Phlebitis in the leg
definition
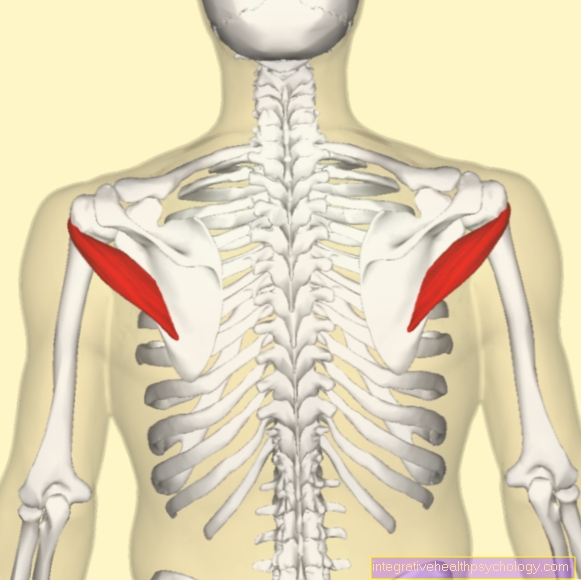
Phlebitis of the leg is inflammation that is confined to a specific section of the vein. The wall of the venous blood vessel is usually the point of attack for the human immune system, which causes the inflammation. A distinction is made between inflammation of the superficial leg veins and inflammation of the deeper veins.
The inflammation can be clearly pronounced as an acute event, such as in thrombophlebitis, an inflammation of the superficial veins, or subliminally, as is the case, for example, with chronic venous insufficiency.
Read more on the subject at: Phlebitis in the thigh

The reasons
The causes for an inflammation of the venous vessels of the legs are different and diversified and therefore have to be treated by different specialist disciplines.
The most common cause is probably phlebitis caused by thrombosis. Usually a combination of little fluid, long periods of sitting, increased age and a familial disposition lead to the development of a thrombosis. This then closes the vein, prevents blood flow and calls the immune system on the plan that causes inflammation in the blocked area.
In the context of chronic venous insufficiency, liquid and small proteins escape from the blood into the surrounding tissue around the smallest venous blood vessels. Here, too, the immune system recognizes an error and starts a slight inflammation, around in the "leaking" smallest blood vessels. However, this inflammation is nowhere near as present and painful, but rather runs in secret.
A third major cause are various autoimmune diseases that target your own blood vessels, so-called vasculitides. This primarily affects components of the blood vessel walls that are recognized as foreign by the immune system. Depending on the disease, not only veins but also arteries are affected
Find out all about the topic here: The thrombosis in the leg.
The diagnosis
The diagnosis of an inflammation of the veins, a so-called phlebitis, is made by the doctor from a combination of anamnesis (recording of the illness history), physical examination as well as imaging and a blood count.
The history and physical examination show a fairly clear picture of a thrombosis of the leg veins - which is the most common cause - which is validated with the help of the ultrasound and various laboratory parameters from the blood test.
The other causes mentioned mostly give less specific anamnesis, so that a larger blood count often provides certainty if there is a justified suspicion of an autoimmune disease. Chronic venous insufficiency, on the other hand, usually presents with leg edema and superficial varicose veins and can also be validated using an ultrasound device.
Find out more about the topic here: The phlebitis.
I recognize phlebitis by these symptoms
Here too, the so-called TBVT - deep vein thrombosis - is the most common and usually the clearest example. On the one hand, the affected leg hurts - regardless of movement, on the other hand it looks red and feels warmer than the unaffected leg when compared to the side. In addition, there is a - partly discrete, partly significant - increase in circumference compared to the healthy side on the affected leg.
These symptoms can, but do not necessarily, occur with every leg vein infection.
The symptoms of phlebitis - You can find more here.
The pain in the leg
Pain in the leg is usually the leading symptom when it comes to diagnosing phlebitis. Every inflammation, no matter whether caused by pathogens or "sterile caused", is characterized by 5 symptoms, one of which is pain.
The pain is only caused by the immune system. Its cells release so-called inflammation mediators, which on the one hand serve to attract other cells of the immune system, but on the other hand also have the effect of making the sensitive nerves more susceptible to pain and creating an acidic environment in the area of inflammation. Thus, the pain goes back when the immune system regulates its work down again.
The treatment
Therapy varies greatly between the different causes of phlebitis. At this point, the corresponding therapies for deep vein thrombosis, autoimmune diseases and chronic venous insufficiency are mentioned as examples.
In order to treat the inflammation resulting from a thrombosis, the primary need to eliminate the thrombosis. As a rule, the body takes on this task itself and therapeutic support takes the form of blood thinning, which is intended to prevent the existing thrombus from enlarging. In special cases, thrombolysis (dissolution of the thrombus) may also be indicated in the case of a venous thrombosis in order to prevent complications of the thrombosis.
