Common illnesses during pregnancy

The most common illnesses during pregnancy include:
-
Genital Infections
-
Asymptomatic bacteriuria
-
Cystitis
-
Urinary obstruction
-
Moles
-
Placental insufficiency (placenta weakness)
-
Placenta previa
-
Too much or too little amniotic fluid
-
High blood pressure in pregnancy
-
Gestational diabetes
-
Pregnancy anemia
Infectious diseases

Asymptomatic bacteriuria
Asymptomatic bacteriuria is found in around 5-8% of all pregnant women. This means that bacteria can be detected in the urine, but they do not cause any problems for the pregnant woman.
E. coli, an intestinal bacterium, is the most common.
Asymptomatic bacteriuria is treated with antibiotics during pregnancy because it can lead to ascending infections such as kidney inflammation or infection of the child during birth.
Cystitis
Cystitis during pregnancy causes symptoms such as a burning sensation when urinating, the need to urinate frequently, and frequent passing of small amounts of urine.
The most common pathogen is the intestinal bacterium E.coli. But other bacteria can also cause cystitis.
Depending on the pathogen, different antibiotics are used.
Find out more about the topic here Cystitis During Pregnancy.
Pelvic inflammation
Acute renal pelvic inflammation occurs in about 1% of pregnant women and is the result of cystitis or asymptomatic bacteriuria.
Typical symptoms are high fever with chills, flank pain, burning sensation when urinating, and frequent urination. Possible complications are blood poisoning (so-called. sepsis), premature birth and irreversible damage to the kidney.
Renal pelvic inflammation must therefore always be treated with antibiotics, which are administered in high doses via a venous access at the beginning of therapy.
Read more on the subject here Pelvic inflammation.
Circulatory diseases

High blood pressure in pregnancy
High blood pressure occurs in 6-8% of all pregnancies and is classified on the one hand according to when it occurs and on the other hand according to the level of the blood pressure.
Mild pregnancy hypertension exists when the blood pressure is above 140/90 mmHg, but below 160/110 mmHg. Severe pregnancy hypertension exists at values above 160/110 mmHg.
It is important to check the blood pressure values regularly in order to start drug treatment in the event of repeated values above 160/100 mmHg.
However, not all medications may be administered during pregnancy, e.g. Alpha-methyldopa, metoprolol, and nifedipine.
The loss of protein via the kidneys is also checked regularly by examining the urine with a test strip. This is used to identify preeclampsia, another form of hypertensive (high blood pressure) pregnancy disorders.
In preeclampsia, in addition to high blood pressure, there is a loss of protein in the urine. If the protein loss is very high, water can accumulate in the tissue (so-called. Edema).
The dangerous special forms of this disease include eclampsia and HELLP syndrome, which are colloquially known as "pregnancy poisoning".
Eclampsia affects less than 0.1% of pregnancies and HELLP syndrome about 0.5%. Both diseases only appear after the 20th week of pregnancy.
Eclampsia not only results in high blood pressure and protein loss in the urine, but also in the mother having seizures. The HELLP syndrome describes a complex of hemolysis (breakdown of red blood cells), high liver values and low platelet counts (blood platelets). Affected pregnant women often have headaches and / or flickering eyes and complain of upper abdominal pain.
Ultimately, both diseases can only be treated by terminating the pregnancy through delivery of the child. In individual cases, depending on the condition of mother and child, it must be weighed how far the pregnancy can be extended.
Find out more about the topic here High blood pressure in pregnancy.
Varicose veins in pregnancy
Pregnancy slows the return of blood from the lower half of the body. This increases the pressure in the venous system. Expanded veins develop (so-called. Varices) that snake on the surface of the skin.
These varicose veins develop in 30% of primiparous women and 50% of multiparous women. These affect the legs and genital area. Hemorrhoids are also possible.
Typical symptoms are heavy and tired legs with water retention, nocturnal restlessness in the legs, a feeling of heat and leg cramps. 80% of pregnancy-related varicose veins regress within a few weeks after giving birth. The treatment of varicose veins takes place with compression stockings, which improve the return of the blood from the legs.
You can find out more about the topic here Varicose veins in pregnancy.
Pregnancy anemia
Anemia describes anemia and is associated with hemoglobin values below 10g / dl (normal value 12-16g / dl). A slight drop in the hemoglobin value is perfectly normal during pregnancy, as the increase in blood volume leads to a thinning effect despite the increased formation of red blood cells.
Anemia during pregnancy causes the following symptoms: paleness, shortness of breath during exercise, fatigue, fast heart rate, ringing in the ears, headache and frequent freezing.
At the end of pregnancy, up to 30% of pregnant women are affected by pregnancy anemia, which in most cases is triggered by an iron deficiency, as the need for iron is increased during pregnancy. In the event of iron deficiency, iron stores can be replenished during pregnancy by giving iron supplements. The iron therapy must be carried out 3-6 months after reaching a normal hemoglobin value.
A certain form of anemia (called megaloblastic anemia) is triggered by a lack of folic acid. Because folic acid deficiency in children leads to increased occurrence of Spina bifida (open back) and cleft palates, women of childbearing age are recommended to take 0.4 mg of folic acid daily before the start of pregnancy, which should be continued during pregnancy.
Read more on this topic at: Iron Deficiency During Pregnancy
Vena cava compression syndrome
The pressure of the uterus on the inferior vena cava (Vena cava) the blood from the lower half of the body is more difficult to transport back to the heart. This leads to a relative lack of volume in the cardiovascular system and can even increase to shock.
Typical symptoms are nausea, paleness, sweating, dizziness and restlessness. Vena cava compression syndrome is particularly pronounced when lying on your back or standing. Most pregnant women have no symptoms when lying on their side. About a third of all pregnant women are affected.
Pregnant women, with or without compression syndrome, should avoid lying on their back, especially in the last third. The compression also reduces the flow of blood to the child and, as a result, does not receive enough oxygen.
Find out more about the topic here Vena cava compression syndrome.
Hormonal changes

