The dorsiflexion weakness
What is dorsiflexion weakness?
Dorsiflexion weakness describes a disorder of the extensor muscles of the lower leg. This consists of the tibialis anterior muscle (anterior tibial muscle), the extensor digitorum longus muscle (long toe extensor) and the extensor hallucis longus muscle (long big toe extensor).
The task of the muscles is to lift the foot or toe, which is where the term “foot lifter” comes from. A dorsiflexor weakness can have various causes, which can mainly be traced back to a restricted nerve function or, more rarely, to deficits in the muscles, joints and tendons.
Lifting the foot is part of a wide variety of motion sequences, as well as normal gait. Therefore, weakness leads to enormous restrictions in the patient's life and should be treated as best as possible.

The reasons
A common cause of dorsiflexion weakness is a stroke. This leads to a destruction of brain matter, which can also affect the centers and nerve tracts that are responsible for movement. The result is that the subordinate nerve cords in the spinal cord and those that are directly connected to the muscle can no longer be controlled by the brain. The muscles become weaker or even completely paralyzed.
Other central neurological diseases, such as multiple sclerosis, damage brain tissue, which can lead to similar symptoms.
If the cause is not central, the nerve flow can also be disturbed on another level. For example, a herniated disc often results in a narrowing of the spinal cord, which can also pinch the motor nerve fibers.
Serious injuries to the legs (especially knees and ankles) or during operations can result in direct nerve damage.
The development of nerve tumors (so-called neurofibroma) may also impair the function of the affected nerve.
Even after the correct treatment of a leg injury - for example a fracture - the nerve can still be damaged: if the plaster of paris is applied too tightly and not relieved, there is a risk of external pressure damage.
In addition to the nervous system, the causes of an existing dorsiflexion weakness can also be looked for in the musculoskeletal system itself. Injuries to the muscles and tendons, chronic joint changes such as osteoarthritis or inflammation (arthritis - joint inflammation, myositis - muscle inflammation) can temporarily or permanently restrict the foot lifter function, depending on the cause.
You can read more information on the subject here: arthrosis
Dorsiflexion weakness after a herniated disc of the lumbar spine
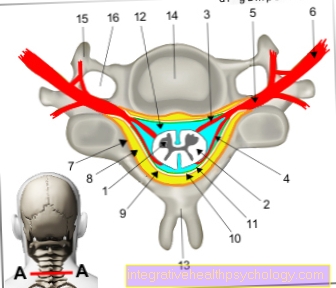
The most common disc herniation occurs in the lumbar spine (lumbar spine) area. The intervertebral disc (a small cartilaginous cushion between the vertebral bodies) protrudes into the vertebral canal, which can displace the spinal cord and impair its function.
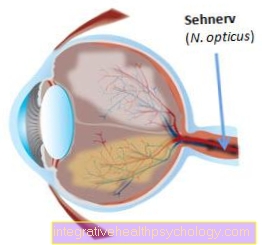
The nerve cords, which are responsible for the movement control of the legs and feet, run at the level of the lumbar spine. This is where the commands from the brain are passed on to the muscles. The nerve that controls the foot lift is called the deep fibular nerve. Its fibers leave the spinal cord at the level of the 4th and 5th lumbar vertebrae. Then they pull in a thick bundle of nerve fibers, the sciatic nerve (sciatic nerve), through the thigh to the lower leg.
When it leaves or above its exit point, the nerve can be affected by the herniated disc. Depending on the severity of the incident, the result is weakness or even paralysis of the lower leg extensor muscles.
Muscle weakness and movement disorders are not uncommon symptoms of a herniated disc and are usually accompanied by severe pain and abnormal sensations (tingling, numbness). A combination of surgical and physiotherapeutic measures may be necessary to treat dorsiflexor weakness.
Find out all about the topic here:
- Herniated disc L4 / 5
and - Herniated disc of the lumbar spine.
Appointment with ?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
Athletes (joggers, soccer players, etc.) are particularly often affected by diseases of the foot. In some cases, the cause of the foot discomfort cannot be identified at first.
