Blood sponge
definition
Blood sponges are also known as hemangiomas in medical terminology and are benign tumors.
They develop from the innermost cell layer of the vessels, the so-called endothelium. Ultimately, a blood sponge consists of a growth of tiny vessels and owes its name to the pronounced blood supply.
About 75% of the blood sponges are already present at birth. Premature babies seem to be affected up to 10 times more often than the rest of the population.
The benign tumors are divided into different classes (cavernous, capillary, senile, generalized) and can in principle occur anywhere where blood vessels are present.

causes
The origin and the causes for the occurrence of blood sponges is currently the subject of research. These are blood sponges Vascular malformationsthat arise when vessels proliferate. However, why they do this for some people and not for others is not entirely clear.
Various factors are discussed that can lead to the development of blood sponges:
- One possible aspect that can help is one hereditary component. Blood sponges are not directly inheritable, but they seem certain genes and variations in DNA favor the appearance of blood sponges.
- Other mechanisms must also be involved, as blood sponges, for example, are more likely to contribute Premature babies occur. About 10 times more often they are found in premature infants compared to full term infants.
- Also neoplastic causes are discussed.
With alcohol
There are no evidence that alcohol consumption contributes to the development of blood sponges. However, the following should be noted: Especially during pregnancy, abstaining from alcohol is essential for the child's healthy development. Although no direct connection cause hemangiomas, alcohol should not be handled lightly.
diagnosis
The diagnosis of a superficial blood sponge is usually already through that close observation possible. Blood sponges on the skin are due to the enlarged vessels reddish to purple colored. In your size can you vary. However, they are different from fire marks raised above the skin level and palpable. It's a kind ulcer.
To Assessment of the depth growth of the blood sponge one is suitable Ultrasound examination. This examination is important in helping you decide whether a blood sponge should be treated. With a very large depth of growth, there may be impairments.
Lower blood sponges are usually called Incidental finding recognized in the context of other diseases. A good example of this are Hemangiomas of the liver. These usually fall within the scope of a CT or MRI examination on. In the case of liver hemangiomas, contrast medium ultrasound is also suitable for more detailed diagnosis.
Concomitant symptoms
Blood sponges can show very different symptoms, depending on their location:
- Generally, a blood sponge does not cause symptoms as such.
- Superficial blood sponges on the skin are symptom-free.
- However, very large blood sponges or those on the face can become a psychological burden for those affected. This is why such blood sponges are often removed for cosmetic reasons.
Depending on the location, blood sponges also cause physical symptoms:
- An example of this are blood sponges that lie in the eye socket. As they grow, they can hinder vision and lead to double vision.
- Blood sponges on the lid prevent the eyes from opening and thus also restrict vision.
- Blood sponges found in folds of skin or around the armpits can be tender and cause pain if clothing rubs against them. Bleeding is also possible.
- The so-called cavernomas occupy a special position among the blood sponges. These vascular malformations are usually located in the brain or spinal cord, where they can lead to epileptic seizures or symptoms of paralysis. In the worst case, there is a risk of cerebral hemorrhage.
The cavernous hemangioma is also an important special form of hemangioma. To learn more about it, read: Cavernous Hemangioma - How Dangerous Is It?
Profuse bleeding from blood sponges
Blood sponges can in some cases bleeding profusely. Depending on the size and location of the blood sponge, the risk of bleeding may be increased. In particular, large blood sponges on parts of the body subject to high mechanical stress, such as skin folds or lips, can bleed easily.
A particular risk of bleeding hold so-called Cavernomas of the brain. Cavernomas are also blood sponges. However, these occur specifically in the brain and spinal cord on. In the worst case, cavernomas lead to life-threatening cerebral hemorrhage and can therefore be a surgical removal require.
therapy
How to remove a blood sponge
Exist to remove blood sponges various possibilities. In principle, not every blood sponge has to be removed, but there are often situations in which it makes sense to remove it.
One common method is Laser therapywhich is mainly used for blood sponges on the face or other visible areas. Different lasers are used for removal.
Apart from the laser therapy, there is the possibility of applying flat blood sponges to the skin freeze. This treatment is known as Cryotherapy. Like laser therapy, it can already in infancy be performed.
Furthermore is a surgical removal blood sponges possible. However, surgery is only performed in very rare cases. In particular, blood sponges of internal organs such as the liver or cavernomas of the brain and spinal cord can make an operation necessary. This is always the case when symptoms arise from the blood sponge.
After all, one has existed for a while medical therapy With Beta blockers, which inhibits the growth of the blood sponges so that they disappear in the best case.
laser
Stand for treating blood sponges different lasers to disposal. The external treatment with the laser causes the red blood cells within the enlarged vessels of the blood sponge to be heated. These give the heat to the Vessel wall further which thereby bursts. This is how blood sponges become scaled down, until they eventually disappear.
Very small blood sponges can already a meeting be enough. Require larger blood sponges several sessions for a satisfactory result.
Treatment will carried out on an outpatient basis and requires one for babies and toddlers anesthesiaas they painful is. Basically, the individual pulses of the laser feel like pinpricks. However, adults tolerate treatment well without anesthesia.
