Inflammation of the mammary gland while breastfeeding
introduction
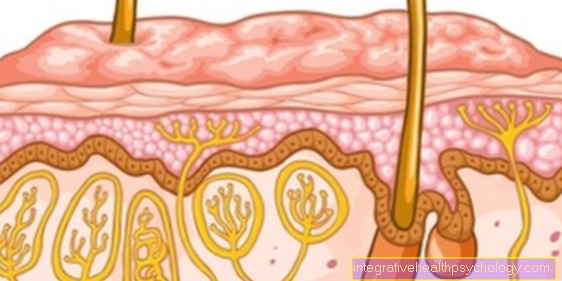
The breast inflammation during breastfeeding will also Puerperal mastitis called. According to the definition, it occurs exclusively during breastfeeding, while breast inflammation outside of breastfeeding is referred to as mastitis non puerperalis. It is an acute inflammation of the glandular tissue of the breast, triggered by a congestion of the milk secretion or an infection with bacteria. It often occurs about two weeks after delivery and can be diagnosed with a clinical exam or an ultrasound. The therapy depends on the cause and ranges from simple cooling of the area to antibiotic therapy.

causes
Mammitis can be caused in two ways. On the one hand, an infection with a bacterium can trigger the clinical picture described. Most often it is an infection with Staphylococci. Due to inadequate hygiene measures, these are transferred from the mother or the hospital staff to the nasopharynx of the infant, which then brings the bacteria into close proximity to the mother's breast when breastfeeding. The pathogen can either get directly through the nipple into the milk ducts and trigger inflammation there, or it enters the lymphatic system via the smallest injuries to the breast and causes the inflammatory reaction from there. In addition to the infection, a build-up of the milk secretion can also lead to an inflammation of the mammary gland, as the secretion builds up in the milk ducts and can cause inflammation there with pain and hardening. Reasons for the build-up of the milk secretion are insufficient emptying of the breast during breastfeeding, increased swelling of the mammary glands after childbirth with the consequence that the breast can only be emptied with difficulty or an inadequate milk donation reflex when the child is placed on the breast, for example can be disturbed by pain or stress.
Further information on the subject can be found here: Milk congestion
Diagnosis of mastitis during breastfeeding
The diagnosis of mastitis is usually made through a clinical examination. Attention is paid to the typical local signs of inflammation (see accompanying symptoms), which are often associated with fever. To distinguish whether inflammation of the mammary gland is an initial stage with diffuse inflammation (Phlegmon) or at an advanced stage with encapsulated inflammation (abscess), a palpation examination or ultrasound can be helpful. An abscess can be felt as a circumscribed mass that can be easily impressed. On ultrasound, the abscess shows up as a dark, almost black mass, while diffuse inflammation shows no typical signs on ultrasound.
Concomitant symptoms of mastitis
The mammary gland inflammation is characterized by local reddening, swelling and overheating of the affected area. In addition, indurations can be felt, which can be so painful that an examination of the breast is hardly possible. The pain and swelling make breastfeeding or expressing the milk secretion difficult, which is an important part of the therapy. Swelling of the lymph nodes in the armpit on the same side is also typical. In contrast to mastitis non puerperalis, inflammation of the mammary gland is regularly associated with a fever> 38 ° C and a pronounced feeling of illness during breastfeeding.
Therapy of mastitis
The most important pillar of therapy is regular breastfeeding or expressing the milk secretion in order to eliminate the cause of the inflammation. Weaning is usually not necessary and does not show any advantage for the course of the disease. The pain can be treated locally with cooling, which is particularly useful after breastfeeding. Heat can be used before breastfeeding or pumping to facilitate emptying of the breast. If complete emptying is still not possible, hardened areas in which milk secretion has remained can be smoothed out manually. Painkillers that are approved for breastfeeding can be given to relieve the pain. This is, for example, paracetamol, which can be taken up to four times a day, or ibuprofen up to three times a day, but which should only be taken for short periods of time. If the inflammation of the mammary gland is bacterial, it is recommended to take an antibiotic. In advanced stages and if the above measures have not led to an improvement, milk production can be reduced or inhibited with medication, for example with the prolactin inhibitor bromocriptine. In any case, an abscess should be emptied either with a puncture or a small incision and the remaining cavity should be thoroughly rinsed.
You may also be interested in the following articles: Drugs for breastfeeding, painkillers for breastfeeding
Therapy with home remedies
Home remedies can be particularly effective in local therapy. Before breastfeeding, an application with heat can help to mobilize the milk secretion, for example with a warm shower. Let the warm water hit your chest directly. An alternative to water is the use of a red light lamp. For local cooling after the breast has been emptied, quark compresses, compresses with natural honey or ice packs are ideal. A white cabbage leaf in the bra can also produce even and pleasant cooling and also has a positive effect on the milk ducts by helping to remove the underlying milk blockage. When cooling, care should be taken that the time intervals are not chosen too long in order to avoid effects on the circuit. In addition, the chest can be immobilized as much as possible with a tight bra, which can have a positive effect on the course of the inflammation. Various household remedies can also be used to influence milk production. For example, drinking at least two cups of hibiscus, peppermint, or sage tea a day can lead to decreased milk production. As with any other acute inflammation, in addition to specific measures, attention should be paid to enough rest and sufficient fluid intake in order to provide the body with the best possible support in fighting the inflammation.
Homeopathy for an inflammation of the mammary gland
Homeopathy knows many remedies against inflammation, so only a selection can be mentioned here. One of the main remedies is belladonna, which can be helpful in acute inflammation with development of fever. Arnica, the most popular wound healing agent, can have a positive effect on initial pain and swelling. In severe and sharp pain, especially in the case of tremors, Bryonia can bring about a relief of the pain, it is also one of the main remedies. Phytolacca or Pulsatilla are indicated if the pain is radiating to the shoulder and neck. They also work against negative mood changes when breastfeeding or expressing.
You might also be interested in these articles: Belladonna, Arnica
When do i need an antibiotic?
In general, it can be said that an antibiotic is indicated if it is a bacterial inflammation of the mammary gland. In clinical practice, an antibiotic should be prescribed if conservative measures such as breast emptying, application of heat and cold have not shown any improvement after 24-28 hours. The administration of antibiotics only makes sense in the early phases of the disease, which is why an early search for the cause is essential. So-called antibiotics are the first choice Penicillinase-resistant penicillins, such as flucloxacillin or cephalosporins.
Duration of mammary inflammation during breastfeeding
As a rule, the inflammation of the mammary gland heals completely within a short time with local measures. There can even be spontaneous healing without any therapy. If an antibiotic has to be taken, the symptoms usually subside very quickly. If an abscess has already formed, this can extend the healing time, as it has to be emptied with a puncture or a small incision, so that the wound must also heal. Compared to breast inflammation outside of breastfeeding, recurrent inflammation and chronification occur less frequently during breastfeeding.
What effects does breast inflammation have on my child?
As a rule, the child can continue to be breastfed during the breast infection, since the risk of infection for the child is very low. It is even beneficial for the course of the disease, as regular emptying of the breast is an important therapeutic measure. Premature babies should be diagnosed with a bacterial cause mastitis not be breastfed any further and also with an infection B streptococci the newborn should no longer be breast-fed. In the event that the child should also show symptoms of inflammation, antibiotic therapy must be started for the mother and the child.