Therefore, the treatment of the foot (e.g. Achilles tendonitis, heel spurs, etc.) requires a lot of experience.
I focus on a wide variety of foot diseases.
The aim of every treatment is treatment without surgery with a complete recovery of performance.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Dorsiflexion weakness after hip surgery
Hip surgery is a major surgical procedure that is regularly performed in surgical clinics. In Germany, for example, over 240,000 hip prostheses are used every year.
A risk during the interventions is the damage to nerve tracts, since the operating area is anatomically close to a wide variety of neural structures. The nerves supplying the gluteal muscles (gluteal muscles) are most at risk.
In the depths, under the gluteal muscles, the sciatic nerve runs out of the pelvis and contains the fibers that control the foot lifters. He continues to squat on the back of the thigh. With a variable course, adhesions or carelessness on the part of the operating doctor, the nerve cord can be injured in such a comprehensive operation (such as hip surgery). The resulting dorsiflexor weakness can be accompanied by other symptoms - this depends on the extent of the damage to the nerve.
More information on the topic can be found here: Hip prosthesis
Dorsiflexion weakness after a stroke
A stroke causes blood vessel blockage or bleeding in the brain. The affected areas determine the severity of the symptoms.
If the cerebral cortex is affected where the center of movement is located, this will lead to disturbances. The opposite side of the damage is always restricted, as the nerve pathways for movement cross to the other side on their way to the muscle.
A dorsiflexor weakness on the right therefore suggests a stroke in the left hemisphere and vice versa.
Stroke is one of the most common reasons for dorsiflexor weakness or dorsiflexor paresis. Paresis, in turn, is a characteristic symptom of a cerebral infarction. The course of the restriction of movement depends largely on rapid treatment and early training of the muscles as part of the rehabilitation measures.
Read more on the subject here Stroke.
Dorsiflexion weakness due to MS
Multiple sclerosis (MS) is a chronic inflammatory nerve disease. In this disease, what is known as demyelination occurs: the covering substance of the nerve cells in the brain and spinal cord is increasingly lost, which slows down or even impedes the transmission of stimuli.
The impairment of nerve function affects a wide variety of organ systems, as well as movement. For this reason, dorsiflexion weakness can occur in the course of the disease. There are various forms of multiple sclerosis.
The condition can appear in stages with (partial) regression of the symptoms or it can progress continuously. According to this, the dorsiflexor weakness can regress if it occurs during an episode of illness.
Since there is unfortunately no therapy for MS yet, it can only be slowed down in its development. As a result, any dorsiflexor weakness can only be treated to a limited extent.
Find out more about the topic here Multiple sclerosis.
Concomitant symptoms
Dorsiflexion weakness is often accompanied by other symptoms. Depending on the cause of the muscle weakness, other nerve tracts or elements of the musculoskeletal system can also be affected by the damage.
If it is a far-reaching impairment of nerve tissue, this can manifest itself in abnormal sensations such as tingling, pain or numbness. In the case of a stroke, there are also often restricted mobility of the arm on the same side, paralysis of facial muscles or language problems. If the dorsiflexor weakness can be traced back to a herniated disc, there is usually also severe pain at the vertebral level, which radiates into the affected leg.
In the case of inflammation in the area of the leg, characteristic features such as reddening, swelling, overheating and local pain can be found. Direct mechanical injury to the muscles or nerves causes severe pain and bleeding.
diagnosis
The diagnosis of dorsiflexion weakness can be made relatively easily. The examiner determines the force with which the patient can lift his feet.
A scale from 0 to 5 is used, ranging from complete paralysis (0) to normal strength and movement control (5). A distinction can also be made as to whether the movement can still be carried out against resistance (4), against gravity (3) or with the removal of gravity (2). Muscular activity that can be felt, but without active movement (1), can also be recorded.
If the diagnosis is to be saved, an EMG (electromyogram) can also be requested. Needles are inserted into the muscles to be examined and the conduction of excitation is measured. In this way deficits can possibly be represented.