Autoimmune diseases, on the other hand, are treated very differently. Glucocorticoids such as cortisone are often the first choice for therapy. Cortisone dampens the effect of the immune system so that it is no longer directed against the body's own cells. Further therapeutic approaches include filtering out incorrectly polarized antibodies or modified antibody therapies. In some cases, “donor antibodies” are also administered, which slow down the immune system, but still guarantee adequate protection.
Chronic venous insufficiency, on the other hand, has its main problem not in the inflammation, but in the consequences of the inflammation, which causes poor blood circulation in the legs, which ultimately leads to open legs. To prevent this, preventive care should be provided. The "leaky" superficial veins can be removed, which strengthens the deeper ones. Compression stockings should also be worn and daily walking activities such as running, hiking, and walking should be undertaken.
Read more about the topic here: Treatment of phlebitis.
What is the best way to put my leg up?
Elevating the leg helps counteract the swelling and makes it easier for the blood to get back to the heart through the inflamed venous vessel. The leg does not have to be positioned very high, 30 degrees in the hip joint are easily sufficient, since the blood vessels or nerves that run in the groin can become trapped if the position is too steep.
Furthermore, it should be ensured that the heel is well padded and the Achilles tendon does not come to rest on an edge. Especially in older patients or diabetics, pressure sores can develop here, the treatment of which would have been an avoidable evil.
The home remedies
All available home remedies can only be used externally in the case of phlebitis, which is why not too great an effect is to be expected. Quark compresses are a popular remedy for inflammation, which could also be used here. The quark has a cooling and thus refreshing effect on the overheated, inflamed leg. Chamomile is also said to have an anti-inflammatory effect, but external use will hardly be of any use.
The most effective is actually the elevation of the inflamed leg, possibly in combination with cooling measures, which, however, serve the well-being rather than have a therapeutically relevant effect.
Also read the article: The quark wrap.
The ointments
No real therapeutic benefit can be expected from any ointment that attempts to treat external venous inflammation. The skin is simply too impermeable for an ointment to penetrate into the depths of the inflamed blood vessel.
As mentioned above, cooling can make the pain and overheating of the inflamed leg a little more pleasant, so an ointment with a cooling effect could be of slight benefit. Otherwise, the money for an ointment is better invested elsewhere.
The duration
As with the therapy, the prognosis of phlebitis is fully dependent on the causative disease. To come back to the three examples (leg vein thrombosis, autoimmune disease, chronic venous insufficiency), the following results:
The venous thrombosis can be treated well; depending on the degree of severity, even to the family doctor. The blood thinning is continued for 6 to 12 weeks and can then be discontinued if everything is ok again. However, if repeated thrombosis occurs, a blood thinner will have to be taken for life.
Chronic venous insufficiency and autoimmune diseases, on the other hand, are chronic diseases that can never be completely treated, but are subject to good control. While conservative measures such as compression stockings and exercise have the greatest effect in chronic venous insufficiency, the autoimmune disease must be treated with medication in order to ensure a normal life as possible.
Find out more about the here Duration of a phlebitis
The course of the disease
The course of the disease is of course highly dependent on the underlying disease.While chronic venous insufficiency and autoimmune diseases have chronic disease courses, i.e. cannot be completely treated, thrombophlebitis is an acute disease that can be treated without residue. Chronic venous insufficiency is associated with the greatest restrictions in everyday life, as its therapy mainly consists of wearing compression stockings, regardless of the weather.
Read more about the topic here: The phlebitis.
The complications
Thrombophlebitis as the most common cause always carries the risk of pulmonary artery embolism. This would cause part of the thrombosis to dissolve and migrate via the heart into the blood vessels of the lungs, where it then becomes "blocked" again. This complication is associated with increased mortality, but usually does not occur at all or only so subliminally that one does not notice it. Another complication after a venous thrombosis is the so-called post-thrombotic syndrome. Here ... ..
Complications of chronic venous insufficiency are, on the one hand, open legs, and, on the other hand, infections that lodge in the wounds and can cause blood poisoning, especially in older people.
The open leg
The open leg is the dreaded complication of chronic venous insufficiency and describes the disappearance of the upper layer of skin in potentially different parts of the lower leg. However, the middle side of the lower legs are predisposed.
Due to the venous insufficiency, there is a remodeling process in the body tissue around the blood vessels. As a result, it is very difficult for the blood to deliver oxygen to the surrounding tissue and the cells that rely on the oxygen supply from the blood perish - just like the top layer of skin. The resulting wound, in turn, also lacks the oxygen required to heal, so that a permanently opened wound appears on the leg, which is the ideal breeding ground for bacterial / viral infections.
When can you do sports again?
Especially after thrombophlebitis, exercise is an important prevention factor in order to prevent or prevent the recurrence of a thrombosis. However, if a thrombosis has occurred, an ultrasound examination should first be carried out to rule out that parts of the thrombosis can loosen and migrate via the blood into the lungs, where in the worst case they would trigger a pulmonary embolism.
Exercise is also an important protective factor in chronic venous insufficiency. However, if there are open areas on the legs, these should be adequately covered. With autoimmune diseases, the general condition is the decisive point. If you feel physically capable of doing this, nothing stands in the way of the sport.