The dental implant
introduction
The implantation of exogenous material, be it as Hip replacement or artificial knee is now almost a routine operation, especially due to the increasing proportion of older people, who naturally show signs of wear and tear on the joints more often.
More and more implants made of metal or ceramic are also used in the oral cavity as tooth root replacements / dentures and fasteners used for prosthetic restoration. Today they are therefore an integral part of dental therapy.

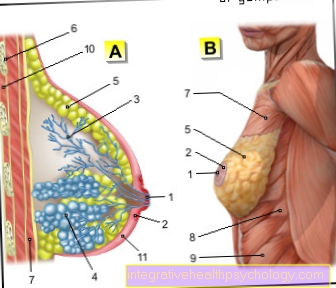
Illustration dental implant

Dental implant
(= artificial tooth root)
- Titanium implant body
here rotationally symmetrical
(Screw implant) - Implant crown
(visible in the mouth) - Implant abutment
with retaining screw - Gums - Gingiva
- Alveolar bone (tooth bearing
Part of the jawbone) -
Pars alveolaris
or alveolar process - Tooth gap
- Tooth pulp in the tooth cavity -
Pulp dentis in the
Cavitas dentis - Tooth crown - Corona dentis
A - missing tooth
B - planting the implant in
Jawbone, supply of
Structure and crown
C - Missing tooth due
Replace single tooth implant
and supplied with a crown
D - orthopanthomogram (OPT)
with three dental implants im
Lower jaw right
You can find an overview of all Dr-Gumpert images at: medical illustrations
Requirements for implantation
If you have decided on a denture with dental implants, you should definitely contact a specialist in implantology in order to benefit from their experience. This will then suggest the individually suitable implant system.
Before starting a prosthetic restoration by means of implants, the treatment is planned, in which the wishes of the patient and the possibilities as well as the advantages and disadvantages of such restoration of a residual dentition or an edentulous jaw are discussed, and what alternatives there are. The financial question also plays a not insignificant role, because to this day the statutory health insurances do not give any subsidies for the implant treatment, but only for the crown, bridge or prosthesis on it.
In order for a dental implant to be placed at all, certain requirements must be met. There must be enough firm bone for the dentist to insert the implant deep enough.
The lower jaw bone is more stable than the upper jaw bone and therefore does not pose a risk for an implant. The X-ray shows whether the bone conditions are correct. are sufficient.
If this is not the case, an implant must be dispensed with, or the bone must be strengthened by implanting the body's own bones. In the upper jaw, the maxillary sinus is a further complication. It can have different dimensions and therefore leave no space for an implant to be placed.
An important consideration is the patient's oral hygiene. The durability of an implant depends largely on the patient's ability and willingness to practice careful oral hygiene. This is not always easy, especially with fixed restorations.
Implants should not be given to patients in whom this is not expected.
Treatment sequence of a dental implant

Once the preparatory measures have been completed, the dental implantation can begin.
The surgical operation is usually carried out under local anesthesia. The procedure is more complex if bone grafting is necessary. If several implants are to be placed and the patient is very anxious, general anesthesia can also be used.
First, the mucous membrane is cut through with a small incision and then the bearing for the implant is prepared with a drill adapted for the dental implant used. This is inserted and the mucous membrane is closed again.
This can lead to pain, which can be eliminated with painkillers. Swelling can be avoided by cooling immediately after the operation. After that, you have to wait for the bone to heal, which can take 3 to 6 months. An interim prosthesis bridges the time. Once the implant has healed, the final restoration can be made: either with a fixed bridge structure or crown or with a removable prosthesis that is anchored to the implants with holding elements.
For the durability of implants, it is very important that the dentures sitting on them are statically sound so that uneven loading is avoided. Otherwise there is a risk of loosening the dental implant. This is why the dentist and the dental technician have to work closely together for such a treatment.
What pain do you have to expect with a dental implant?
You shouldn't endure pain during the operation. There are local anesthetics or stronger narcotisiacs for this. Since the procedure is more invasive than with smaller dental surgeries, postoperative pain can occur when the anesthesia wears off.
The incision made in the mucous membrane and gums alone is painful because the soft tissue has to be severed down to the bone.
Since bones are not dead tissue, the bone can also cause discomfort afterwards. Finally, a screw is drilled into where there may have been nothing but bone for years. The operation itself, the grinding on the bone and the cold water cooling alone can lead to hypersensitivity.
If this persists, you should definitely clarify this with your dentist.
Immediate implantation or conventional tooth implantation?

The so-called immediate implant is only suitable for replacing teeth that are not root-inflamed or acutely periodontally inflamed.