For a few hours after treatment, there may be a local itching, slight pain and one Redness come to the affected skin area. A bruise and swelling may appear a few days after treatment, but these will go away in about a week or two. Cool packs help very well against swelling and blue discoloration of the skin. In some cases, light scabs can form on the skin.
Direct sunlight should be avoided during the entire treatment period in order to prevent pigment shifting. The sun should be avoided for up to two months after the treatment is completed. The skin must not be pre-tanned for laser therapy.
Duration
Blood sponges vary greatly in their growth tendency and their course. Some congenital blood sponges form by themselves after some time back. They usually show a growth phase of around 6 to 9 months. A regression usually takes place within the first 10 years of life and cannot be predicted.
However, there are also blood sponges that only appear in adulthood and last a lifetime. Since it cannot be predicted in children whether the blood sponge will regress or not, it is usually removed in toddler age.
Blood sponge in the baby
The most blood sponges in babies kick already immediately after birth on or are innate. Very few forms emerge after the third decade of life. However, contrary to many rumors, the appearance of blood sponges cannot be caused by the behavior of the mother or the child. There is often a misconception that events during pregnancy or childbirth lead to blood sponges in the baby. However, this is not the case. Mothers should therefore not blame themselves if a baby has a blood sponge.
About 3-5% of all newborns have a blood sponge. Premature babies seem to be about 10 times more likely to be affected than full term babies. The reasons for this have not yet been clarified. Blood sponges usually show one within the first year of life Growth tendency. The size varies greatly from child to child and cannot be predicted. Most blood sponges regress and disappear by the age of 10. Because of this tendency towards self-healing, a wait-and-see attitude can be adopted in many cases.
Cause blood sponges as such no complaints to the baby. They can bleed or pain when subjected to mechanical stress. Depending on the location, some blood sponges require treatment. This is the case, for example, when they grow very deeply and thereby impair or displace important structures. These include, for example, large blood sponges near the eyes and the eye socket. Various methods such as laser, cryotherapy or surgical therapy are available for therapy. Recently, drug treatment with the beta blocker propanolol, which can stop the growth of some blood sponges, has also been possible.
You might also be interested in: Stork bite on baby
Blood sponge in adults
Blood sponge in the liver
Often fall at one CT, MRI or a simple one Ultrasound examination blood sponges of the liver of the abdomen as an incidental finding. This is because they usually do not cause any discomfort and are therefore almost never searched for specifically. Up to 20% of the population have blood sponges in their liver - so it is the so-called Liver hemangioma the most common tumor of the liver. Since it is a benign malformation, the liver hemangioma has no potential to degenerate.
Also read our article: Liver Hemangioma- Is It Dangerous?
There are three types of blood sponges in the liver:
- The capillary liver hemangioma (Type 1) is usually very small (about 1-2 cm).
- Cavernous hemangiomas (Type 2), however, are larger and have a lobed structure.
- From a diameter of about 5 cm one speaks of a Giant hemangioma. This mostly belongs to type 3, the characteristics of which are thrombosed and scarred areas.
To confirm the diagnosis of a liver hemangioma, the Contrast medium sonography. There the so-called shows up Iris diaphragm phenomenon. The name is explained by the fact that the contrast agent accumulates from the outside to the inside and thus takes on the appearance of an iris diaphragm. Therapy is basically not necessary. In very rare cases, when the blood sponge causes pain or presses neighboring organs due to excessive growth, it makes sense to remove it.
Blood sponge on the lip
On most parts of the body, blood sponges are not perceived as particularly annoying. The lip is one of the few exceptions. Already in Infancy can cause blood sponges of the lip Be an obstacle to food intake and to complaints to lead.
Smaller blood sponges are mostly not a problem, whereas in particular larger blood sponges in this area bleed easily can. Since the lip is constantly being mechanically stressed by the children, be it by eating, sucking or later speaking, the blood sponge can bleed or hurt easily.
Very large blood sponges in this area may also lead to Deformations on the jaw or the row of teeth. Treatment of such blood sponges is already advisable in infancy and toddler age, since complications threaten, especially with rapid growth. However, the decision must be made individually. In the case of very small blood sponges, you can initially wait, as spontaneous healing can also occur.
Blood sponge in the baby
The most blood sponges kick already immediately after birth on or are innate. Very few forms emerge after the third decade of life. However, contrary to many rumors, the appearance of blood sponges cannot be caused by the behavior of the mother or the child. There is often a misconception that events during pregnancy or childbirth lead to blood sponges in the baby. However, this is not the case. Mothers should therefore not blame themselves if a baby has a blood sponge.
About 3-5% of all newborns have a blood sponge. Premature babies seem to be about 10 times more likely to be affected than full term babies. The reasons for this have not yet been clarified. Blood sponges usually show one within the first year of life Growth tendency. The size varies greatly from child to child and cannot be predicted. Most blood sponges regress and disappear by the age of 10. Because of this tendency towards self-healing, a wait-and-see attitude can be adopted in many cases.
