Cervicobrachialgia
Synonyms
Cervicobrachialgia, neck and arm pain, radiculopathy, nerve root pain, back pain, lower back pain, lumbar syndrome, root irritation syndrome, compression syndrome, herniated disc, facet syndrome, vertebral joint pain, myofascial syndrome, tendomyosis, spondylogenic reflex syndrome (cervical spine, spinal column)
Definition of cervicobrachialgia
Cervicobrachialgia is not a diagnosis of illness, but the description of a decisive and pioneering sign of illness, the in the poor forward cervical spine pain.
Cervicobrachialgia is the most common expression of one Herniated disc of the Cervical spine (cervical spine).

Terminology
Cervicobrachialgia is made up of the terms cervicalgia = pain in the cervical spine and brachialgia = arm pain transmitted via the nerve roots and arm nerves.
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Causes of cervicobrachialgia
Cervicobrachialgia can have several underlying causes. By far the most common cause of disease is a herniated disc in the cervical spine (cervical spine). The herniated disc tissue in the direction of the spinal cord leads to chemical and mechanical irritation of the nerve roots. This causes nerve root pain (radiculopathy), which continues along the affected body nerve (peripheral nerve) into the body. Depending on which nerve root / which arm nerve is affected by the damage, the pain band along the arm can differ (see above dermatome distribution).
There is a connection between the strength of a nerve root irritation and the extent of the pain in the arm. The stronger and the more sudden the irritation (stimulus) of the nerve root, the further the pain is transmitted along the affected body nerves into the arm. Very strong nerve root irritations lead to arm pain up to the hand, less severe and slowly developing nerve root irritations lead to arm pain that can break off in the upper or lower arm. Typically, the patient experiences neck-arm pain caused by a herniated disc more in the arm than in the cervical spine.
Less common causes of cervicobrachialgia are wear-related narrowing of the nerve exit holes in the spine (degenerative spinal disease), vertebral joint cysts or inflammation of the body nerves themselves (neuritis / plexus neuritis).
Cervicobrachialgia is to be distinguished from pseudoradicular pain. This refers to simulated nerve root pain that can be caused by various diseases (e.g. cervical spine syndrome). Pseudoradicular cervical spine pain also radiates to the arm or neck area, but never reaches the hands and cannot be assigned to any nerve root. The following diseases can cause pseudoradicular cervical spine pain:
- Facet syndrome / spondylarthrosis
- Uncarthrosis (form of cervical spine osteoarthritis)
- "Blockages" of the cervical spine joints
- Muscular tension (myogelosis)
Symptoms
Complaints caused by cervicobrachialgia are mostly all in one constant or epoch-making pressure on the nerves of Cervical spine justified. The nerves running along the cervical spine pull into the area of the poor. Complaints come in the form of strong ones depending on their severity a headache that radiate into the cervical area.
These can be pulling or dull, knocking in character. They can sometimes be triggered by manual pressure on the cervical spine, which makes them worse. Most of the time they are not permanent, but they can gain in strength, especially during long periods Lying phases or after getting up in the morning. Even after long Car trips there may be a severe headache in the area. In addition to the headaches and the sometimes very severe ones Neck tension Pain in one or both arms is usually described in parallel. This pain is described as pulling and extremely uncomfortable. Also in places Numbness can come to light with a correspondingly severe course.
Cervicobrachialgia and headache
Strength a headache are the most common symptom of cervicobrachialgia. Since the nerves of the cervical spine are stimulated by constant pressure, the pain spreads from the head, into the neck area and into the arms. The pain is particularly felt after periods of inactivity, for example after getting up in the morning or staying in a sitting or lying position for a long time.
The pain is often described as pulling and throbbing and has something of the character of a migraine-like pain. In addition, the pain is described more in the back of the head, which allows conclusions to be drawn about damage to the upper cervical spine. In the therapy of cervicobrachialgia, above all the pain is reduced, which is mainly due to the so-called "NSAIDs“Happens, for example ASS, Ibuprofen and Diclofenac.
diagnosis

The symptoms described by the patient and the physical examination are groundbreaking.
Typical of cervicobrachialgia is the radiation of pain along a dermatome (see above). The most common nerve root irritations of the cervical spine caused by a herniated disc affect the nerve roots C6 and C7.
