Lyme disease
Synonyms
Lyme disease, borreliosis, Lyme disease, Lyme arthritis, erythema chronicum migrans
English: borreliosis
definition
Lyme disease is one bacterial diseasewhose transmission by the stitch of a Shield tick he follows. The consequences of the infection range from simple skin symptoms to neurological symptoms and what is known as Lyme arthritis. Borreliosis was first observed in 1975 in the small town of Lyme in the US state of Connecticut and as a Lyme arthritis (Lyme-Joint inflammation) has been described.
In contrast to that which is also transmitted by ticks TBE (Early summer meningo encephalopathy), a viral disease, you cannot vaccinate yourself against Lyme disease! However, she is with Antibiotics (Drugs that kill bacteria) easily treatable.
Epidemiology
Lyme disease cases are only notifiable in the new federal states, the incidence (this means the number of new cases per year) can therefore only be approximated 30.000 - 50.000 Estimate cases per year. Borreliosis is thus much more common than that TBE.
According to the Robert Koch Institute, after a tick bite, 1.5 to 6% of those affected are likely to have a Borrelia infection, but this does not always lead to symptoms. See also Tick bite.
Tick borreliosis (Lyme borreliosis) is a disease that is caused by a tick bite. It is assumed that, depending on the area, around 5 - 35% of the ticks are the causative agent, more precisely Borrelia burgdoferi bear in themselves.
Pathogen / transmission path

The causative agent of the borreliosis disease, the bacterium Borrelia burgdorferi, belongs to the spirochete family and has the ability to survive in the tick's intestines. It gets into the human bloodstream through the tick bite. Borrelia can be extracellular (outside the body cells) lie protected between connective tissue fibers or intracellularly in phagocytes (Resource cells / immune cells) survive, so that they can persist for a long time in the host (Borrelia carrier) "undetected" by the immune system. In addition, the borreliosis bacteria have the ability to "camouflage" themselves. Once the body's own defense system has identified the bacteria as a foreign body and has begun to defend itself, the Borrelia change their surface so that they can be separated from the antibodies (the body's own defense substances; see immune system) can no longer be recognized.
Is Lyme Disease Contagious?
Borreliosis is basically not contagious.
At least human-to-human transmission has never been detected or observed. The transmission takes place exclusively through blood contact between the tick and humans.
Read much more information about the risk of infection through blood or in pregnancy at: Is Lyme Disease Contagious? and Tick bite during pregnancy
Symptoms of borreliosis
Second stage:
The main symptom for this stage is a burning pain emanating from the nerve roots (radicular). It can be observed that this pain is concentrated in the vicinity of the wandering redness or the tick bite.
It is an inflammatory reaction that mainly affects nerve roots. affects the cranial nerves. In addition, meningitis can be caused by the pathogen (meningitis), which can lead to neck stiffness, headaches and other neurological failures.
After the name of the discoverer, this is also called Bannwarth syndrome or meningopolyneuritis.This can occur weeks to months after the infection by the tick. In addition to this characteristic pain, paralysis also occurs due to the inflammation of the nerve root by the borreliosis pathogen. These are mainly to asymmetrical paralysis, ie. only one side fails and not both.
Since the roots of the cranial nerves are often affected, facial muscles fail. The cranial nerve called the facial nerve is most frequently affected. This nerve primarily supplies the facial muscles, which are responsible for our facial expressions.
Affection of the heart walls can occur much less frequently. Depending on which layer of the heart wall is inflamed, this is called myocarditis, pericarditis or pancarditis. This can lead to cardiac arrhythmias by affecting the pacemaker systems of the body.
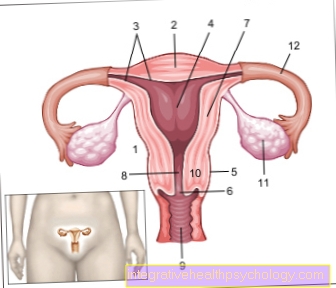
Another rarer symptom at this stage is that Lymphadenosis cutis benigna. This is a blue-reddish colored soft knot or raised area. The cause of this lump is the invasion of white blood cells (Lymphocytes) into the skin through the Borrelia infection. Common locations of this benign nodule are the earlobes, neck, armpits, genital area and nipples.
