Diabetic nephropathy
General

The diabetic nephropathy is one that has been badly adjusted over the years Blood sugar level resulting complication of the "Diabetes“Regardless of the cause of the Metabolic disorder can arise.
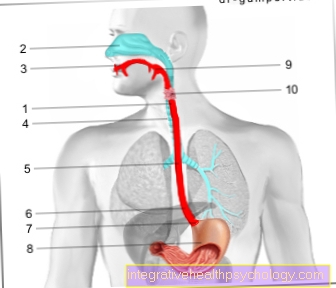
Permanently elevated blood sugar levels can lead to changes in the Vessels of the kidney, as well as structural changes to the filter organs (Glomerula), along with Scarring (Sclerotherapy) and thickening of the structures.
As a result, the filter also becomes permeable to larger and more complex molecules, such as the proteins in the blood (for example albumin), so that proteins, among other things, can be lost.
Read more on the subject at: Albumin in the urine
The disease progresses relentlessly and, without treatment, can lead to a complete loss of kidney function within a few years of the onset of symptoms.
Due to the increasing number of diabetes patients, diabetic nephropathy is now the most common cause of kidney replacement therapy (dialysis) in Germany at 35%.
Diabetes mellitus types
Primarily there is a glucose metabolism disorder, diabetes, which can basically be divided into two types based on their origin.
Of the Type I diabetes usually becomes noticeable in children or adolescents due to a metabolic imbalance that occurs in a short time.
This occurs as a result of the destruction of the insulin-producing cells of the pancreas to an absolute Insulin deficiencyso that the sugar absorbed through food can no longer be absorbed from the blood into the cells, especially the muscles and liver.
As a result, the sugar accumulates in the blood, so that the patient reaches very high blood sugar levels in a short time, which is primarily due to increased need to urinate (Excretion of glucose in the urine), increased Feeling thirsty and Weight loss demonstrate.
To be distinguished is that Type II diabetes, which occurs frequently in connection with poor nutrition and obesity and is caused by a relative insulin deficiency with simultaneous insulin resistance of the cells.
This is true continue to insulin produced by the pancreas, which, however, always over a longer period of time less impact on the cells of the body, so that increasingly higher levels of insulin in the blood are required in order to be able to absorb the same amount of sugar into the cells.
This also leads to increased blood sugar levels, which on various organs (Vessels, kidneys, nerves etc.) can lead to permanent damage.
Nephropathy is a kidney disease that is not caused by inflammation or poison resulting damage was caused.
How does the disease develop
The origin of diabetic nephropathy is still controversial, whereby the so-called "metabolic theory“Is classified as most likely.
This assumes that the permanently high blood sugar levels initially through the accumulation of sugar molecules on body proteins, such as those found in the kidney (Basement membrane of the renal glomeruli, walls of blood vessels) leads to damage to these structures and associated functional changes.
This creates the so-called "Diabetic microangiopathy“ (=Damage to the smallest vessels).
In addition, there is increased blood flow to the kidneys, which, together with this damage, leads to the kidney filter, which normally strictly controls the blood components that are filtered into the urine, loses selectivity, so that larger components also increase how proteins are excreted in the urine.
This leads to a deficiency in these blood components, which can lead to various symptoms.
Symptoms and course

The presence of diabetic nephropathy usually goes unnoticed for years, as the increased blood flow to the kidneys that initially occurs does not cause any symptoms.
Over the years, the structural changes described above occur in the vessels of the kidney and the tissue itself, which after a long time lead to an increased excretion of the main protein of the blood (albumin) leads as the first symptom; there is microalbuminuria with a loss of up to 300 mg albumin per day.
At this stage, the disease is not yet associated with symptoms for the patient; the blood pressure may begin to rise permanently.
If therapy is started immediately at this stage, the progression of the disease can be delayed or prevented.
If this does not happen, there is a steady increase in albumin excretion, which is caused by a transition to macroalbuminuria (Excretion of more than 300 mg per day) is marked.
As progress continues, the kidney becomes increasingly insufficient and more and more blood components (larger proteins too) are lost in the body unintentionally through the urine, which also leads to the accumulation of toxins (especially creatinine and urea) in the blood that would have to be eliminated via the kidneys.
In addition, in advanced stages there is a permanent increase in blood pressure which, in addition to the kidneys, also negatively affects other organs, such as the heart.
The disease has been divided into five stages since 1983, with the increasing, primary urine excretion characteristic of the first stage.