C6 syndrome
From the intervertebral disc or a Herniated disc C5 / C6 with training a Cervicobrachialgia C6 / C7 At 36%, most herniated discs come from. The sensitive skin supply area of the affected nerve root C6 (dermatome of C6) extends over the upper arm and forearm on the thumb side to the thumb itself. Sensory disturbances and pulling pains in this area are clearly assigned to this nerve root.
When the C6 syndrome is fully developed, the biceps reflex and radius periosteal reflex are weakened or extinguished. In addition, there is a loss of strength when actively flexing the forearm.
Read more about these symptoms at:
- Cervicobrachialgia C6 / C7
and - Herniated disc C5 / 6
C7 syndrome
The C6 / C7 herniated disc is almost equally in second place in terms of frequency with 35%. The dermatome of the C7 root extends over the shoulder and upper arm to the central forearm on the extensor side and into fingers 2-4 (especially the middle finger). Symptoms can be a sensory disturbance in this area, as well as a muscular weakness of the upper arm extensor muscles (triceps) with failure of the triceps reflex. Another characteristic is stunted muscles of the ball of the thumb, which in turn must be causally differentiated from carpal tunnel syndrome.
Read more about this at: Herniated disc of C6 / 7
Magnetic resonance imaging (MRI) of the cervical spine is best suited if the root pain is to be proven in imaging procedures. It can be used to make the nerve roots of the spinal cord and any herniated discs visible.
Further information on this topic can also be found at: MRI of the cervical spine
therapy
The therapy depends entirely on the cause of the cervicobrachialgia. Above all, it is important to have an adequate one Pain therapy to be carried out in order to exclude corresponding bad posture due to the painful course. There are mainly pain relievers that are next to pain reliever also anti-inflammatory Have an effect. That would be mentioned here non-steroidal anti-inflammatory drugs, such as. Ibuprofen or Voltarenthat can be taken. In addition to pain treatment, there can also be a muscle relaxing Medication to be carried out. Here, mainly drugs come from Benzodiazepine type for use. It is important, however, that these drugs are only used for a certain period of time, as the drug group has a not insignificant amount Dependency potential disposes. You can also supplement and accompany physiotherapeutic measures which are mostly aimed at strengthening the muscles of the cervical spine. Cooling or warming Measures on the cervical spine can be tried, but are usually only of limited effectiveness. The use of Ruff should only be used in acute conditions, as they relieve the neck muscles so much that they can degenerate over time. In very severe cases you can try to get through operative interventions to bring about an improvement.
Operation of cervicobrachialgia
Treating a Cervicobrachialgia depends on the cause and the extent of the complaints a person has.
Usually one tries to relieve the pain with the help of Medication or other conservative methods to alleviate. Only if this does not succeed or if the symptoms are very pronounced at the beginning, the doctor will suggest one surgery The advantages and disadvantages of course always have to be weighed up, and in the end the patient is the one who has to make the decision.
Most procedures are not high risk and of course, as with any surgery, there are some dangers such as infection of the wound or problems posed by an general anesthetic can result
There are various options for the treatment of cervicobrachialgia as operations.
If they are through a Herniated disc of the cervical spine caused, you can remove the herniated part. If the mass that previously pressed on the nerve is no longer there, the pain may decrease if the nerve was not previously permanently damaged.
If it is necessary to remove a large part of the vertebral body, it may be necessary to insert a vertebral body prosthesis.
Another option to treat cervicobrachialgia is the so-called Spinal fusion, in which two or more vertebral bodies are to be restricted in their mobility to one another, which can be done, for example, with the help of screws. This will make the Spine stiffer, which can help relieve the pain, for example, if it is caused by wear-related instabilities or deformities, such as the Scoliosis, came about.
In addition, one can widen the exit holes of nerves that for some reason do not have enough space, this is known as Foraminotomy or Decompression.
Generally, however, it has to be said that the results of surgical interventions that are used to treat a Cervicobrachialgia are used, have a rather low success rate, as they only rarely improve the pain in the long term or even make it disappear and therefore represent a disappointment for many patients who decide to do so.
Massages for cervicobrachialgia
Many patients with cervicobrachialgia or chronic pain in the spinal column area are prescribed massages and experience them. However, massages are not very sustainable for such pain conditions.
