Fallopian tube inflammation
introduction
A fallopian tube inflammation is called in medical terminology Salpingitis refers to and is one of the inflammations of the upper genital tract. In the majority of cases, both fallopian tubes are affected by the inflammation. Inflammation of the fallopian tubes usually occurs in conjunction with inflammation of the ovary. The combination of inflammation of the fallopian tubes and ovaries is also known as adnexitis.
Inflammation of the fallopian tubes is a common gynecological condition that can affect women of all ages. However, there is an increased risk in young, sexually active women or women with an intrauterine device (coil). In most cases, fallopian tube inflammation is caused by a bacterial infection ascending from the vagina or uterus.

Causes of the fallopian tube inflammation
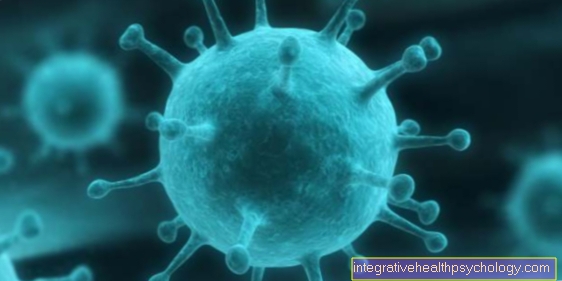
A Fallopian tube inflammation or one Adnexitis is often through a ascending infection from the vagina or uterus. The cause of such ascending inflammation is one Decrease in natural protective barriers. The protective barrier can e.g. the Menstrual period, through foreign objects such as a spiral, one birth or vaginal operative interventions have been affected. Due to the disrupted protective barrier, bacterial or viral pathogens can now enter the body more easily and cause an infection.
In the case of fallopian tube inflammation, the bacterial pathogen in the foreground, are rarer Viruses responsible for adnexitis. The bacteria that are most likely to trigger inflammation are Gonococciwhich one gonorrhea Trigger (gonorrhea), Chlamydia and Mycoplasma. In percentage terms, these three types of bacteria are responsible for most of the inflammation.
In addition to a disturbed barrier function, there is also an increased risk of pathogens entering unprotected intercoursewhich can lead to the infectious transmission of bacteria or viruses.
There are also other strains of bacteria that can cause fallopian tube inflammation. These include e.g. Escherichia coli and other microorganisms, the so-called anaerobes, which are characterized by their ability to live in an oxygen-free environment.
Girls or women who have not yet had sexual intercourse must also go through one tuberculosis-Bacteria (Mycobacterium tuberculosis) induced inflammation.
Inflammation of the fallopian tubes can originate directly from the genital organs (primary inflammation), or from other organs located in the abdominal cavity (secondary inflammation). For example, a Intestinal inflammation spread and cause inflammation of the fallopian tubes and ovaries. However, this type of adnexitis is extremely rare and occurs in less than one percent of cases.
therapy
An inflammation of the fallopian tubes, with or without inflammation of the ovaries, should be treated immediately, otherwise complications can arise.
Antibiotics are usually given intravenously to treat the inflamed fallopian tubes. The treatment is usually inpatient, which means that those affected remain in hospital for the treatment period. The treatment period is about 10 days.
A broad spectrum antibiotic is often given at the beginning of the therapy, as the pathogen has not yet been detected by the laboratory. The laboratory results require some time, so that treatment is started immediately due to the possible complications of fallopian tube inflammation.
As soon as the pathogen is detected by the smear, antibiotic therapy specific to the pathogen is initiated. If no pathogen can be clearly identified or if the antibiotic therapy is unsuccessful, a broad spectrum antibiotic is administered.
If the symptoms improve, the antibiotic administration can be changed - instead of the intravenous administration of the drug, a change to tablets can be made.
In addition to antibiotic therapy, anti-inflammatory therapy with anti-inflammatory drugs (e.g. diclofenac) should also be initiated. This therapy also relieves the acute pain associated with fallopian tube and ovarian inflammation. In addition, cooling the lower abdomen also provides pain relief in the early stages. In the further course, moist, warm wraps and fango packs, which stimulate the blood circulation, help. After the treatment in the hospital has been completed, mud packs and mud baths support the healing process.
The therapy remains the same for chronic fallopian tube inflammation if there are still signs of inflammation. The problem is that at this stage the fallopian tubes often remain glued and if you still want to have children, a laparoscopy (laparoscopy) have to be reopened. Adhesions can also be loosened during a laparoscopy.
In rare cases, the only treatment option is to remove the fallopian tubes via an abdominal incision (Salpingectomy).