Please also read our article on this Neuroborreliosis can be recognized by these symptoms.
Third stage:
At this stage, painful inflammation of the joints and muscles can also occur (Arthritis and myalgia). This inflammation can jump from joint to joint or from muscle to muscle. This stage occurs months to years after the tick bite.
Joint inflammation, also known as Lyme arthritis, is often chronic, relapsing and can occur in one or more joints. The knee joint, then the ankle, elbow, finger and toe joints, wrist joints and temporomandibular joint are most commonly affected.
Acrodermitis chronica trophicans is another typical picture of the disease at this stage. This is characterized by a dark bluish discoloration of the skin and very thin skin. In the course of the disease, the bluish discoloration of the skin appears first, which may be a little swollen. However, there is no triggering of complaints. This leads to a steady decrease in the subcutaneous fat tissue and thus to a strong reduction in the thickness of the skin. This results in the skin vessels showing through. In addition, the skin can harden due to the formation of fibers (fibrosis) in the skin. Preferably this occurs on the fingers and extensor sides of the limbs. Furthermore, joints and nerves can also later after the occurrence of the Acrodermitis chronica trophicans to be affected.
Please also read our article on this Rash and joint pain
Enzphalomyelitis is a very rare form of Lyme disease. This is characterized by paralysis of one or both extremities.
diagnosis

The diagnosis of an infection with Borrelia burgdorferi is made by the detection of antibodies in the patient's blood and the results of the examination. For more information, see Lyme Disease Test.
Overall, it is difficult to recognize Lyme disease. As mentioned earlier, months to years can pass between each stage, making it difficult to see all symptoms in context. All you have to do is think about when you last felt like you had the summer flu and whether you would think about it if you went to the doctor with joint pain. Most symptoms of Lyme disease are very unspecific and can also be triggered by a number of other diseases. To make matters worse, there are a large number of "atypical courses" in which there are only a few or even only one of the symptoms mentioned.
Antibody detection can be used in every stage of Lyme disease, but then it has different success rates. Especially in the early stages of Lyme disease, antibody formation can only be detected in 10% -40% of cases. In the late stage, the antibodies are practically always detectable, although here too there are isolated cases in which the examination of the blood remains “silent”.
Even if the antibodies are detected in the blood, this result is only of limited use, since it can also be an "old, healed" infection.
Basically, two types of antibodies can be detected: antibodies of the IgM type show the early infection (usually stage I of Lyme disease or else symptomless) while antibodies of the IgG type show the late infection (stage II + III) or an infection that was a long time ago, which may be completely healed. For antibody detection there are the simpler screening tests, such as the so-called ELISA test and the more complicated confirmatory tests such as the immuno-blot or western blot test, which give you the certainty that the test was not false positive. This means that in order to determine a current or past Borrelia infection, you should initiate a confirmation test if the search test is positive so that you can really be sure that anti-Borrelia antibodies have actually been detected.
The amount of antibody detection (Titer) is of little value for diagnosis.
Lyme disease test
First of all, it has to be said that a Lyme disease test is only carried out if there is reasonable suspicion. Certain symptoms that indicate the disease are suspected.
The most common and gold standard of tests is a cerebral fluid test, which is also called a CSF puncture. A hollow needle is used to pierce the lumbar vertebral area and nerve fluid is removed. It is important to ensure that the work is sterile, as otherwise infections can be carried over into the spinal cord and brain, which can lead to Encephalitis (Encephalitis) or too Meningitis (meningitis) can lead. In addition, it must be punctured sufficiently far down in the lumbar vertebra area (approximately between the third or fourth lumbar vertebrae) so as not to injure the spinal canal.
However, a blood test must also be carried out.
