Iron deficiency anemia
Note
You are in a sub-topic of the anemia section.
General information on the topic can be found at: Anemia
introduction
Iron deficiency anemia is the most common form of anemia, accounting for over 50% of cases. Women are most frequently affected (around 80%).
It occurs when the body needs more iron to produce blood than it can absorb and the iron stores are exhausted.

Symptoms of iron deficiency anemia
The clinical appearance of iron deficiency anemia has three components:
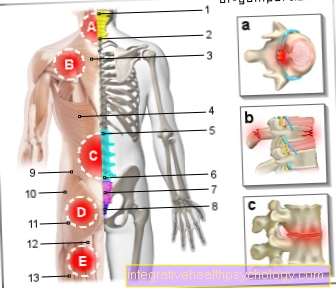
- Signs of anemia such as paleness, poor performance, accelerated heartbeat (tachycardia), shortness of breath
- Signs due to iron deficiency:
Dryness and brittleness of the skin, hair and nails, inflammation in the mouth area (rhagades at the corner of the mouth, burning tongue) - Signs of blood loss such as Tarry stools (black stools), blood in the urine (Hematuria), Coughing up blood (hemoptysis), or if menstruation is too heavy or too frequent, etc.
Read more about this: How to recognize iron deficiency anemia such as Consequences of iron deficiency
Therapy for iron deficiency anemia
The aim of iron deficiency therapy is to sustainably replenish the iron stores in the body. If the iron deficiency is already visible in the blood count in the form of anemia (anemia), the iron stores have already been used up and the iron deficiency has progressed further. Basically, in the case of iron deficiency, the supply of iron must be increased. On the one hand, this can occur through increased consumption of iron-containing foods. Iron from animal products can be absorbed 3 times better by the body, vegetable iron, on the other hand, has a lower value and is more difficult to absorb through the intestine.
This article might also interest you: Foods with iron
In general, however, only 10-15% of the iron ingested through food is absorbed in the intestine. If iron deficiency anemia is already pronounced, therapy by changing diet alone is very tedious and not very promising. Here you should use food supplements in the form of juices (herbal blood), tablets or capsules. In order to increase the absorption in the intestine, the preparations should be taken with foods containing vitamin C, such as orange juice. But even here the therapy has to be carried out for several months.
The fastest and most effective form is the administration of iron infusions. By bypassing the gastrointestinal tract, the iron is 100% available to the body. However, intravenous iron therapy must be carried out and monitored by a doctor, as allergic reactions can occur. At the same time as iron administration, the cause of the deficiency must always be found and a possible underlying disease such as bleeding or inflammatory bowel disease treated.
Read more on the subject at: This is how you fix an iron deficiency such as Diet for iron deficiency
What are the consequences of iron deficiency anemia?
If there is anemia due to iron deficiency, the red blood pigment hemoglobin is low. Hemoglobin is responsible for the transport of oxygen in the body, it is loaded with oxygen molecules in the lungs and releases them again in the organs. Oxygen is required there to generate energy. The heart muscles have the highest oxygen demand, followed by the skeletal muscles, the brain and the kidneys. These organs are the first to react and very sensitively to a drop in oxygen levels in the blood. The first consequences of iron deficiency anemia are therefore a drop in performance, both in physical and mental work. Those affected often feel weak and tired despite getting enough sleep.
Lack of oxygen in the brain also leads to headaches and dizziness. The body reacts to the drop in oxygen levels by increasing the heart and breathing rates. In this way, the remaining hemoglobin should be transported faster through the body and recharged more quickly with oxygen in the lungs.However, increased work of the heart and breath consumes more energy and oxygen - a vicious circle.
