Platelets

introduction
Platelets, or also Platelets, are cells in bloodthat are involved in blood clotting, i.e. the Hemostasis play an important role. You are next to that red blood cells and the immune cells (Leukocytes) one of the main components of blood. The technical term thrombocyte for blood platelets is derived from the Greek word thrombos for "Lump"which also aptly describes their function - they form lumps.
Place of formation of the platelets
The platelets are produced in the bone marrow. Here are so-called megakaryocytes (giant cells that form platelets) from which the platelets are pinched off. Up to 8000 platelets can be cut off from one megakaryocyte. This process is called thrombopoiesis. The formation of platelets from megakaryocytes is caused by the hormone Thrombopoietin promoted.
Lifespan and number of platelets
There are usually between 150,000 and 380,000 platelets per µl of blood in the blood. This makes them the second most common cells in the blood. The lifespan of the platelets is around eight to twelve days.
Platelet size
Platelets are small, disc-like platelets with a diameter between 1.5 and 3 µm and are therefore the smallest cells in the blood. Due to their small size, they also have no nucleus. During hemostasis, the platelets change their shape and develop small extensions in all directions (pseudopodia). In this way they can increase their surface area.
Platelet normal values
The normal platelet values vary depending on the age group. Adults should have between 150,000 and 350,000 platelets per µl of blood. In newborns, there are only 100,000 to 250,000 platelets normal per µl blood and in adolescents (up to 17 years of age) it is 200,000 to 400,000 platelets per µl blood. From one Thrombocytopenia (Lack of blood platelets) one speaks when the value is lower 150.000 Platelets per µl of blood. One speaks of thrombocytosis from a value of 500.000 Platelets per µl of blood.
Read more about the topic here: Thrombocytopenia
Functions of the platelets

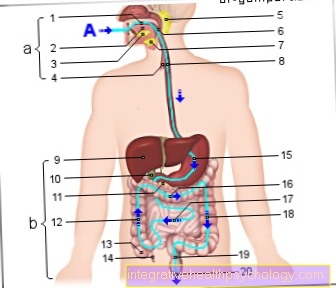
The blood platelets (thrombocytes) have the task of blood clotting. When an injury occurs in a vessel, the platelets are said to have one prevent major bleedingby closing the jar again as quickly as possible. This works by treating a vascular injury Messenger substances be released. The platelets are transported to the injured area in the bloodstream and are activated by the messenger substances. They can now bind to specific receptors (docking sites) on the tissue under the injured vessel. After binding, various mechanisms are activated. On the one hand, the platelets release substances that cause even more platelets to reach the injured area and bind to the platelets that are already present. This activates the platelets and changes their shape. They form small processes in different directions and can do so clump together. There are also various modulators that Clotting factors, e.g. the von Willebrand factorwho support this response. The reaction is also called platelet aggregation. This is also where some medications (called thrombus aggregation inhibitors) come into play, for example aspirin (ASA).
Read more about the topic here: aspirin
The connected platelets form a plug called one red thrombus is called. This temporarily closes the injury. At the same time, the platelets release other substances that activate the coagulation cascade. This leads to the activation of a number of substances first Thrombin and finally fibrin is activated. After being activated by thrombin, the fibrin forms threads and thus forms a plug. This is called white thrombus. He finally closes the vascular injury. This part of the hemostasis reaction is called blood clotting. Various medications can also be used to intervene in blood clotting (anticoagulants). These are, for example, heparins (Clexane Syringe e.g. after operations).
You can read more about the topic here Heparin read
Usually there are always 150,000 - 380,000 platelets in one microliter of blood, which is several trillion cells in a 50 pound man. Nevertheless, their number seems negligible if you look at the 4-5 million red blood cells (or Erythrocytes) per microliter Blood thinks that are in the average person.
Read more about the topic here Tasks from the blood
Platelet disorders

Blood platelets are indispensable for the body due to their function - the closure of injured vessels. A Lack of platelets leads to a shortened hemostasis. The medic speaks of one here Thrombocytopenia. By definition, this occurs from one Platelets- or platelet count of less than 150,000 pieces per microliter of blood on.
There is a very wide range of causes for a lack of blood platelets, which is why only the most common diseases are discussed below.
In principle, a distinction is made between three starting points:
- 1: one lack of production of platelets
- 2: one shortened service life / increased degradation
- 3: Distribution disorders in the blood
1) A lack of production can result from a congenital or acquired educational disorder: An example of a congenital educational disorder is the heritable Wiskott-Aldrich syndrome, with a frequency of 1 in 250,000.
