Egg freezing
introduction
The possibility of freezing human egg cells, regardless of whether they are fertilized or unfertilized, gives women who do not yet want motherhood at a young age, more flexibility in terms of family planning. While the process of freezing has been used experimentally for decades, it was only through the recent development of a “shock freezing method”, the so-called flash freezing, the rate of egg cells that survive the defrosting and defrosting procedure has risen to such an extent that the Cryopreservation is at least technically possible. However, since the freezing of egg cells is also associated with risks and costs, but above all because it represents an essential interference in the process of human reproduction, the ethical and social aspects of this topic are controversially discussed.
history
The process of freezing a human egg cell was originally developed as a variation of artificial insemination in order to be able to conceive at a later point in time for young women who were expected to lose fertility as part of the treatment of cancer with radiation or chemotherapy . The first successful insertion of a previously cryopreserved egg took place in 1986. Since the newly developed method of freezing was developed a few years ago, the survival rate of a frozen egg has generally been over 80%. A few years ago the American Society for Reproductive Medicine declared (American Society for Reproductive Medicine) that she no longer sees the process of freezing a human egg cell as an experimental process.
Read more on this topic at: Egg donation
When does egg freezing make sense at all?
Certain diseases, especially cancer, can threaten fertility due to the subsequent therapy. This includes not only some drugs that damage germ cells, radiation in the area of the pelvis and thus the reproductive organs or certain operations can have a negative impact on fertility.
Furthermore, if there is a genetic predisposition to premature ovarian function loss, freezing (Cryopreservation) of egg cells can also be useful. All indications have in common that the freezing of egg cells is a preventive, i.e. prophylactic, procedure. Functioning of the ovary at the time of egg retrieval and freezing is therefore a prerequisite and should always take place before any damage to the ovarian function is likely.
Before chemotherapy
Whether freezing egg cells before starting chemotherapy is sensible and necessary at all depends largely on two main factors: the age of the patient at the start of therapy and the chemotherapeutic agent used. The dosage and the duration of intake also play a role here. In general, it can be said that, for example, the chances of young patients without cryopreservation of their eggs are often better than those of older patients, where the freezing of eggs is more often necessary to realize the desire to have children.
In the case of chemotherapy with frequent administration cycles and in high doses, the freezing of egg cells is usually recommended due to the strong effect on cell division. Ultimately, however, the decision as to whether cryopreservation makes medical sense with the selected form of therapy depends on the individual case and should be discussed with the treating team of doctors.
Read more on the subject at: Chemotherapy side effects
How Many Eggs Should You Freeze?
There is no one-size-fits-all recommendation on how many eggs should be frozen. However, it has been shown that a certain number of frozen egg cells do not survive cryopreservation and perish. Therefore, one should not assume that the number of frozen eggs equals the number of attempts at potential pregnancy. The probability of a later successful pregnancy increases with the number of cryopreserved egg cells. Therefore, between 10 and 20 eggs are often frozen. Such a large number of egg cells can often only be obtained in several hormonal stimulation cycles with subsequent suction of the mature egg cells
Can you freeze already fertilized egg cells?
There are two types of egg cryopreservation. The egg cells can be frozen in both the unfertilized and fertilized form. Both procedures have in common that first of all a drug-based, hormonal overstimulation of the ovaries takes place. This causes the simultaneous, simultaneous maturation of several egg cells. These mature egg cells are then punctured from the ovary in a small operation.
Suitable egg cells can then either be frozen directly or fertilized with the sperm of the partner or a donor using the In-Vitro-Fertilization (IVF) or Intracytoplasmic Sperm Injection (ICSI) method. In the so-called pronuclear stage, i.e. in the state in which maternal and paternal DNA have not yet merged, fertilized egg cells are frozen. This is done after adding an antifreeze, which is supposed to prevent cell damage from ice crystals, using liquid nitrogen at a temperature of -196 degrees Celsius.