With immediate implants, the implant is inserted immediately after the tooth has been extracted. The crown sitting on it must be designed in such a way that there is no contact with the opposing teeth so that bone healing can take place in peace. The dental implant can only be loaded after about 6 weeks.
When pulling a tooth, it is important to ensure that the bone must not be damaged and that enough bone remains in which the dental implant can be inserted. Teeth with two or three roots are less suitable for this type of dental implant, but not entirely unsuitable.
The advantage of the immediate implant is the shorter treatment time.
The most common is the conventional approach, where the bone has completed healing. The disadvantage, however, is that the patient has to wait several months before the final treatment can begin. But this waiting time can be bridged easily with an interim prosthesis.
Another question is whether the dental implant can be loaded immediately after an implantation. Today there are implant systems that promise immediate loading. The dentist must decide whether the jaw conditions are suitable for this.
Here, too, the fact that the implant has grown in, or osseointegration, over several months is the safest method to ensure an intimate connection between implant and bone.
Medical studies, however, show that there are no significant differences in the durability of immediate implants or conventionally placed dental implants.
Follow-up care for dental implants
Excellent oral hygiene on the part of the patient is essential to maintain the dental implant. The patient must be very careful to keep the implants free of bacterial deposits, as there is a risk that bacteria will otherwise penetrate between the mucous membrane and the dental implant and cause so-called peri-implantitis (inflammatory disease of the teeth supporting appendix, similar to periodontitis). If left untreated, this can ultimately lead to loosening and loss of the implant.
In addition, the patient should come to the dentist for regular check-ups so that complications can be recognized and treated at an early stage.
When can I smoke again with a dental implant?
If you ask a dentist, they would probably say “never”. Nicotine is a cell toxin that can destroy all cells and inhibit wound healing. Since a large wound is made in the mouth during the implantation, the nicotine would destroy the cells that are important for healing, and thus interfere with wound healing.
A simple wound after tooth extraction is said to be at least 2 weeks off from smoking. The wound of an implant is much more invasive. So the cigarette break is correspondingly longer: You should not smoke for 6 weeks.
It could be argued to start smoking again as soon as the wound has healed, but after the wound has healed, bone ingrowth begins, which involves bone cells that must not be destroyed. In addition, the oral flora is so disturbed by cigarette smoke and nicotine that the implant is not adequately protected against inflammation, and there is therefore a risk of loss.
What are the risks with a dental implant?
There are a number of risks associated with implantation that you should be fully aware of prior to surgery and that your dentist should explain to you.
A common problem is the so called Peri-implantitis. This means the inflammation of the tissue around the implant. Due to the inflammation, the implant does not heal into the bone, which can lead to bone loss and loss of the implant.
Smoking, in particular, poses a great risk of inflammation in the newly placed implant.
In order to avoid this, oral hygiene must also be observed and a regular visit to the dentist for control is useful. The earlier peri-implantitis is detected by the dentist, the better the treatment prospects and the implant can be retained.
In principle applies. that a foreign body, such as an implant, is recognized by the cells as not being the body's own and is then rejected by the body. The implant then does not bond with the bone and cannot be retained. Any allergies to a material used should therefore be ruled out beforehand in order to prevent an allergic reaction and thus the loss of the implant.
But rejection of the dental implant is rather rare, since dental implants are usually made of titanium or ceramic. These materials are considered non-allergenic.
In general, there are risks with a dental and especially with such a surgical intervention, since it is necessary to use at least local anesthetics (local anesthesia). In the case of many general illnesses, extreme caution is required when administering local anesthesia and adrenaline.
Despite careful planning, there can always be complications in the operating room, for example
- that the bone splinters or cracks or
- that the nerve canal in the lower jaw is drilled,
- that the maxillary sinus is hit by a maxillary implant,
- that an implant is placed at an angle and the subsequent restoration (i.e. the implant crown) does not fit,
- that it comes to secondary bleeding.
- There are other risks that occur more or less frequently, but less and less because science and dentists have already gained a lot of experience.
Also read the article on the topic: Inflammation on the dental implant
Indications for a dental implant
Dental implants replace the tooth root and replace lost teeth. Once a single tooth has been extracted, an implant can be the basis for a crown. A dental bridge is an alternative, but for this two neighboring teeth would have to be ground and also crowned, a loss of healthy tooth substance that is avoided by the implant. If several teeth are missing, dental implants can also replace the abutment teeth. The alternative would be a removable prosthesis. If the last teeth in the row of teeth are also missing, a dental bridge is only possible with the help of implants.