The treatment options
The treatment of dorsiflexion weakness depends entirely on the cause. The aim of therapy should be to restore the nerve to function as completely as possible. If this is no longer possible due to extensive damage, complications such as malpositions (e.g. equinus) and the breakdown of surrounding muscle groups must be prevented
If the dorsiflexion is weak due to direct nerve damage or severance, the chances of recovery are relatively poor. Attempts can be made to join the nerve endings back together with a seam, but this only rarely leads to success.
Physiotherapy is the main focus of therapy for dorsiflexion weakness. On the one hand, the surrounding muscles should be strengthened so that they can take over the functions of the impaired muscle groups; On the other hand, the foot lifters should be exercised in order to prevent the muscle tissue from regressing and to improve the function of the nerve through regular stimulation.
Furthermore, splints can be placed on the foot and lower leg, which bring the foot into a stable position and thereby make walking much easier. Functional electrical stimulation (FES for short) is another treatment option: It takes over the function of the nerve by directly stimulating the muscle and causing it to contract. It can also train muscles that have been completely separated from the nerve supply. The activation also has an effect - as with physiotherapeutic exercises - on the restructuring of the supplying nerve and promotes healing.
Which track can help?
When using splints with an existing dorsiflexion weakness, various principles can be used. There are various mechanical aids that help the patient to stabilize the ankle and thus make walking easier. The splints can be adapted to the degree of weakness of the foot dorsiflexion.
With only slight restrictions, the splint can only include the ankle joint, for example.
If there is a severe weakness or even paralysis, more comprehensive measures are necessary. As a rule, a base plate under the sole is firmly connected to a bracket that is attached to the lower leg by means of straps. In addition to the mechanical principle, splints can also be used, which make use of functional electrical stimulation (FES). The splint is a band attached to the lower leg, which contains electrodes for electrical stimulation and activates the muscles from the outside through the skin.
When choosing the right splint, the patient's wishes must be addressed individually and the likely healing process (as well as the prognosis) taken into account.
The foot orthosis
Orthoses are externally attached aids that are intended to enable the patient to maintain a healthy posture and movement. The group of orthoses also includes the term “splint”, which is found more frequently in linguistic usage
If the foot is weak, various orthoses can be used, which are mainly adapted to the degree of muscle weakness. If it is a matter of a slight weakness in the dorsiflexion of the foot, an ankle orthosis (splint or bandage) is sufficient. This is put on like a stocking and helps the patient to stabilize the ankle while walking.
If there is already a tendency to develop a deformity (e.g. equinus foot) or if the dorsiflexor weakness is very severe, other foot orthoses can be used. These usually have a base plate on which the sole of the foot rests. A fixed guide connects the base plate with a belt or bandage that is attached to the lower leg. This prevents the foot from folding down while running and promotes natural movement.
The orthosis can often be worn under clothing, which increases comfort for the patient.
For more information read: Orthosis for the foot
The electrotherapy
In functional electrical stimulation (FES) - a form of electrotherapy - electrodes are attached to the muscles from the outside. The electrodes cause the muscles to contract through electrical stimulation. In this way, the muscles are tensed and thus trained, although they have no or only inadequate contact with their supplying nerves. As a result, FES can slow down or even stop the regression of the muscles. Furthermore, the resulting movement of the foot can be used to make walking easier for the patient.
Another important point is the declining excitation of the damaged nerve. Regular activation can promote a new network of nerve cells if there is no serious damage to the tissue. Thus, under certain circumstances, the functionality of the nerve can be restored and the dorsiflexor weakness cured.
Read more on the subject here Electrotherapy
The kinesio tape
Kinesio tapes are self-adhesive, elastic tapes that are applied directly to the skin and used for a wide variety of diseases. Its effectiveness has not yet been scientifically confirmed, but "taping" still has a large following. It is primarily intended to provide help with muscular problems and diseases of the musculoskeletal system.
If the foot is weak, the tape is applied in two layers. The course begins at the inner edge of the foot and leads over the back of the foot to the area of the outer ankle and the outer lower leg.