Acquired educational disorders such as a Bone marrow damage on that by a drug, Irradiation, or one poisonous substance can be caused. Also leukemia belongs here and can lead to a blood platelet deficiency as it increases the production in the Bone marrow impaired.
2) A shortened lifespan can easily be due to Bleeding caused: In the case of severe blood loss, every single platelet is urgently needed, which logically means that fewer are available. Also a longer therapy with the thrombosis inhibitor Heparinwhich may be necessary in bedridden patients, can trigger a platelet deficiency: the body forms antibodies against the platelets due to the administration of heparin, whereupon they agglutinate, i.e. aggregate.
Now the platelet level in the blood drops to below 50% of the normal amount - an acute shortage of blood platelets is the result. One speaks here of a so-called Heparin-induced thrombocytopenia of the second type, HIT2 for short. A Immediate change of anti-thrombosis therapy is indexed!
Another conceivable cause of a severe drop in blood platelets is a so-called transfusion incident, in which, for example, a patient blood type A with a blood bag from a donor blood type B receives. The recipient's body reacts to what is strange to him bloodby sending out all of his platelets to bind it. Immediate clumping of the transfused blood occurs and life-threatening shock occurs. In order to avoid such accidents, every doctor is instructed to do what is known as a blood donation before administering blood Bedside test (German: test directly at the patient's bed), in which Patient blood and donor blood mixed on a small card to avoid clumping. Of course, this test is only the last link in a series of strict test mechanisms!
Also a lack of Vitamin B12 or Autoimmune diseases such as Werlhof's disease (antibody formation against blood platelets) can cause platelet deficiency.
3) One Distribution disorder occurs at a Enlargement of the spleen on. The spleen sorts out damaged platelets and destroys them. If the spleen is impaired in its function, the platelets do not distribute evenly in the body.
The causes mentioned are only a brief outline of the wide range of diseases that can lead to a platelet deficiency. However, some diseases with fewer than 100 documented cases worldwide are so insignificant in their relevance that it would go beyond the scope to mention them all here.
In addition to the already mentioned lack of blood platelets, there is, as one can imagine, that too Excess platelets. This is also dangerous for the body and, by definition, occurs from one Platelet count of over 500,000 pieces per microliter of blood on. The technical term for this is Thrombocytosis.
The danger with one Thrombocytosis is the decreased fluidity of the blood, and the associated decreased blood flow. Also form more Thrombi, so Blood clotthat in an emergency in heart, lung or brain can flow, and there the Vessels To block. The result is reduced blood flow to the underlying tissue, which leads to a loss of function and deterioration of the affected organ. Well-known clinical pictures are stroke, also stroke called that Heart attack, and the Pulmonary infarction. In principle, however, any organ can be affected.
Conversely, however, the symptoms mentioned above are not exclusively due to a pathological increase in the number of blood platelets. Other factors like stress, alcohol, Nicotine and Sedentary lifestyle are much more common!
Cause of thrombocytosis is mostly one compensatory overproduction of platelets after major surgery with blood loss, malignant Tumors, chemotherapy, but also chronic inflammatory diseases such as gastrointestinal disease Crohn's disease.
Platelet count too high
If the platelets in the blood are increased (> 500,000 / µl), one speaks of thrombocytosis. These can either be primary (congenital, genetic) or secondary (acquired, due to another disease). Secondary thrombocytosis usually results from infections, chronic inflammatory diseases, tissue injuries or certain forms of anemia. Infections with increased platelet counts: pneumonia, meningitis, kidney inflammation, joint inflammation and bone inflammation, but also gastrointestinal infections or blood poisoning are possible causes. During the infection there is usually an increased consumption of thrombocytes, so the number of blood platelets first drops.
The release of messenger substances (cytokines) then leads to an increased expression of thrombopoietin (stimulates platelet formation) and thus to an excessive production of blood platelets (rebound effect). This effect can also occur after chemotherapy or an autoimmune disease, for example. Not only acute but also chronic inflammation can lead to this increase in cytokines. These include, for example, rheumatism, intestinal inflammation (Crohn's disease, ulcerative colitis) or tissue injuries after accidents or burns. Another cause of thrombocytosis is certain types of anemia. These include hemolytic anemia (anemia caused by bleeding), sickle cell disease, and thalassemia (changes in red blood cells).