These articles might also interest you:
- Consequences of iron deficiency
- The consequences of anemia
Iron deficiency anemia and hair loss
A typical symptom of iron deficiency anemia is hair loss. Iron is an important component of various enzymes that are involved in metabolic processes, growth and regeneration. The hair root cell is one of the fastest dividing cells in the human body and therefore requires a lot of iron and energy. In iron deficiency anemia, the body lacks iron and oxygen and thus the energy required for rapid cell division. If a hair root cell is not adequately supplied, it dies and the hair falls out. In general, the hair becomes increasingly thin and brittle.
This article might also interest you: Hair loss
Can iron deficiency anemia also be fatal?
With untreated iron deficiency anemia, the hemoglobin value (Hb value) continues to drop. If this happens slowly, the body can adapt to a certain point. Hb values between 6-8 g / dl can be compensated well in some cases. If Hb values are below 6 g / dl or if complications such as a sharply increased heart rate (tachycardia), a sharp drop in blood pressure (hypotension), falling blood pH or ECG changes occur, the body must be given foreign blood in the form of a blood transfusion as the situation can decompensate (derail) in a life-threatening manner.
Read more on the topic: Blood transfusion
Causes of Iron Deficiency Anemia
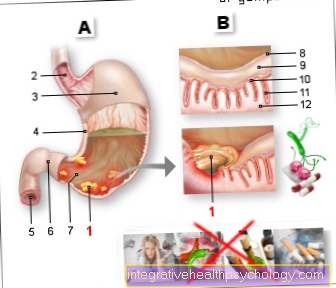
An iron deficiency arises on the one hand in gastrointestinal disorders such as after removal of the stomach (gastrectomy), resorption disorders in the intestine (malassimilation) or due to chronic intestinal diseases.
Bleeding is also the most common cause. The source of these losses can be:
- too heavy and too frequent menstruation
- Bleeding from tumors, ulcers
or - hemorrhoids
There is also an increased need for iron during pregnancy or growth. Diet also plays an important role in iron deficiency anemia.
Vegetarians can be particularly affected. The divalent iron in meat can be absorbed particularly well by the body. If a person eats a vegetarian diet, it must be ensured that sufficient substitute sources are available.
Typical risk factors for iron deficiency anemia
-
Female gender (menstrual bleeding)
-
Pregnancy / lactation
-
Chronic diseases (heart failure, kidney failure)
-
Cancers
-
Chronic inflammation
-
(Chronic) blood loss (stomach ulcer, intestinal ulcer, hemorrhoids)
-
Competitive athlete
-
After gastrointestinal resection
Iron deficiency anemia from a heavy period
Women of childbearing potential are at a particularly high risk of developing iron deficiency anemia. On a normal day, the healthy body loses around 1 mg of iron. This amount can be balanced with a balanced diet.
In women with heavy menstrual bleeding, the loss of blood and thus iron can increase immensely. Typically, a woman loses 30-60ml blood (60-120mg iron) per month, but with heavy bleeding it can lose up to 800ml blood (1600mg iron). Since only 10-15% of the iron ingested through food is absorbed in the intestine, iron deficiency situations can quickly arise.
Laboratory parameters in iron deficiency anemia
In iron deficiency anemia, laboratory parameters such as decreased serum iron and ferritin, increased transferrin with decreased saturation and decreased reticulocyte hemoglobin are shown.
The soluble transferrin receptor sTfR is increased. In terms of differential diagnosis (alternative causes), it is also important whether there is inflammation at the same time. The parameters transferrin and ferritin show changed concentrations in inflammatory reactions.
They are also referred to as acute phase proteins (ferritin, the value is increased in the event of inflammation) or as anti-acute phase proteins (transferrin, the value is decreased in the event of inflammation). Therefore, the inflammation parameters CRP and leukocytes are also determined.
Morphologically, the red blood cells appear hypochromic-mircocytic, i.e. Hemoglobin content (MCH) and cell volume (MCV) are reduced. The erythrocytes may appear as anulocytes or target cells in the blood smear. This means that the cells are pale in a ring due to the lower hemoglobin content.
In addition to the analysis of the blood, a clinical examination (examination of the affected person by a doctor) is mandatory.