Now the values of the antibodies against the borreliosis pathogen in the blood and in the brain water are compared with each other. One can use the antibodies of the Immunoglobulins M or G (IgM and IgG) measure up. The antibodies differ in that the antibodies IgM in the event of an infection increase first and IgG only after a longer period of time, when the disease has become chronic.
A certain ratio of antibodies in the blood and nerve water is calculated.
This ratio, which is calculated, is also called CSF serum index or specific antibody index. The ratio should be below 2, everything above this indicates an increased number of antibodies against the Lyme disease pathogen in the brain water and thus a Lyme disease disease.
Recognize Lyme disease
The Lyme disease recognizing is sometimes more difficult than expected.
It can happen that Lyme disease is only recognized in its later stages, because those affected do not address one Tick bite and remember typical symptoms or they were not characteristic. The problem is that the condition can sit in the body for years with no symptoms before it breaks out again.
In order not to overlook Lyme disease, one should try to recognize the infection in its early stages. The most common symptom and early symptom that a visual diagnosis can represent is the Wandering redness. Typically this is also with fever connected. Wandering redness is a reddening that is surrounded by a circular, ring-shaped reddening that occurs at the point where the tick stung. They are also called Erythema migrans.
The erythema migrans must not be associated with the Granuloma annulare, a benign non-infectious skin disease. Raised papules form here, whereas in Lyme disease there is a ring-shaped reddening around the bite site.
Find out more about the topic here: Granuloma annulare
Should you recognize the redness just described and possibly even a Tick bite remember, you should definitely consult a doctor!
Other very characteristic symptoms are the asymmetrical paralysis of the Facial nerves, especially of the facial nerve and a Meningitis. Here too, a possible Borrelia infection must be considered immediately!
Other unspecific symptoms of Lyme disease can also Joint pain, prolonged fatigue, skin inflammation and Flu symptoms occur in borreliosis.
In the case of long-lasting joint pain that does not respond to treatments or skin inflammations that cannot be classified, one should also consider Lyme disease in its later stages as the cause.
More signs
Other signs that can be seen in the cerebrospinal fluid are an increased number of white blood cells, an increased content of protein, an increased lactate level (Lactic acid) and a reduced sugar content in the brain water. These parameters indicate a bacterial infection and are therefore initially not specific for the Borreliosis infection. In contrast, the above-mentioned antibody detection is more decisive.
It must be said that this test, which is often used as the gold standard, can lead to false negative results in a Lyme disease diagnosis, ie. there is an infection but no antibodies have been produced by the body and the test would not indicate an infection. It is therefore very important not to overlook the clinic of the person concerned. Despite a negative test, typical symptoms such as the wandering redness come for a treatment!
In addition, the Borreliosis test can still be used years after the tick bite.
In the case of joint pain with inflammation, on the other hand, you can also perform a joint puncture and thus use the growth of the bacteria after the sampling as evidence.
If the tick is on site, which is usually not the case after removal until symptoms appear, you can test whether the borreliosis pathogen can be detected in the tick. The tick has to be sent to a laboratory. If the tick is infected, this does not mean that the person bitten was also infected.
However, the longer the tick bites on the body, the greater the likelihood of transmission. It is therefore important to remove the tick as soon as possible if it is noticed. Since the infected tick and the patient have to be retrained, this is a more complicated method.
- Further tests are the LTT test (lymphocyte transformation test):
Certain white immune cells (lymphocytes) are detected that are specific for surface proteins (antigen) of the borreliosis pathogen.
After the blood has been taken, the lymphocytes are centrifuged off and separated from the other cells in the blood. Then the antigen of the Borreliosis pathogen and the nutrient solution are added and a culture of the lymphocytes is made. By adding a radioactively labeled amino acid for DNA production, the thymine, one can observe whether the lymphocytes are specific for an antigen on the borreliosis pathogen.
What is criticized about the test, however, is that there are still many false positive and false negative results. Ie. both infected persons are not recognized and non-infected persons are incorrectly measured as infected. On the one hand, this is due to the fact that the test is very complex and demanding. The test is also relatively expensive.