In the majority of cases, a full denture is an option for an edentulous jaw. But there are patients whose jaws are so unfavorable that a prosthesis does not hold properly. In order to avoid the annoying use of adhesives, implants can provide a secure anchorage. Such a supply is necessary even if the patient only wants a fixed replacement. In these patients, however, it is not enough to only have one implant; at least six implants must be placed depending on the condition of the jaw.
In the lower jaw we often have difficulties in holding a full denture. Especially when the alveolar ridge has already sunk significantly. The reason for the poor hold of the full denture is the tongue movements, the movements of the chewing and sub-tongue muscles. Implants are often the last resort here.
Contraindications to dental implants
There are some situations in which it makes more sense to prefer conventional alternatives to an implant restoration. If the jawbone has broken down too much and augmentation or filling with your own bone is not desired, a supply with implants is not possible. Drugs that disrupt bone metabolism, such as bisphosphonates, or treatment with cytostatics and cortisone, also call the use of implants into question. Even with heavy smokers, you have to check whether implants should be placed. Of course, patients with poor oral hygiene should be excluded from implantation
Lifespan of implants
There are different statements about the lifespan of implants, they range from 10 years to lifelong. The shelf life of Dental implants depends essentially on 3 factors.The osseointegration, i.e. the connection of the implant with the jawbone, the construction of the dental bridge or prosthesis attached to it, which ensure an even distribution of the chewing pressure on the implants, and the careful cleaning of the implants. If these 3 conditions are met, the implant should fulfill its function for a long time.
Dental implant pain
The warranty that the dentist must guarantee on the work carried out is 2 years. Since experience has shown that many dental restorations fortunately last much longer, an implant can, provided it is well cared for, last over 20 years.
Nevertheless, it is subject to natural wear and tear, which is accelerated by too much or incorrect loading. The bone changes over the years and so it can lead to an implant becoming inadequate.
Pain is often related to improper or excessive strain or inflammation. The exact cause and treatment therapy should be clarified quickly with the dentist in order to preserve the implant despite its age.
What to do if the dental implant is inflamed
Regardless of whether a tooth or an implant is painful, you should visit the dentist to clarify the cause. The implant is at least as important as a real tooth root, and requires even better care.
Unfortunately, implants can also cause spontaneous inflammation, despite very good oral hygiene. Once the implant is inflamed, you can treat this inflammation and try to get it under control. Depending on the severity of the inflammation, cleaning may be enough.
If the inflammation is advanced, more thorough inflammation is necessary. This includes rinsing with antibacterial rinsing solutions and cleaning the implant with special instruments that are less hard than the implant itself in order not to damage the dental implant.
In severe cases, depending on how deep the gingival pocket that has formed around the implant is, the gums must be surgically opened and cleaned under direct view. If necessary, depending on whether and which bacteria are responsible for the inflammation, the inflammation can first be treated systemically with medication (e.g. antibiotics).
The treatment is therefore similar to a periodontal treatment. However, the prognosis of an inflamed implant is less good than if it were a natural tooth root with a tooth retaining apparatus, since the immune system of the natural periodontal space is missing.
When is a bridge and when is an implant?
Bridges can only be made if at least 2 abutment teeth are still present. If this is not the case, the missing abutment tooth can be replaced by a Implant be replaced.
Cost of a dental implant
In principle, the costs for dental implants are not reimbursed by the statutory health insurance companies. The cost depends on the number of implants and the implant system used.
In any case, placing an implant is more expensive than making a tooth crown.
In the case of privately insured persons, a request for assumption of costs should always be made in advance so that there are no problems with assuming costs afterwards.
Read more on the topic: Dental implant cost
Can you get dental implants cheaper?
As a rule, implants in Germany cost the same at different dentists. Of course, there are price fluctuations within different manufacturer brands and not every dentist offers the same types of implants, so that there are different prices from practice to practice.
Implants are private services, i.e. they are not covered by the health insurance, unless you have special dental insurance that includes such cases.
In special cases, you can submit a hardship application to the health insurance, and if this is approved, part of the prophetic care (tooth crown or bridge on the implants) will be covered.
There is also the possibility of having implants placed in other countries, for example in Eastern European countries such as Hungary or Poland or even in Turkey. The prices are a lot cheaper there, which the doctors there use to attract many patients. It should be noted, however, that travel expenses are added and the guarantee for a dental implant only applies to the dentist who installed it.
The reasons for lower prices are, for example, lower practice maintenance costs, hourly wages and hygiene standards.