The therapy of cervicobrachialgia itself must treat the causes, although massage is rarely helpful. The second aspect is pain therapy, which is done through pain reliever and anti-inflammatory drugs.
Massages are more of the complementary physiotherapy treatments. Massage is very pleasant and relaxing for the patient. The muscles can relax briefly and the pain is reduced.
Pain therapy is important in cervicobrachialgia so that the pain does not cause the patient to adopt relieving or bad postures and trigger other painful ailments.
Similar to cooling and warming measures or neck braces, massages have a complementary effect here, but are not a sustainable therapeutic measure. The patient should therefore weigh himself up whether massages are a sensible measure for him.
Exercises
Whether and to what extent special exercises are useful in cervicobrachialgia depends primarily on the underlying cause of the symptoms. If the cause is a degeneration of the spine in the neck area, exercises can only achieve a limited improvement.
Read more on the topic: Degenerative spinal disease
Acute symptoms due to muscle tension or the blockage of individual joints can be improved with the help of certain exercises. In addition to a relaxing massage, which is best performed by a physiotherapist, exercises can help to strengthen the muscles in the affected area.
In consultation with the attending physician or physiotherapist, the following exercises can help to alleviate the symptoms: In the prone position, the arms are held in a 90 ° position by the body, while the palms of the hands are against the floor. The face also points to the ground. Now lift your head off the floor and lift your arms for a few seconds. In the second exercise, you sit on a chair and put your head back. Now the chin is stretched towards the ceiling by your own muscular strength. This exercise can be repeated several times. Stretching the individual muscle groups on the neck and shoulder can also provide relief from the symptoms of cervicobrachialgia.
homeopathy
As with many other clinical pictures, the use of homeopathic remedies is enjoying increasing popularity in cervicobrachialgia. Examples of possible remedies that are supposed to help with cervicobrachialgia are, for example, Cimicifuga, Nux vomica, Bryonia, Ledum or Arnica. It should be noted, however, that there is currently no scientific basis that homeopathic remedies help to improve the symptoms of cervicobrachialgia. The use of homeopathic remedies should therefore always take place in consultation with the attending physician and in addition to conventional therapy.
Find out more about the topic: homeopathy
Cervicobrachialgia and osteochondrosis
Under one Osteochondrosis one understands a chronic disease of wear and tear Vertebral bodies and the Intervertebral joints.
The likelihood of developing osteochondrosis increases with age, as the natural wear and tear over the years can damage the intervertebral joints. Anything that strongly compresses and stresses the elastic intervertebral discs increases the risk of wear and tear, be it from long periods of sitting and little movement or from hard physical work.
The intervertebral discs lose their elasticity in the long run and can no longer cushion the movement between the vertebral bodies optimally. The bone adapts to the situation and forms small bony processes, so-called "Spondylophytes". Because the bones of the individual vertebral bodies are now closer together, there is bony wear, one arthritic change.
The development process takes months to years. The pain also occurs only sporadically at the beginning, with longstanding osteochondrosis there is persistent back pain that can spread to the arms and legs. The earlier treatment for osteochondrosis is started, the sooner more can be done degenerative changes in the spine prevent.
Chronic cervicobrachialgia
If the cervicobrachialgia cannot be adequately treated or does not respond to therapy, the symptoms can become chronic. One speaks of chronification if the symptoms persist for more than three months. In this case you should contact a pain clinic / pain therapist.
Duration of cervicobrachialgia
The duration of cervicobrachialgia varies too much to be able to give a general and always valid statement. Above all, the causes that lead to the symptoms are relevant for the duration of the cervicobrachialgia. The duration of the symptoms can be very long, especially when the causes cannot be eliminated by therapy, as is the case with degenerative changes in the cervical spine. In other cases, such as muscle tension in the neck or shoulder, the symptoms can get significantly better after a few weeks or even days.
The duration of the complaints can be shortened with the help of good pain therapy and appropriate physiotherapy. It is also advisable not to seek medical advice until the symptoms have lasted for days or weeks, so that the symptoms can be prevented from becoming chronic.