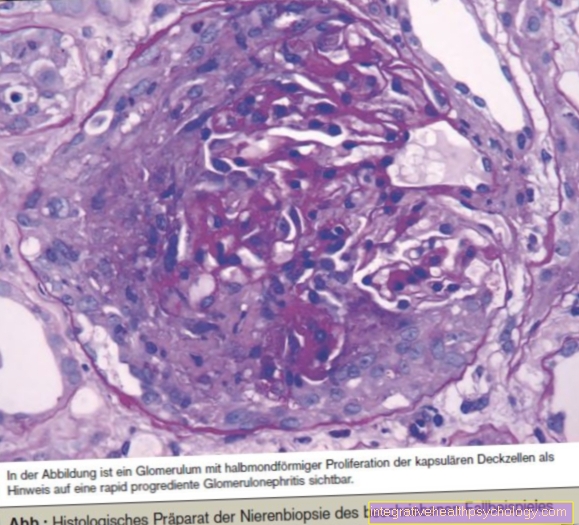
In stage II, kidney function appears to be normal; There is no protein loss yet, but a microscopic examination of a kidney sample (biopsy) typical changes can already be seen.
From stage III onwards, microalbuminuria occurs, which by transitioning to macroalbuminuria exceeds the threshold in the fourth stage.
In stage V, the kidneys are damaged to such an extent that chronic renal replacement therapy, for example using dialysis, is unavoidable.
„Visible"Symptoms usually only appear as soon as more than 3.5 grams of protein are excreted via the kidneys in 24 hours, so that as a result there is a significant protein deficiency in the blood, which leads to water from the vessels passing into the surrounding tissue (Edema formation). In addition to the "Water in the legs“Often about the associated weight gain and foamy urine.
As a complication, the risk of developing blood clots increases (Thrombosis) on; Furthermore, the abnormal excretion of sugar in the urine increases the rate of urinary tract infections.
Early diagnosis
Since the clinical picture of diabetic nephropathy in a large part of thesugar“Occurs in sick people, the patient should be examined annually for the presence of nephropathy.
The screening test includes, among other things, the determination of the amount of albumin in the morning urine; if this is below 20 mg / l, damage to the kidneys in the form of diabetic nephropathy is not to be assumed. If, however, an increased excretion of albumin is found in two out of three urine samples, therapy with so-called ACE inhibitors / AT1 receptor blockers (see below) initiated.
therapy
The main goals of the therapy include, on the one hand, reducing the risk of cardiovascular complications, such as a heart attack or stroke, and, on the other hand, inhibiting the progression of the disease in the form of increasing functional impairment of the kidneys.
The therapy consists of two medicinal pillars:
Check the blood sugar level, if necessary with adaptation of the therapy
Lowering blood pressure
The antihypertensive therapy must be started immediately after the diagnosis of diabetic nephropathy, regardless of the stage; In this case, the goal of a type II diabetic is to lower the blood pressure permanently below 130-139 / 80-85 mmHg. Furthermore, one strives for a maximum protein excretion of 0.5 to 1 gram per day during the therapy.
First choice therapeutics are those already mentioned Angiotensin inhibitors (ACE inhibitors, AT1 receptor blockers), which intervene inhibitory in the blood pressure regulation of the kidney and also demonstrably a protective effect for the kidney against further damage (Inhibition of remodeling processes and scarring) exhibit.
Because the mirror increased Blood lipid levels (LDL cholesterol) Another risk factor for Cardiovascular complications these are also treated in stages one to four, the target value being <100 mg / dl.
The initiation of this therapy is no longer effective in stage V, which is associated with renal replacement therapy, and is therefore normally omitted.
In addition to drug therapy, patients with diabetic nephropathy are also advised to do so Increase hydration, whereby you should make sure that you consume a maximum of 60 to 80 grams of protein per day.
In addition, a Weight normalization (BMI 18.5 to 24.9 kg / m2) recommended.
Risks and prophylaxis
As a preventive measure, the patient can prevent diabetic nephropathy from developing strict blood sugar control and -therapy prevent or at least delay.
Long-term hyperglycaemia (severely increased blood sugar levels) are to be avoided as far as possible, as this increases the risk of developing diabetic nephropathy, among other things due to the accumulation of sugar molecules on structural proteins of the kidney.
In order to be able to measure and control the successful adjustment of the blood sugar over a longer period of time, there is the possibility of the HbA1c value of the patient's blood.
Under Hb (hemoglobin) one understands the oxygen-transporting component of the red blood cells, on which the sugar molecules in the blood prefer to attach.
The HbA1c now shows the percentage of this in the total hemoglobin, which in a healthy patient maximum 6.0 g / dl lies.
If there are increased blood sugar increases, this value increases; Since the red blood cells have an average lifespan of 120 days, the HbA1c provides information about the average blood sugar level over the last three months.
If there were frequent hyperglycaemia, this manifests itself in noticeably increased values.
In addition to poorly controlled blood sugar levels, the risk of developing diabetic nephropathy increases with increased levels Blood lipid levels and presence of a Nicotine addiction.
Furthermore there is a genetic Influence (predisposition), which was shown in studies of affected families.