depending on which generation of monoclonal antibodies it is, the risk of intolerance and allergies is higher or lower. This means that the more mouse protein is still present in the active ingredient, the greater the risk of allergies and intolerance. In addition, certain autoantibodies can occur. Treatment with a TNF-α inhibitor rarely resulted in what is known as lupus erythematosus. This also decreased again when the biologic was discontinued. In addition, various diseases and relapses in the context of multiple sclerosis, as well as worsening in the case of pronounced cardiac insufficiency, have been described.
interaction
If vaccinations with live vaccines are given and at the same time TNF-α inhibitors, this can trigger disease with the vaccine pathogen instead of a vaccination effect. Furthermore, an interaction could be observed when combining two biological drugs. For example, this has been observed with simultaneous administration of etanercept and anakinra in the course of treatment for rheumatoid arthritis. The effect was not improved, but the side effects were potentiated. Serious infections and a shortage of certain blood cells developed, so what is known as neutropenia developed.
When should biologics not be taken?
If there is a previous tuberculosis disease, no TNF-α inhibitors should be used. This is irrespective of how long ago you had tuberculosis. This is due to the fact that inactivated tuberculosis bacteria are still present in the body after someone has suffered from tuberculosis. These tuberculosis bacteria are inactive because so-called macrophages watch over them. They take care that the bacteria do not become active again. In order for the macrophages to be able to perform this task, they need TNF-α. If this is no longer sufficiently available to the macrophages due to the effect of the drug, they can no longer carry out their task. As a result, the tuberculosis bacteria can become active again and reactivate tuberculosis.
In addition, the presence of hepatitis B is a contraindication for treatment with a biological agent. It has been found that in this case treatment with a TNF-α inhibitor can reactivate herpes zoster. This manifested itself in an increased incidence of shingles and chickenpox in adults.
However, differences were found in the various active ingredients of the TNF-α inhibitors. The diseases occurred more frequently in patients treated with infliximab, while these side effects could hardly be observed in therapy with etanercept. The level of risk of reactivation correlated with age in both diseases, with so-called comorbidity (additional diseases) and with additional treatment with glucocorticoids, such as cortisone.
In order to protect the patient, however, it is currently the case that treatment with a TNF-α inhibitor is generally not permitted in the case of previous tuberculosis or hepatitis B.
Biologics and alcohol - are they compatible?
When treating with biologicals, you do not have to do without alcohol completely. However, there are experience reports in which intolerances have been described. Since biologics influence the functions of the kidneys and liver, it is quite possible that alcohol consumption can lead to acute intolerance. In addition, long-term alcohol consumption in combination with biological drugs can increase the risk of liver and kidney disease.
Treatment cost
The costs are very high due to the manufacturing process and the parenteral administration. TNF-α inhibitors cost around 40,000 to 50,000 euros per year. A single application is at least in the upper two-digit range. In addition there are personnel costs, costs for preliminary examinations, etc. If a specialist in a practice or in a clinic should decide that treatment with a biologic is the best form of therapy, he must give a good reason for this. He can submit an application to the health insurance company to cover the costs. The processing of the application usually takes a few weeks. Once the application has been checked, processed and approved, the health insurance company pays the costs. However, it can limit the duration of the takeover. A cost commitment is often made initially for 3 months. Then a new application must be made.
In 2016 the first so-called biosimilars for the treatment of rheumatic diseases were officially approved. As the name suggests, they are similar to the Biologikas, but not the same as the original. Some authors suggest that they are a cheaper alternative to the biologics. It is controversial whether their effect actually corresponds to that of the original. The health insurances hope to save billions in costs. Other experts are skeptical of the estimates. So far, the biosimilars have only been used in around 1-2% of rheumatism patients. The biosimilars are recommended by the German Society for Rheumatology. However, she advises against switching from the original to the replacement product. Since there are no long-term studies on this yet, the specialist society cannot yet welcome a change in active ingredients in this way. She also advises against making such decisions only for reasons of cost. In addition, she is too optimistic about the assessment of the cost savings. In summary, it can be said that it is not yet possible to estimate how the use of biologics will look in the future, despite the costs.





.jpg)

















.jpg)
.jpg)