These home remedies can help
It should be emphasized that the fallopian tube inflammation is a very serious clinical picture, which can have serious consequences in chronic or recurring courses. These include, for example, infertility and the spread of the inflammation to surrounding organs. Therefore, home remedies should only be used as a support, for example to relieve symptoms or pain, and never alone. In terms of therapy, a gynecologist should always be present so that, after a thorough examination, a pathogen-specific antibiotic drug can be prescribed and long-term effects can be prevented. Home remedies that can be used as support can be, for example, cold applications in the abdomen. These have a pain-relieving effect in acute inflammation and slightly lower the fever when the temperature is high. In the already subsiding symptom interval, hot water bottles can again have a relaxing effect. In addition, various tea blends with anti-inflammatory ingredients can be drunk. These include chamomile or yarrow.
Duration
The duration of inflammatory processes in the area of the fallopian tube varies widely. This depends on the severity of the inflammation, any involvement of neighboring organs and the underlying spectrum of pathogens. Inflammation of the fallopian tube can subside spontaneously and last only a few days, but it is not uncommon for the inflammation to cause little or no discomfort, which is why, in the absence of therapeutic measures, the inflammation can last for weeks to months. The timely start of a pathogen-specific antibiotic therapy significantly influences the duration of a fallopian tube inflammation. The intake of antibiotics takes an average of three weeks, but can take longer if the therapy is unsuccessful.
Complications
Untreated or inadequately treated fallopian tube inflammation can develop into chronic fallopian tube inflammation develop. As part of the chronification, the inflamed tissue is converted into scars and connective tissue. This results in a permanent or a temporary one Closure of the fallopian tubes, being additionally still Fluid in the fallopian tubes collects (Hydrosalpinx), which leads to further damage to the tissue. In connection with inflammatory changes in the fallopian tubes, adhesions (see: Fallopian tubes glued) spoken. The danger of a sterility (Infertility) increases and becomes more likely without treatment. The risk one Ectopic pregnancy is also significantly increased.
Furthermore, inflammatory processes of the ovaries that are not treated can lead to a Inflammation throughout the pelvis come, which can have serious consequences.
These life-threatening complications include e.g. a Peritonitis as well as a Intestinal obstruction.
Possible symptoms of chronic inflammation are alternating dull pains in the lower abdomen or also Discomfort during intercourse.
What can the consequences be?
Inflammation of the fallopian tubes, especially if the infection lasts for a long time and there is no therapy, can have numerous consequences. Due to the female anatomy and the close proximity of other organs, the inflammation can spread to surrounding structures, for example inflammation of the ovaries and inflammation of the uterus, especially with its frequently affected uterine lining. The full picture of a pronounced inflammation of several genital organs is called Pelvic Inflammatory Disease designated. Perihepatitis (Fitz-Hugh-Curtis syndrome), i.e. an adhesion of the liver capsule and the peritoneum, can also occur. In connection with this, right-sided upper abdominal complaints are often described. It can also lead to the formation of encapsulated pus collections. The pathogens can also spread through the bloodstream and affect other organs that are further away. In such cases, one speaks of sepsis, which is to be classified as potentially life-threatening. Another, relatively common and much feared complication is an unfulfilled desire to have children due to infertility. This is often the result of inflammatory adhesions in the fallopian tube, which is therefore neither penetrable for sperm nor for the cracked egg cell. With milder adhesions and the fallopian tube still partially accessible, the risk of ectopic pregnancies, so-called extrauterine pregnancies, is increased.
How does a chronic fallopian tube inflammation come about?
A chronic, long-lasting inflammation of the fallopian tubes can occur in several ways. On the one hand, in many cases the inflammation caused has few symptoms or has no symptoms at all. This makes an early medical consultation and drug treatment impossible, which can lead to chronification. In addition, even with symptomatic fallopian tube inflammation, the complaints are often so unspecific that many women dismiss them as harmless and refrain from gynecological advice, which in turn results in a protracted course and thus enables the transition to a chronic stage of inflammation. Incorrect antibiotic therapy with a dose that is too low or insufficient coverage of all pathogens involved in the case of a mixed infection can also result in chronification.
Is fallopian tube infection contagious?
The possible pathogens of fallopian tube inflammation include, for example, bacteria of the gastrointestinal tract, some others address the spectrum of pathogens that cause sexually transmitted diseases. These include in particular gonococci, the pathogen causing gonorrhea (also: gonorrhea), and chlamydia. The latter two are mainly transmitted through sexual intercourse. Sexual abstinence must therefore be observed in the case of a diagnosed fallopian tube inflammation in order to avoid re-infection for the duration of the antibiotic therapy. In addition, the partner should also present himself to a doctor in order to have a microbiological smear made and, if the result is positive, also start drug therapy. To prevent infection, the use of condoms is strongly recommended. In addition, the recommended gynecological check-ups should be taken in order to diagnose a possible infection at an early stage.
