The physiotherapeutic therapy concept for fibromyalgia
Note
This topic is a continuation of our Fibromyalgia topic.
Physiotherapy / physiotherapeutic therapy concept
- information
- Detailed assessment of the findings
- Passive treatment
- Active therapy
- Ev. Group offers
information
At the beginning of the treatment there should be a detailed information talk about the clinical picture and the course of the physiotherapeutic treatment, in order to explain the connections and behavior patterns to the patient and to relieve him of the fear of the treatment.
Since, in addition to the physical complaints, the psychological situation of the patient also plays an important role in fibromyalgia, the structure of one plays an important role Relationship of trust between patient and therapist an important role. The success of the treatment essentially depends on the fact that the patient feels personally addressed and has the feeling that the treatment is individually tailored to his symptoms and that his pain and problems are taken seriously. There is one interdisciplinary cooperation of the physiotherapist with the doctor and psychotherapist is very important (see multimodal treatment concept).
Without an accompanying drug treatment (chronic pain picture) the Physiotherapy / physiotherapy do not achieve sufficient pain relief, but which is the prerequisite for active therapy. Additional information aids such as Recommended literature, information events and self-help groups are useful.
The training of the physiotherapist in the treatment of chronic pain symptoms is therefore a prerequisite for good treatment. For the reasons mentioned, it therefore makes sense that there is no change of therapist if possible.
Since the patients are often afraid of pain and movement, the physiotherapy treatment should be based on an individual finding (see also Physiotherapy / physiotherapy) and careful start of treatment with pain relieving and relaxing measures an increasingly demanding trend in terms of physical activity to have. In this way, the often careless and inactive patient can find out that he is able, despite his pain picture, to perform physical activities with hopefully less pain. A slowly increasing stress demand can be crowned with success to the extent that a moderate strength training is possible.
That is in most cases Increased performance in everyday life and at work and a clear one Increase in quality of life reachable.
If more pain occurs with increasing physical activity (this can certainly happen because the assessment of the patient's resilience - often fluctuating and depending on the daily form -) and therefore the individual dosage is difficult, the load requirements should be reduced and tackled again at a lower level. The patient must be informed beforehand about the possibility of increased pain in the event of excessive training be well informedso that he doesn't lose heart and fall back into his old habits of exercise.
Detailed assessment of the findings
The detailed assessment includes 2 parts:
- Medical history and
- Physical examination
Anamnesis (collection of the medical history)
- How long have the complaints existed?
- Was there an initial event? Trigger?
- How are the complaints expressed? (see symptoms)
- What makes the symptoms worse?
- What alleviates
- How is the everyday stress? What are the biggest problems in everyday life and at work?
- Which drugs? (important for passive and active techniques with regard to the dosage, e.g. with reduced pain perception)
- Are there additional diseases e.g. Overlapping of the pain picture due to a herniated disc?
- Are there any risk factors for active exercise?
- What goals has the patient set for treatment?
Here it is advisable to obtain additional information via a pain questionnaire, which the patient should fill out before treatment.
Physical examination
- Examination of posture and statics
- Checking the active movement functions of the spine and extremity joints (arms and legs), mobility in a pain-free space?
- Examination of the passive movement function of vertebral and limb joints in order to rule out other pain triggers (e.g. joint dysfunction in the spine, herniated disc, shoulder joint problems)
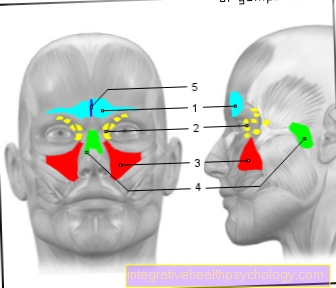
- Examination of the tender points (dolormeter = device for measuring the pain reaction to pressure to estimate the pain intensity)
- Examination of muscle tension, trigger points?
- Checking muscle strength manually or with devices
- Testing of cardiovascular resilience (bicycle ergometer)
- Checking everyday functions such as walking distance, climbing stairs, bending over, lifting