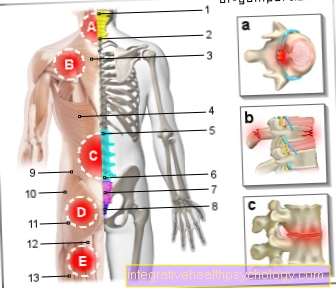
Urinary obstruction
Two thirds of all pregnant women have different types of urinary congestion. In most cases, the ureters and renal pelvis are affected.
The cause lies on the one hand in the hormonal change that causes the ureters to widen, and on the other hand the growing uterus presses on the ureters.
In most cases, the urinary congestion is only slight and does not cause any symptoms. But it can also promote kidney inflammation.
If the kidneys are severely congested, the drainage can be improved by inserting ureteral splints. Urinary congestion usually resolves within 3 months of birth. If this is not the case, further clarification should take place.
Gestational diabetes
Gestational diabetes describes the first occurrence of a diabetic metabolic condition during pregnancy and does not refer to type 1 or type 2 diabetics whose disease was known before pregnancy.
Due to the hormonal changes, the sugar concentration in the blood increases during pregnancy. At the same time, the release of insulin (one of the main hormones in sugar metabolism) is increased because the pancreas produces more of it. However, if the extent of the increased sugar concentration exceeds the ability of the pancreas to produce insulin, gestational diabetes occurs.
This disease makes urinary tract infections and preeclampsia more common. The disturbed metabolic situation also has a negative effect on the unborn child. The children are very often "macrosomal" (very large) with a birth weight of over 4 kilograms. The malformation rate increases with poorly adjusted sugar values. Developmental disorders are also possible, especially of the lungs and liver. Other effects include excessive amniotic fluid and increased rates of premature births and fatalities in the womb.
In order to identify as many pregnant women with gestational diabetes as possible, the urine is checked for sugar during the preventive examinations and, in cases of doubt, an OGTT (oral glucose tolerance test) is carried out.
The treatment of gestational diabetes consists of an appropriate diet, exercise and sport. Insulin therapy may have to be started if these measures are not sufficient.
Read more on the subject here Gestational diabetes and glucose tolerance test during pregnancy
Thrombosis in Pregnancy
The hormonal changes during pregnancy increase the tendency of the blood to form clots. This is why the number of leg vein thromboses or pulmonary embolism increases during pregnancy.
The risk is six times higher than that of a non-pregnant woman. About 0.13% of pregnancies are affected by a thromboembolic event.
The treatment is carried out by inhibiting blood coagulation using heparin, which is not passed on to the unborn child via the placenta.
Read on here: Thrombosis in Pregnancy.
Anatomical malformations