The tape should thus fulfill a holding function and give stability to the foot that drops when the foot is weak. In addition to their normal training, many physiotherapists also qualify for the correct handling of kinesiotape, which is why the application should be carried out by such specialists.
Find out more about the topic here: Kinesio tape.
What other resources can help?
Other aids can also support the patient in everyday life. First of all, you should always pay attention to sturdy and safe shoes. Since the patient has already lost stability due to the weakness of the foot dorsiflexion, the right shoes help to stabilize the gait and prevent stumbling caused by the ground.
There is also the possibility of using walking aids. The options range from walking sticks and crutches on both sides to a rollator. Since the aids are sometimes perceived as stigmatizing, information should be given about the possibility of using orthoses or FES (functional electrical stimulation).
If there is severe weakness in the dorsiflexion of the foot or even paralysis of the corresponding muscles, which cannot be compensated for by any other aids, it may be necessary to use a wheelchair.
In everyday life, further technical equipment can then be used that can guarantee independent supply (e.g. (stair) lifts in multi-storey buildings.
Which exercises can help?
In most cases, the exercise of the foot lift is instructed by trained physiotherapists. Nevertheless, there are some exercises that can also be carried out at home in order to maximize the success of the therapy.
Here, the training can slowly be built up from minimal load until more intensive exercises can be performed. First, for example, you can begin to pull your toes towards your head while lying or sitting. During the exercise, the muscles are only slightly stressed and used without the influence of gravity. At the beginning, an additional person can support the movement with their hands if the patient cannot build up enough strength.
Increasing the exercise would be performing from a standing start. The toes can initially be lifted slowly, while the aim is to drum the toes on the ground more quickly. While sitting, the exercise can be intensified by using a latex strap. The foot is inserted into a loop and the two ends are fastened. Now the toes can be pulled towards the head against increased resistance.
Another exercise is lifting objects with your toes. Not only the foot lifters, but also the rest of the muscles in the foot are used, which promotes stabilization. The heel gait is also a way to train the foot lifters, but is probably only possible at the end of the training due to the muscles that have been built up by then.
Is a dorsiflexor weakness curable?
Whether or not an existing dorsiflexion weakness is curable depends heavily on the cause of the disorder.
If the nerve has been irritated by pressure damage, the chances of complete healing are good. Such pressure damage can result, for example, from incorrect posture or incorrect positioning when bedridden.
A dorsiflexor weakness in the context of a stroke has a poor prognosis with a lower chance of recovery. The function of the nerves and the affected muscles can often be improved through intensive training - however, weakness usually remains. However, through the use of aids such as functional electrical stimulation (FES), a persistent deficit can be compensated for with promise.
The lowest chances of recovery exist with direct mechanical (or traumatic / accident-related) damage or destruction of the nerve tissue. Treatment options for severing nerves are very limited and surgical interventions rarely lead to therapeutic success. The result is permanent functional impairment or even paralysis.
Duration of healing
The various therapy options for dorsiflexor weakness take different amounts of time.
In the case of pressure damage due to incorrect posture or incorrect positioning, the weakness of the foot dorsiflexion can subside after a few days if the nerve tissue has not suffered any serious damage.
However, if the muscles and nerve tissue have to be trained again, this can take a few weeks to months. Depending on the severity of the damage and thus also the weakness of the dorsiflexion of the foot, the training program is adjusted by the treating doctors and physiotherapists so that progress can be made as quickly as possible. In some cases, the training has to be carried out for years to counteract a regression of the muscles. Splints (or orthotics) or functional electrical stimulation (FES) are also long-term therapeutic measures, which, however, hardly lead to any restrictions in the everyday life of the patient.
It is also not uncommon for skills believed to be lost to be regained after a long period of time through continuous and persistent training.
Further information
Read more information about dorsiflexion here:
- Foot disorders
- Inflammation of the foot
- Herniated disc in the lumbar spine
- Palsy of the foot
- Electrotherapy
- Kinesitherapy
You can find an overview of all orthopedic topics under: Orthopedics A-Z.