- There is also the CD-57 test.
Here it is said to have been established that an infection with Lyme disease results in an altered immune defense.
This indicates, for example, a lower number of natural killer cells in Lyme disease.
The CD-57 surface protein is located on activated natural killer cells. And it is precisely these that should be particularly reduced in the case of a Borreliosis infection. So you can detect the reduction of these cells through the surface protein. A blood sample is also taken for the Lyme disease test. Here, fluorescence-marked (Substances that trigger a light reaction) Antibodies against the CD-57 antigen were brought into contact with the blood sample, thus providing evidence. However, false positive or negative results can also occur here. This can be the case that the natural killer cells are reduced by another disease or the immune response can be very variable.
- The latest test in the field of borreliosis diagnostics is the Spirofind test.
Defense cells called monocytes are examined. After contact with the borreliosis pathogen, these should react more quickly to the pathogen than the first time. Here, the monocytes are filtered out of the blood sample and brought into contact with the borreliosis pathogen. However, the method is still in research and its efficiency has yet to be clearly proven in studies.
Lyme disease therapy summary
Is the Lyme disease diagnosed needs treatment with Antibiotics respectively. Drug therapy usually works well for this disease. Problems arise from the necessary, individually very different dosage and the duration of therapy, which makes it necessary to take the respective antibiotic over a period of two to four weeks. Borreliosis is treated differently depending on the stage of the disease, this is known as "Stage-appropriate" treatment.
A Lyme disease can manifest itself in different localizations of the organism, so that a Lyme disease therapy can represent an interdisciplinary task in which doctors from different disciplines are involved.
In general, the disease can be broken down into three stages divide which are also taken into account in Lyme disease therapy. One is decisive for the further course of the disease antibiotic therapy early in the morning, because a longer pathogen infestation makes a complete elimination of the pathogen from the organism more difficult.
The failure of antibiotic therapy in the early stage is only around 10% and rises to around 50% in the late stage, which again illustrates the importance of an early start of therapy.
In the early stages of Lyme disease, antibiotics are usually used Doxycycline and Amoxicilin used, but they are only two examples of a variety of preparations that can be used to achieve an optimal therapy for the patient. Reasons for exclusion for certain active ingredients must be observed, such as the presence of a Renal failure or the patient's age, to name but two.
In the later stage of Lyme disease it will mostly Ceftriaxone prescribed a cephalosporin antibiotic.
Therapy stage 1 borreliosis
in the Stage I., which is caused by the characteristic round reddish rash, the so-called wandering redness (Erythema migrans) is embossed around the puncture site of the tick, an antibiotic is applied Lyme disease treatment for two weeks with:
- Doxycycline (a tetracycline)
or - Amoxicillin (an aminopenicillin)
What is relevant is that Doxycycline because of his Storage in bones and teeth not for children under the age of 8 given, as otherwise bone growth is impaired, tooth enamel is underdeveloped and the teeth are yellowed.
For these reasons, amoxicillin is used in children under the age of 8. In case of non-response to the carried out antibiotic Lyme disease treatment the antibiotic should be exchanged for another.
Therapy stage 2 and 3
In more advanced stages like that Stage II and the Stage III come first of all the antibiotics Ceftriaxone and Cefotaxime for use.
Ceftriaxone and Cefotaxime are Cephalosporins of group 3a and have an extremely broad spectrum of activity.
Borreliosis therapy with cephalosporins of group 3a must last for three to four weeks be performed.
It is administered intravenously, i.e. the injection takes place directly into a vein.
In stage II and III, other antibiotics are currently used in addition to the group 3a cephalosporins listed above.
Other Antibiotics can represent an alternative in Lyme disease therapy, as it is being discussed that group 3a cephalosporins do not have sufficient effect against Borrelia, which are present in the cells, and also promote the formation of cystic Borrelia, which are difficult to combat with drugs.
If there is another treatment after antibiotic Lyme disease Flare-ups of the disease, so this is done again with a another antibiotic cycle treated.
What should be considered during the treatment?