Read more on the topic: Therapy of cervicobrachialgia
incapacity for work
Basically, cervicobrachialgia is a very common clinical picture, which in many cases leads to a temporary inability to work.Depending on the individual cause of the symptoms and the individual healing processes, this can take several weeks or even months. The aim of the attending physician and physiotherapist is to ensure that the person concerned is able to work as quickly as possible. If a degeneration of the spine is the cause of the problem, retraining may be necessary, depending on the job.
Anatomy of the cervical spine
On its way to the end of the spine, the spinal cord releases one pair of nerves each floor (Spinal nerves). After leaving the spinal cord, but still in close proximity to it, this spinal cord nerve becomes a Nerve root newly interconnected (new nerve cell). From there a spinal cord nerve (ramus ventralis), which between two Vertebral bodies (Movement segment) emerges from a space provided for this purpose (intervertebral hole) to the right and left of the spine, into the body.
Very soon after leaving the spine, the spinal cord nerves unite to form large body nerves (peripheral annoy). As such, they hug their arms and legs and send and receive all kinds of information.
The spinal cord nerves 4-8 in the cervical spine and the 1st spinal cord nerve in the thoracic spine are responsible for supplying the arms with nerves. These spinal cord nerves combine outside the spinal cord into 3 large body nerves.
- Radial nerve (radial nerve = radial nerve).
- Median nerve (middle nerve = median nerve).
- Ulnar nerve (ulnar nerve = nervus ulnaris).
The tasks of the nerves include above all the control of reflex and muscle activities as well as feeling and pain perception.
Thanks to intensive research, we now know exactly how the individual nerves run in the body, which skin area and which muscle are supplied by which body nerves or which nerve roots. For this reason, with a certain complex of complaints (radiation of pain, loss of feeling, Muscle weakness or paralysis) it can be predicted which body nerve or which nerve root is affected by the damage.
If there is one Herniated disc of the cervical spine or any other major nerve damage with corresponding characteristic failure symptoms, the doctor can thus determine the location of the nerve damage or the damaged nerve. A number of technical investigation procedures are available to support him (MRI of the cervical spine (magnetic resonance imaging), neurological nerve function measurements, e.g. Measure the Nerve conduction velocity (NLG)).
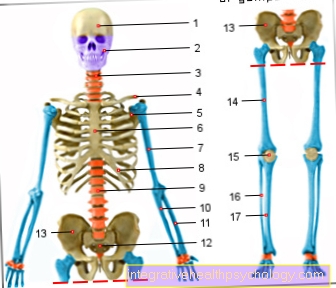
Illustration of the cervical spine
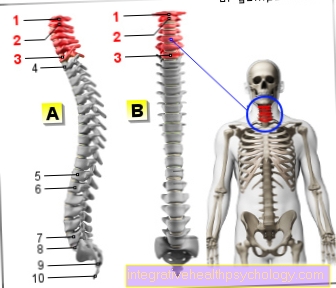
Cervical spine (red)
- First cervical vertebra (carrier) -
Atlas - Second cervical vertebra (turner) -
Axis - Seventh cervical vertebra -
Vertebra prominent - First thoracic vertebra -
Vertebra thoracica I - Twelfth thoracic vertebra -
Vertebra thoracica XII - First lumbar vertebra -
Vertebra lumbalis I - Fifth lumbar vertebra -
Vertebra lumbalis V - Lumbar cruciate ligament kink -
Promontory - Sacrum - Sacrum
- Tailbone - Os coccygis
You can find an overview of all Dr-Gumpert images at: medical illustrations
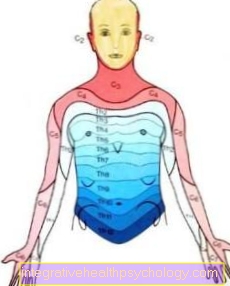
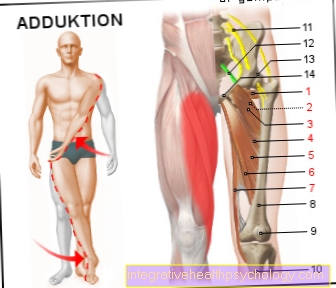
Dermatome
One nerve each for the right and one for the left side of the body supplies a very specific area of the body that is characteristic of these nerves (dermatome; see illustration e.g. C5 = 5th cervical spinal nerve root).
Based on the numbness of certain areas, specific conclusions can be drawn about the affected nerve root.