If pregnancy is to begin, the fertilized egg cells must be thawed during a so-called thawing cycle (Cryocycle) first thaw. Not all cells are still able to develop after freezing. Those who are able to do so are transferred to the uterus to implant there.
Read more on the subject at: Artificial fertilization
Biological-technical background
In order to be able to successfully store a human egg cell for years or decades and then use it to bring about a pregnancy, three hurdles must be overcome.
First, one or more mature, healthy egg cells must be removed from the woman. As a guide, the number required is around 10 to 20. There are three main problems: a healthy woman usually only matures one egg cell per month, with the quality of this egg cell rapidly decreasing as the woman ages. An operation under general anesthesia is necessary for the removal. In order to protect the woman from many procedures, before the procedure she undergoes hormonal treatment to increase the number of eggs jumping per cycle. As in fertility or fertility treatment, the ovary is stimulated. Usually this hormone treatment is done with the drug Clomiphene in tablet form or the hormones FSH / LH by syringe. This drastically reduces the number of removal operations required, so that 2 to 3 removal procedures are now usually sufficient to obtain over 10 “good” egg cells for freezing.
However, the problem remains that the quality of a woman's egg cells continues to decline beyond the age of 25. In a 30-year-old, less than 50% of the egg cells are capable of fertilization, in a 40-year-old less than 20%. The corresponding monthly chances of a naturally occurring pregnancy are approx. 20% for a 30 year old woman and approx. 5% for a 40 year old. However, a 25-year-old who would be at the optimal age for a collection usually does not see the need for egg screening, nor does she have the necessary financial resources on hand. If the desired partner has still not been found beyond 35 years of age, or if the professional career is currently more in the focus of acute interest, the ticking of the biological clock makes the possibility of cryopreservation look much more seductive. The result is that the average woman who wishes to freeze egg cells, due to naturally already reduced fertility, then has to undergo several cycles of hormone treatments and removal procedures to achieve the required number of healthy egg cells.
The second hurdle is of a technical nature. In order to enable a biological material to last for years without natural aging or decomposition by microorganisms causing an undesirable end to its shelf life, freezing is the method of choice. The problem: If ice crystals form in the process, they pierce the cell boundaries of the frozen biomaterial because they are sharp-edged. As a result, the cells are irreparably destroyed; when thawing, only mud is presented. To prevent the formation of crystals, anti-freeze agents - so-called Cryoprotectants - added and freezing takes place either very slowly (as was usual in the past) or very quickly (new method). As part of the so-called Vitrification the cell material is cooled to approx. -200 ° C in little more than a second, preferably with the help of liquid nitrogen. The disadvantage is that the use of antifreeze agents, some of which are toxic, cannot be prevented.
The third hurdle after successful removal, selection, freezing, thawing and artificial insemination is the task of getting this egg cell into the uterus (uterus) of the woman. Since it is often not successful implantation, especially in older women, especially because of reduced blood flow, it is legally permitted in Germany to introduce up to three fertilized egg cells at the same time. However, this also increasingly leads to multiple pregnancies. In order to increase the chances of implantation, additional previous hormone therapy may be necessary. As a result, a more pronounced mucous membrane of the uterus can provide a more favorable starting position.
Medical risks
For the child that has emerged from a frozen egg including artificial insemination, there are no known risks for hereditary diseases or other diseases that exceed the average; Thousands of children have already been conceived this way. However, due to the expectant mother's age, which is usually advanced, there is by definition a high-risk pregnancy with in some cases considerably higher probabilities of numerous pregnancy complications. The risk of miscarriage is significantly increased.
In addition to the increased risks of a late pregnancy, the woman herself is also directly exposed to an above-average risk to her health through the procedural interventions and hormone treatments. The most common undesirable effects that can occur during hormone therapy that stimulates the ovaries are nausea and vomiting. A so-called ovarian hyperstimulation syndrome (OHSS) it is less common. In the case of this more serious complication, in the mild, more usual form, nausea and vomiting, but sometimes also abdominal pain, are to be expected. About 1% of patients develop a worse form of ovarian hyperstimulation syndrome, which is associated with cysts on the ovaries, ascites (Azsites), Shortness of breath (Dyspnea), as well as coagulation disorders can be associated. Especially younger women and those with ovaries rich in blisters (polycystic ovaries) have an increased risk of developing ovarian hyperstimulation syndrome from hormone therapy.