These diseases lead to fewer functioning erythrocytes, which in turn leads to a lack of oxygen in the tissues. This ultimately leads to the release of cytokines. The cytokines then increase the production of platelets again. Primary thrombocytosis can also result from various causes. These are inherited diseases (familial primary thrombocytosis) or malignant diseases of the bone marrow (e.g. chronic myeloid leukemia). Even after the spleen has been removed, the values can rise because the storage organ disappears. But even healthy people can temporarily experience elevated platelet counts. For example, this can have emotional causes, such as stress or fear. But physical exertion can also lead to a temporary increase, which is particularly common during pregnancy. This temporary increase is mostly due to the fact that the spleen, which stores up to 30% of the platelets, releases them more. The effect of an increased platelet count is increased blood clotting. Patients have an increased risk of developing thrombi. This can lead to secondary diseases such as leg vein thrombosis, stroke, splenic infarction, pulmonary embolism or the development of acute myeloid leukemia.
Read more about pulmonary embolism here
Diagnosis of platelet disorders

A Lack or excess of platelets can be done very easily with a Blood collection and subsequent Examination in a laboratory be asked. This can be done in hospital or at Family doctor as a routine check and usually only takes a few minutes. The blood is then automated in the laboratory examined, and a so-called "blood count" created. In addition to the number of blood platelets, this also contains the Erythrocytes and White blood cell count, as well as a lot of other parameters (Inflammation values, Thyroid levels, etc.) A total of over 500 different parameters can be determined, but this is omitted for reasons of cost and sensibility. Usually one simply distinguishes between a "small blood count"And a"large blood count". The tested values are usually the same everywhere, with mostly small differences between the clinics.
Therapy of e-diseases of the platelets
A platelet deficiency of less than 50,000 platelets per microliter of blood is dangerous in most cases and should be treated. A number of treatment methods are available depending on the cause of the deficiency.
At a pure platelet loss after profuse bleeding, for example after a traffic accident, are suitable Platelet concentratesthat the patient intravenous, i.e. given into a vein using a needle. The platelet concentrates are obtained from donors in blood banks or blood donation facilities. In some cases it is necessary to find several donors for a patient, because on the one hand the donation amount and donation intervals are limited, on the other hand some patients (mostly Leukemia patients) need large amounts of platelets. The target value is 150,000 platelets per microliter and up.
For operations, it is necessary to increase the platelet count to over 50,000 and possibly even higher, as it becomes extremely difficult for the surgeon to stop any bleeding during the operation - after all, the blood does not clot without platelets.
On the other hand, coagulation can also be disruptive in many cases:
For example, if the patient is at increased risk of his Vessels close. One has to remember that whatever is in a blood vessel that, in its opinion, does not belong there, the body responds to with a platelet reaction. This means, among other things: an artificial heart valve, arteriosclerosis, a metal insert like a Stent, any deposits of fat, damage to the inner wall of the vessel, etc. There is a risk of Blood clot formation, and its replacement and migration into smaller ones Vessels, such as in brain, lung or heartwhich would lead to heart attacks.
To prevent this clumping, there is the very well-known group of Antiplatelet drugs. That means in German that these drugs die Prevent platelet aggregation.
The most famous representative is probably that Acetylsalicylic acid, short ASS, best known trade name "aspirin". This drug is capable of that blood keep fluid and a To prevent accumulation of supposed foreign bodies in the vessel.
One makes use of this with patients high blood pressure, arteriosclerosis and more general Risk of thrombosis by lying down for long periods (in the hospital) or sitting (on a plane, on bus rides). Other known drugs with similar effects but different starting points are Clopidogrel or Abciximab.
Prevention
Most people have blood platelet levels in the normal range and do not require any therapy. An artificial correction of the platelet count can be done in high-risk patients such as long-term Smokers, obese Patient, or a high Cholesterol level be necessary. Usually a prophylactic one is used here Antiplatelet drugs how ASS given in individually dependent dosage.
This keeps the blood fluid, prevents plug formation and prevents the risk of thrombosis.
A well-known non-drug measure are those Thrombosis stockingscompressing the legs. This will make the Pressure on the vessels increased, which speeds up blood flow, and a Prevents blood stagnation.
So as not to let it get that far in the first place, are healthy eating, sufficient physical activity of 2-3 hours a week and waiving risk factors like Cigarettes and alcohol essential.
Platelet donation
The donation of blood platelets (thrombocyte donation) is a procedure similar to the plasma donation, in which 5 to 6 times more Platelets can be obtained from a normal blood donation. When donating, only the platelets are removed from the donor's blood via a “cell separator” and the remaining blood components are returned to the donor. Depending on the device and platelet count, the donation takes between 60 and 90 minutes. Since only a very small part of the blood cells are taken, a platelet donation can be done every 2 weeks in addition to the normal whole blood donation.