Also read: Test for iron deficiency and ferritin
How is the MCV changing?
MCV meant mean corpuscular volume i.e. it shows the average volume of red blood cells (erythrocytes). The value can be calculated from the hematocrit (proportion of solid components in the blood) and the number of erythrocytes.
In iron deficiency anemia, fewer and, above all, smaller red blood cells are formed because the important component iron is less available. The MCV is thus lower - one speaks of microcytic anemia. The normal value is 85-98 fl. Changes in the MCV alone are not meaningful; other blood values such as hemoglobin, hematocrit, MCH (mean amount of hemoglobin per erythrocyte) and MCHC (mean hemoglobin concentration per erythrocyte) must always be taken into account.
Read more on the subject at: Erythrocyte parameters
Laboratory values of transferrin
Transferrin is a protein that transports iron. It is made in the liver, depending on the iron content in the body. The total transferrin in the body can bind 12 mg iron, but usually only 30% is loaded with iron.
An iron deficiency leads to a decrease in the transferrin level, and the value is also decreased during pregnancy. Elevated values are found in chronic inflammation, tumor diseases or iron overload.
Laboratory values of ferritin
The term ferritin is understood to be a protein that stores iron. As the storage form of iron, it acts as an indicator of the iron supply in the blood plasma.
Serum ferritin is a basic building block for diagnostic methods of iron metabolism. Its reference range is normally 30-300 µg / l for men and 10-200 µg / l for women.
In iron deficiency anemia, the ferritin level is lowered and is crucial for the differential diagnosis. So you can e.g. Iron deficiency anemia cannot be ruled out if the ferritin level is increased, because a chronic inflammation may be present at the same time, which would increase the ferritin parameter.
Reticulocyte count in iron deficiency anemia
Reticulocytes are newly formed, young, immature red blood cells (erythrocytes). During blood formation, the red blood cells go through various stages of maturity - the reticulocytes are the last stage before the mature, functional erythrocytes. Usually 1% reticulocytes are present in the blood.
In the case of anemia, which is caused by blood loss, the reticulocyte count increases in order to compensate for the loss of red blood cells as quickly as possible. If there is an iron deficiency, however, reticulocytes can only be formed more slowly because an important component is missing. In iron deficiency anemia, the reticulocyte count is therefore reduced.
Find out more about this topic at: The reticulocyte count.
Iron Deficiency Anemia in Pregnancy
The pregnant woman supplies the unborn child with blood via the umbilical cord and thus with nutrients and oxygen. For this, more blood and, above all, red blood cells must be produced in the woman's body. For this, twice as much iron (30mg / day) is needed as in non-pregnant women (15mg / day). Blood volume increases by up to 40% during pregnancy.
In addition, the work of the heart increases to pump larger amounts of blood forward per beat, which requires more energy and oxygen. If the hemoglobin value of the pregnant woman is below 11 mg / dl, anemia is beginning. In addition to the typical symptoms of anemia, iron and oxygen deficiency have negative effects on the growth of the placenta and the child. The rate of premature births and miscarriages is increasing. In addition, the development of a pregnancy-related illness (gestosis) is favored.
Iron is also required for the formation of thyroid hormones, which in turn are very important for the child's brain development. Existing anemia can also make it harder to compensate for increased blood loss during childbirth and promote puerperium infections. Therefore, Hb and ferritin control at the beginning of pregnancy is of great importance. An Hb value above 11g / dl is harmless. Iron deficiency anemia should be considered below 11g / dl and the attending gynecologist should be advised about iron administration.
Read more on the topic: Iron Deficiency During Pregnancy
Classification of iron deficiency anemia
The classification of the Anemia takes place after:
- the volume of red blood cells: macrocytic, normocytic, microcytic
- the hemoglobin content (protein, which one oxygen transported and iron contains): hypochromic, normochromic, hyperchromic
- the cause: blood loss, synthesis disturbance, increased breakdown (hemolysis)
- the bone marrow findings