Read more on the subject at: Polycystic Ovarian Syndrome
Ultimately, when deciding on egg screening, the risks that arise from the surgical egg retrieval itself should also be taken into account. This procedure, which is usually carried out under general anesthesia, is not a complicated matter for the surgeon, but even if the risks for bleeding, infections, etc. are very low in addition to those of an anesthetic complication, they can never be completely ruled out. A conscientious weighing of opportunities, costs and risks should therefore always precede a decision for such a procedure.
Read more on the subject at: Risks of general anesthesia
costs
Usually, the costs for hormone treatments, removal interventions, egg storage and insertion of the egg cells, which are incurred as part of egg cell screening, are not covered by the health insurance company. Should follow-up costs arise as a result of these medically unnecessary treatments, these must also be borne privately.
The costs involved are by no means insignificant; just keeping the egg cells in a so-called cryobank costs hundreds of euros per year. Overall, depending on the provider, the number of necessary removal interventions, etc., costs in the high four-digit or even five-digit range are to be expected.
Social implications
At the biologically optimal age for pregnancy - between around 20 and 25 years of age - the average woman in a western industrial nation is generally more likely to be in training or at the beginning of her career than in a married or illegitimate partnership. Therefore, intentional motherhood only occurs in individual cases. The emancipated woman is expected to follow the man in terms of education and professional advancement. Also, due to the lack of large family associations and sufficient social and state backing in childcare in Germany, a problem-free coexistence of family and work of both parents is de facto not given. Many couples only decide “at the last minute” for a family that is often quite poor in numbers.
The possibility of freezing an egg cell undoubtedly gives the individual woman more room to maneuver in family planning, to the effect that the founding or expansion of the family can then be postponed beyond the natural fertility phase. The problem is that the existence of this option (especially when the employer bears the costs, for example) also enables the society to expect women to actually take advantage of this option, for example in order to devote themselves to a job in their “best” years , and not starting a family. It is highly questionable whether a work-life balance is more likely at the age of 40 or even 50. From a medical point of view, however, it is strictly not advisable to postpone starting a family beyond work, i.e. into retirement age. In general, younger parents are also better equipped than “sprightly” seniors to cope with the hurdles of bringing up children.
To what extent the existence of the possibility of a human egg cell for the purpose of a displaced, artificial reproduction To be able to freeze is desirable from an ethical point of view, and to what extent the exercise of this option is socially meaningful remains to be seen.
In summary, it can only be said that the cryopreservation process has left the experimental stage in medical and technical terms and is routinely possible, but not free of risk. In biological terms, however, a natural pregnancy at 20 to 25 years of age (except in exceptional cases such as cancer) is always superior to late motherhood with the help of reproductive medicine and is therefore preferable.
Illustration of an egg cell
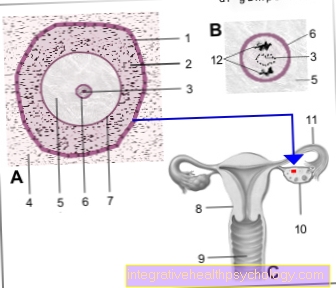
- Basin -
Membrana basalis folliculi - Granular layer
(seed-rich layer
of follicle cells) -
Epithelium stratificatum
cuboideum - Granules -
Nucleolus - Basic tissue of the ovary -
Stroma ovarii - Egg cell - Ovocytus
- Cell nucleus - Nucleus
- Glass skin - Zona pellucida
- Uterus - uterus
- Sheath - vagina
- Ovary - Ovary
- Fallopian tubes - Tuba uterina
- Polar bodies
You can find an overview of all Dr-Gumpert images at: medical illustrations