During the antibiotic treatment a weekly blood sample should be taken at the beginning to check the small blood count and others Laboratory parameters respectively
In the following, a check every 2-3 weeks is sufficient. One complication that can occur with antibiotic Lyme disease treatment is the so-called Jarisch-Herxheimer reactiondue to massive bacterial kill at the start of treatment.
From the killed Borrelia become bacterial toxins, so-called endotoxins are released, which then cause a counter-reaction in the body.
Our organism releases inflammatory mediators that lead to:
- high fever
- chills
- a headache
- Muscle pain (myalgia)
- Joint pain (arthralgia)
and - fatigue
being able to lead. In extreme cases it can even lead to one Circulatory shock come. If these symptoms occur, immediate treatment is required cortisone displayed in hospital.
Prophylactic cortisone intake before taking the antibiotic can be useful for certain risk factors after consultation with the treating doctor.
In the case of long-term Lyme disease therapy with an antibiotic, the intake of Probiotics to the Protection of the intestinal flora be considered. On the one hand, there are foods that contain probiotic bacteria, such as probiotic yogurt. There are also probiotic medicines.
According to studies, taking these probiotics is said to reduce the occurrence of Diarrheathat can occur as part of antibiotic therapy.
prophylaxis
A vaccinationhow it is against them TBE disease there (see also Vaccination against meningitis), is not available for Lyme disease in Europe, but intensive research is being carried out in this area and the first results of this work are being tested in the USA. Still for that It is not expected that a vaccine will hit the German market in the near future.
To the often tedious, not always successful and with Side effects connected Lyme disease therapy to work around it is recommended Tick bites as best possible to prevent, because one too Vaccination sometimes doesn't exist.
As follows, staying in the bushes and tall grass should be avoided or only carried out with protective clothing.
After a tick bite, a so-called Post exposure prophylaxis be performed. Post-exposure prophylaxis is a measure taken after someone has been exposed to an infection risk to prevent the infection from actually breaking out.
In the event of a tick bite, the patient would one-time use of the antibiotic doxycycline receive. The execution this measure is common in medical circles, however controversial and is used in Germany due to the low risk of infection of about 2% after a tick bite not recommended.
The best protection is therefore still the so-called Exposure prophylaxis.
This means avoiding tick bites by avoiding tick-rich areas, or using insect-repellent creams, sprays, etc.
Lyme disease and wandering redness
The Wandering redness is a very common but also a very characteristic symptom of Lyme disease. About 60-90% of those infected with Borreliosis show a form of wandering redness. The wandering redness usually develops 10-30 days after the tick bite appeared. However, it occurs after 7 days at the earliest. The wandering redness is also painless.
It is a reddish spot or a reddened elevation, which can be sharply delimited and rounded-oval. This reddening is now spreading outwards in a ring-shaped manner.
This leads to a central pale after some time, so that a ring-shaped reddening occurs. The reddened bite of the tick is often still in the center. There is no flaking of the skin or an open lesion to the outside due to the wandering redness. It must be noted that the expression of the wandering red can be very different. In most cases, the wandering redness heals automatically after about 10 weeks. However, it can also occur repeatedly. This is particularly the case with children, but on average only in 5-10% of those affected.
It also happens that the wandering redness is so discreet that it is not even recognized or noticed by those affected. In children, wandering redness can have peculiarities such as manifestations in the head and neck area or even fleeting redness in the facial area
Fever and flu-like symptoms are also frequent accompanying symptoms of wandering blush.
The cause of this skin reaction is an immune reaction in the body. Immune cells such as lymphocytes and plasma cells flow into the skin. This leads to reddening of the area.
Is Lyme Disease curable?
In relation to cure The experts argue about Lyme disease.
Especially in the past it was assumed that in late stages and above all in very pronounced cases, a cure is only possible to a limited extent. For the stadiums I and II everyone agrees that complete healing is ensured through treatment. Recently, however, many experts have assumed that Lyme disease can also be cured in its late stages. It was found that in many cases the healing only worked after a second or third attempt at treatment