Moles
The mole represents a vesicular malformation of the chorionic villi, which actually serve to ensure the exchange of substances between mother and fetus. Chorionic villi are cells of the placenta (placenta) which have protuberances in order to enlarge the surface.
The mole of the bladder occurs in one out of 1,500 pregnancies and causes the following symptoms: vaginal bleeding in early pregnancy, pronounced nausea, significantly enlarged uterus, pregnancy poisoning and breathing disorders.
The treatment involves a complete scraping of the uterus.
Placenta previa
A placenta previa describes an incorrect position of the placenta after the 24th week of pregnancy, the placenta lies entirely or partially in front of the inner cervix. The frequency is 0.5% of all pregnancies.
If the inner cervix is completely closed by the placenta, a caesarean section must be performed. If the placenta previa only touches the inner cervix at the edge, no normal delivery attempt should be made.
The symptom of placenta previa is painless bleeding, which occurs mainly in the last trimester of pregnancy and, depending on the extent, can be very dangerous for mother and child. If there is a bleeding of the placenta previa, the pregnant woman is admitted to the hospital and closely monitored.
Depending on the age of the pregnancy and the degree of risk for mother and child, delivery is carried out by caesarean section or drugs are administered to control the bleeding.
Read here on the topic: Diseases of the placenta.
Other diseases

Placental insufficiency
Placental insufficiency, also known as placental weakness, affects about 2-5% of all pregnancies. It can arise either acutely or slowly and describes a dysfunction of the mother cake with a decrease in the ability to supply the child with nutrients. It can occur at any stage of pregnancy.
Acute placental insufficiency occurs with permanent contractions of the uterus, a knot in the umbilical cord, bleeding of the placenta, or pregnancy poisoning.
Chronic uterine weakness is often caused by diseases of the mother (e.g. high blood pressure, diabetes, collagenosis), by maternal smoking or by infectious diseases.
The consequences of a placenta weakness can be the death of the unborn child, growth retardation or an early release of the placenta. An ultrasound examination of the unborn child and the blood vessels that supply the placenta and child with blood can determine the extent of placental insufficiency and determine the best time to give birth.
Depending on the cause of the mother cake weakness, a different approach is required.
Calcification of the placenta also often occurs towards the end of pregnancy. These can only be determined by means of an ultrasound examination. They are often natural and harmless. Read more about this under: Calcified placenta
Find out more about the topic here: Diseases of the placenta.
Too much or too little amniotic fluid
Too much amniotic fluid Polyhydramnios) occurs in up to 3% of all pregnancies; too little amniotic fluid (oligohydramnios) in up to 7%.
Too much amniotic fluid has no cause in 60% of the cases, in 20% of the cases the mother suffers from diabetes mellitus and in up to 20% of the cases the child has malformations that can affect the digestive tract, for example.
Too much amniotic fluid can cause labor, a feeling of tightness in the abdomen, or shortness of breath. The therapy of polyhydramnios depends on the cause; an early delivery may have to be carried out.
Too little amniotic fluid in the last trimester of pregnancy may have been caused by an early rupture of the bladder or indicate the onset of placental insufficiency. The prognosis for insufficient amniotic fluid in the last trimester of pregnancy is good. However, if there is a lack of amniotic fluid earlier, this can be an indication of malformations of the urinary tract in the unborn child.
If the bladder ruptures prematurely, the pregnancy should be extended up to a maximum of 34 weeks in order to keep the risk of infections or compression of the umbilical cord lower than the risk of premature birth.
Find out more about the topic here Amniotic fluid.