Cause blood sponges as such no complaints to the baby. They can bleed or pain when subjected to mechanical stress. Depending on the location, some blood sponges require treatment. This is the case, for example, when they grow very deeply and thereby impair or displace important structures. These include, for example, large blood sponges near the eyes and the eye socket. Various methods such as laser, cryotherapy or surgical therapy are available for therapy. Recently, drug treatment with the beta blocker propanolol, which can stop the growth of some blood sponges, has also been possible.
You might also be interested in: Stork bite on baby
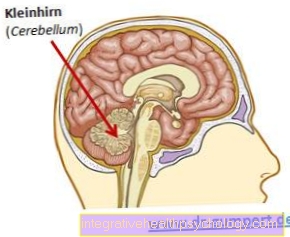
Blood sponge in the head or brain
Blood sponges also rarely appear in the brain. There they are called cerebral cavernomas designated. The information on the frequency of cerebral cavernomas varies widely in the literature, so that an exact statement is difficult to make. The frequency is probably somewhere around 0.7 to 4% the population.
she consist from a Interweaving of enlarged capillariessurrounded by a capsule. These vessels are also known as caverns. Most cavernomas occur for no apparent cause, but some will inherited.
About 80% of the brain's cavernomas are in one of the two Cerebral hemispheres, around 15% can be found in the Cerebellum and Brain stem.
Only about half of the cavernomas cause symptoms and are thus clinically apparent. In most cases, the findings are incidental. Cavernomas can cause a wide variety of symptoms. These depend primarily on the location of the cavernomas. It can epileptic seizures or even Signs of paralysis occur. The symptoms of paralysis affect different parts of the body depending on the location of the cavernoma. Usually cavernomas are developed as part of a MRI or CT examination of the head discovered. Cerebral cavernomas that appear symptomatically are surgically removed if possible. If the findings are asymptomatic, a wait-and-see attitude is adopted.
Blood sponge on the face
The face represents one frequent localization for congenital blood sponges. The distribution on the face can be very different, as can the size. Since most blood sponges go away on their own by the age of 10, treatment is not always necessary. Flat blood sponges in particular that do not grow in depth are not a problem. Only one cosmetic impairment can exist due to the good visibility on the face.
It makes sense to remove it if the blood sponge shows no tendency to heal itself, but continues to grow.
There are also blood sponges of the face, the one health impairment represent. Above all, this includes blood sponges strong in depth to grow. This can become a problem, especially around important structures such as the nose or eyes.
Large blood sponges the Eyelids or Eye sockets hinder vision and can cause disturbances, such as a Squint or Double vision, cause. At the nose there is a risk of obstructing breathing or deforming the nose.
Furthermore, blood sponges of the lips or mouth are potentially problematic if they have the Ingestion or that Impede speaking. In these cases in particular, therapy is very useful. Which method is most suitable is a decision on a case-by-case basis.
Blood sponge in the head or brain
Blood sponges also rarely appear in the brain. There they are called cerebral cavernomas designated. The information on the frequency of cerebral cavernomas varies widely in the literature, so that an exact statement is difficult to make. The frequency is probably somewhere around 0.7 to 4% the population.
she consist from a Interweaving of enlarged capillariessurrounded by a capsule. These vessels are also known as caverns. Most cavernomas occur for no apparent cause, but some will inherited.
About 80% of the brain's cavernomas are in one of the two Cerebral hemispheres, around 15% can be found in the Cerebellum and Brain stem.
Only about half of the cavernomas cause symptoms and are thus clinically apparent. In most cases, the findings are incidental. Cavernomas can cause a wide variety of symptoms. These depend primarily on the location of the cavernomas. It can epileptic seizures or even Signs of paralysis occur. The symptoms of paralysis affect different parts of the body depending on the location of the cavernoma. Usually cavernomas are developed as part of a MRI or CT examination of the head discovered. Cerebral cavernomas that appear symptomatically are surgically removed if possible. If the findings are asymptomatic, a wait-and-see attitude is adopted.
On the spine and spinal cord
Blood sponges can also appear in the spine - to be more precise in the spinal cord - but they are very rare there. They are called cavernomas. Why cavernomas occur in some people and not in others is largely unclear. Hereditary factors seem to play a role in this context.
Cavernomas in the spinal cord can lead to symptoms such as paralysis, pain or impaired sensitivity. Most of the time, they are discovered incidentally during a CT or MRI examination. Often they do not cause any symptoms. The nature of the symptoms of a blood sponge in the spine depends on its exact location. The symptoms come about because the blood sponge presses on nerve fibers. In certain cases, surgical removal is possible and necessary, for example if paralysis occurs. Cavernomas that do not cause any symptoms, however, do not require acute treatment.
Read more on our website Hemangioma on the spine
On the testicle
True are Blood sponges on the testicles rarely, but they do occur every now and then. In principle, they are not a cause for concern. As blood sponges are benign malformations of the blood vessels, they do not pose an acute risk to health.
If a child has a blood sponge on their testicles, first of all be awaitedwhether this disappears by itself after a while. However, an examination by a doctor is useful to assess how far the blood sponge grows in depth. Very deep blood sponges can cause damage and removal is therefore usually sensible in such cases. The parents and the treating physician then decide together which procedure is most suitable.












.jpg)