There are many cases in which patients report positively about their dentist in another country, but one must consider which advantages outweigh the advantages. "Made in Germany" stands for quality and, above all, legal security. Monitored by the health care system, only selected and well researched products are used in Germany. So there is always a guarantee on the work that the dentist does in Germany. In the event of any problems (see inflammation below) you always have a contact person who is familiar with the implant used.
Dental implant in the upper jaw vs in the lower jaw
There is no general difference between maxillary and mandibular implants. It always depends on the nature of the bone and the amount of bone available, which type of implant and which size is used.
Dental implants differ not only in length, but also in thickness. If the bone is thin, for example in the region of the lower anterior teeth, thinner implants can be used than in the upper jaw. The thickness of the existing bone, however, again varies from patient to patient.
You don't necessarily have to take the thicker or longer implant, even though there is a lot of bone. Often the smaller one holds just as well. Every dentist has his preferences and experience as to which implant is best for which region.
Of course, it stands to reason that the implant must be thin enough and short enough not to hit adjacent anatomical structures. For example the nerve canal in the lower jaw or the maxillary sinus in the posterior region of the upper jaw.
A notable difference between the bone structure in the upper jaw and the lower jaw is that the lower jaw is much more densely packed than the somewhat more airy upper jaw bone. The stability in the lower jaw is correspondingly much higher.
When do you need bone augmentation for a dental implant?
Basically you need a bone augmentation if the bone is too short or too thin to attach an implant there. The implant needs a certain height and thickness in order not to be levered out again.
However, the abutment is not absolutely necessary if the implant could also be placed in another location.
Nowadays there are also mini-implants that can not only be used for temporary restorations. Because often bone building is not possible or “does not work”. In such cases, the short implants are often used.
The bone structure also depends on the subsequent prosthetic restoration. Often, bone is built up in the maxillary anterior region, although there may be enough bone available just to achieve a better aesthetic result. In this way, a harmonious dental arch can be restored.
For example, if you are planning an implant-supported prosthesis and the patient has a fracture in one place compared to the rest of the alveolar ridge, you should compensate for the loss.
There are no typical places where bone is often built up. Depending on the patient, it depends on where which teeth were before and how long the bone was stressed and how.
In addition to building bones, there is the sinus lift procedure for the upper jaw. The floor of the maxillary sinus, which is located above the maxillary molars, is raised. Then bone substitute material is filled into the cavity created. Thus one achieves a "bone structure" in the figurative sense. There is then more bone substance before the socket for the dental implant is drilled into the bone.
Remove dental implants
If the dental implant is already loose and no longer or hardly connected to the bone, this can easily be removed with the forceps or tweezers. With neglected dental care and inflamed implants with bone loss, there are even patients in whom the implant and restoration (e.g. a bridge) “falls out”.
If the implant is not completely fused with the bone a few weeks after insertion, you could try to unscrew it again. However, this can also lead to bone splintering or fractures.
If the dental implant were completely symptom-free and firmly attached to the bone, there is no need to remove it.
It is problematic if, for example, it was set incorrectly and has already grown together with the bone. It cannot simply be pulled like a tooth, since an implant is not connected to the bone by a fiber apparatus, but is screwed directly into the bone. The bond between the implant and the bone is therefore very solid and strong. In such a case, the oral surgeon or oral surgeon has to mill the implant out of the jaw, including the surrounding bone. This involuntarily leads to bone loss.
history
The insertion of Dental implant was first used in the 1950s. However, it was only 30 years later that implantology was recognized by the dental society as a useful and proven therapy. At first it was the so-called leaf implants. So that this ins Temporomandibular joint large grooves had to be cut in the bone. Today these implants are therefore no longer used. The research dealt primarily with the development of suitable materials. These should of course be tissue-compatible and have a firm connection with the Jawbone achieve. There were implants made of ceramic zirconium dioxide, titanium and titanium coated with ceramic. The shapes and surfaces of the implants were also varied to ensure the most intimate connection possible with the bone. In particular, the surfaces of the implants were repeatedly redesigned to enlarge the area, sometimes by etching, always with the aim of improving the bone apposition. Today the dental implants are made almost exclusively from pure titanium, as this material has proven to be extremely well tolerated. There are now many different implantation systems available to dentists who work in implantology, so that they can select the procedure required for the individual case.
Summary
Implants replace the roots of natural teeth. They are used to attach bridges and prostheses. Dental implants should always be used by an experienced implantologist who has a variety of different implant systems available. Pure titanium is currently the most compatible material. Immediately resilient implant systems and those of a conventional type are offered. Firm anchoring in the bone and careful planning of the superstructure are important. Due to the special anatomical conditions at the interface between the implant and the mucous membrane, careful cleaning is essential to preserve the implant.