For more information, see: Sexually transmitted diseases
Symptoms
The symptoms of fallopian tube inflammation or inflammation of the fallopian tubes and ovaries can be very different. An infection can proceed without any severe discomfort or be associated with severe pain. Of the Degree of severity of symptoms is here variablewhich sometimes results in fallopian tube inflammation not being immediately recognized as such.
Quite often, however, occur in those affected as part of an infection severe, sudden onset of bilateral pelvic pain on which by a general feeling of illness (Exhaustion, tiredness, weakness). The abdominal wall is often under tension and is extremely sensitive to touch and pressure in the lower abdomen.
A temperature rise, respectively fever, can accompany the pelvic pain and the general feeling of illness.
Also Spotting and an increased and malodorous one discharge (fluorine) can emerge from the vagina. Furthermore, it can also lead to discomfort during sexual intercourse, a so-called dyspareunia, irregular stool behavior such as diarrhea (Diarrhea) or constipation (Constipation), Flatulence (Meteorism) and Painful urination (Dysuria) come.
Regardless of whether the fallopian tube inflammation causes only mild or severe discomfort, is one Treatment indispensable. If an acute fallopian tube inflammation is not adequately treated, it can develop into a chronic fallopian tube inflammation develop. The chronic stage is characterized by dull Pelvic discomfortwhich can occur on one or both sides and usually increase in intensity when you sit down. Adhesions can in some of the affected patients for Discomfort during intercourse to care.
These can be signs
There are different courses of fallopian tube inflammation. The acute, subacute and chronic stages are divided. The acute, i.e. sudden, symptoms include unilateral abdominal complaints, which can point to the affected fallopian tube. Depending on how severe the inflammation is and whether neighboring organs are affected, the entire abdomen can also hurt and become hard, which is then referred to as the acute abdomen. Other symptoms can include fever, fatigue, and feeling very sick. In the subacute stage, the symptoms are milder and more unspecific. A slight feeling of pressure on the affected side can occur in the lower abdomen, possibly also pain during a palpable examination. Fever is less likely to occur. Chronic fallopian tube inflammation can be almost completely symptom-free or, similar to a subacute course, be associated with unspecific symptoms. These include back pain, gas, and constipation. You may also experience pain during sexual intercourse. Each stage can flow into another. Other possible signs of fallopian tube inflammation may include heavier or prolonged bleeding during your period. It can also lead to increased vaginal discharge, which can also change in consistency, color and smell.
diagnosis

The first indications of an inflammation of the fallopian tubes emerged from the questioning of the patient. Those affected complain of existing pelvic pain and a general feeling of illness. In some cases, those affected also describe other symptoms, such as painful urination, vaginal discharge and diarrhea.
This is followed by a physical examination of the patient. In the majority of patients, bilateral tenderness in the lower abdomen can be identified, which is a first indication of an existing inflammation. There may also be a defensive tension when examining the lower abdomen.
As part of the gynecological check (Speculum examination), the cervix and vaginal area can be examined and smears can be taken to detect the pathogen.
In the advanced stage of inflammation, the fallopian tubes and possibly also ovaries can be enlarged and palpable in a tightly elastic manner.
In addition, an ultrasound examination is extremely helpful in making a diagnosis. If the inflammation persists over a long period of time, this can result in an accumulation of fluid in the lumen of the fallopian tubes, a thickening of the fallopian tubes and free fluid in the free abdominal cavity.
With the help of a blood sample, inflammation values in the blood can be found that would suggest an existing fallopian tube inflammation or inflammation of the appendix organs. Typical inflammatory parameters include an increase in white blood cells (Leukocytes), an increase in C-reactive protein, also known as CRP, and an accelerated sedimentation rate, often known as ESR.
If none of these examination methods result in a clear picture, an MRI of the abdomen can be made, which can reveal evidence of an inflammation in the lower abdomen.
In addition, an abdominal or pelvic examination (laparoscopy or Pelviscopy) provide important information or serve as evidence of an inflammation of the fallopian tubes. As part of a mirroring, a direct smear is taken from the fallopian tubes and then examined for pathogens.
Summary
At a Fallopian tube inflammation Both fallopian tubes are often affected. It is also often associated with inflammation of the ovary. The combination of fallopian tube and ovarian inflammation can be described with the term Adnexitis sum up.
Inflammation of the fallopian tubes can cause severe discomfort and requires inpatient treatment with antibiotics and pain relievers. If left untreated, fallopian tube inflammation can become chronic, leading to changes in the tissue, which can ultimately lead to adhesions and occlusion of the fallopian tubes. The risk one sterility Developing (infertility) increases sharply without initiating therapy.



.jpg)