Purulent meningitis
Synonyms in a broader sense
bacterial meningitis, hood meningitis, convexity meningitis, leptomeningitis, meningococcal meningitis
Medical: Purulent meningitis
English: meningitis, brain fever
General information
General information on "What is meningitis?" can be found under our topic:
- meningitis
definition
The term purulent meningitis (purulent meningitis) describes a purulent inflammation (-itis) of the meninges and spinal cord membranes (Meninges), which can be triggered by different pathogens.
The purulent meningitis (purulent meningitis) is mostly caused by bacteria. She goes with high fever and severe general symptoms such as clouding of consciousness and represents an absolute emergency that must be treated immediately.

Symptoms
The symptoms of purulent meningitis is usually similar for all pathogens. It often begins with a period of flu-like symptoms such as:
- Exhaustion
- Temperature increase / fever
- Body aches
This phase is known medically as the prodromal stage. The prodromal stage is followed by the generalization stage. At this stage, the pathogen floods the body, leading to a very acute, severe clinical picture with:
- high fever
- strongest a headache (Stage of inflammation of the meninges)
- Neck stiffness (meningism)
Symptoms in Infants and Children
In infants and young children it is more difficult meningitis as such to recognize. The symptoms are not as pronounced as in adults. The children may be apathetic or scream shrilly and refuse to eat.
Symptoms of intracranial pressure are vomiting and a bulging one Fontanel (Bone gap in the infant's skull).
The Meningitis in children should be treated in a children's clinic if possible.
The patients cannot put their head on the chest or only with severe pain because this movement inflamed the chest Meningessurrounding the spinal cord / neck cord become stretched and irritated (posopportunityitive stretch mark). The patients show an increased sensitivity to all sensory stimuli; Touching the skin, bright light or loud noises are perceived as painful. Often exist dizziness and chills.
It is not uncommon for concomitant encephalitic symptoms to develop. This means that not only the meninges, but also the brain is irritated, what with Impaired consciousness and mental symptoms can go hand in hand. Meningitis often spreads to the brain as it is washed with the "excitatory" nerve water (Meningoencephalitis).
The consciousness is then often clouded and can range from mild drowsiness to delirious states to coma. Patients can be confused and misunderstand their surroundings, which means that older patients are at risk of developing the disease as stroke or acute confusion is misinterpreted.
Other symptoms can include pronounced restlessness or seizures (epilepsy) be.
In 10% of patients it happens Cranial nerve involvement, 10-20% have hearing impairments due to involvement of the Labyrinth of the inner ear.
Because of the inflammation in the brain, that can happen too Intracranial pressure builds up (increased intracranial pressure), because inflammatory processes tend to result in swelling / water retention (Edema) go hand in hand so that the body's own defenses can work better (as can be done e.g. by Insect bites knows).
In most inflammatory processes, this swelling can escape outwards. However, since the skull is limited to the outside and there is not so much space inside, the brain literally compresses itself when it swells (Brain edema).
Signs of increased intracranial pressure Vomit and rapid deterioration of consciousness.Centers in the brain that are important for survival are then squeezed together and stimulated. Sometimes the intracranial pressure builds up so quickly that it can no longer be controlled, and life-threatening conditions can occur despite immediate treatment.
Especially with meningitis Meningococci (meningococcal encephalitis) it can happen that small punctiform skin bleeding occurs that cannot be pushed away (petechiales exanthem).
When they do occur, urgency is paramount as they are signs of a Blood poisoning (sepsis) by the bacteria or their components that Endotoxins = bacterial toxins, represent.
75% of patients with a Meningococcal meningitis show these or other skin changes.
The Meningococcal sepsis (approx. 50% of the cases of meningococcal meningitis) is more dangerous than meningitis itself, because the endotoxin toxins of the bacteria activate the coagulation system in the blood and use up the coagulation factors dissolved in the blood (Consumption coagulopathy, disseminated intravascular coagulation).
As a result, it not only bleeds into the skin, but also into other organs, especially the Adrenal gland (Waterhouse-Friedrichsen Syndrome), shock symptoms can arise (Endotoxin shock).
Despite timely treatment, the lethality (mortality rate) in this sudden course is still 85%.
Causes / origin
The emergence of the purulent meningitis can be traced back to three causes.
- Purulent meningitis via the bloodstream (mostly after droplet infection, e.g. via cough or runny nose)
- referred meningitis
- direct (secondary) meningitis
Purulent meningitis
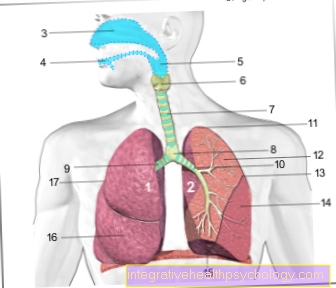
The most common is the spread of the pathogen with the bloodstream (hematogenous meningitis). On the one hand, this can be the case if a bacterial infection (e.g. of the nasopharynx (runny nose) or the lungs (to cough)) generalized, i.e. the pathogens spread throughout the body with the blood.
On the other hand, pathogens from a chronic pus focus can repeatedly be washed into the blood, for example in a chronic one Endocarditis (Inflammation of myocardium / valvitis = pathogens spread from the heart) or one Osteomyelitis (chronic bone suppuration = pathogens spread from the bone).
Most common pathogens: Meningococci, Pneumococci, Streptococci, Staphylococci, Enterococci
Forward meningitis
The relayed meningitis usually arises from an infection on the head, e.g. an (acute or chronic) sinus infection, otitis media or Mastoiditis (The mastoid process is called the temporal bone behind the external auditory canal.
It is an air-filled bone that is connected to the Middle ear connected). The pathogens migrate here through the thin bone walls of the skull into the so-called Subarachnoid space and thus lead to infection.
Of the Subarachnoid space lies with the three meninges between the bony skull and the brain and is bathed in nerve water, the so-called. Cerebrospinal fluid. Bacteria that enter this space through the bone first pass through the outer, hard meninges (Dura mater). Below is the middle, delicate spider web skin (Arachnoid), under which the said space is located (sub = under, sub-arachnoid = under the spider's tissue), which is filled with nerve water and from which the pathogens can easily spread over the entire surface of the brain (and the spinal cord). The lower limit of this subarachnoid space forms the inner, soft meninges (Pia mater)that lies directly on the brain as a delicate layer and follows it into its furrows and coils.
Most common pathogens: Pneumococci, meningococci.
Direct (secondary) meningitis
Even with skull injuries like with Skull base fracture bacteria that colonize the nasopharynx and sinuses can easily enter the Subarachnoid space immigrate, especially if the outer, hard meninges have been injured. Finally, in the case of open skull injuries, the pathogens have direct access to the Liquor spaces, so that in many cases inflammation occurs within a short time.
Most common pathogens: Pneumococci, Haemophilus influenzae, staphylococci.
diagnosis

In addition to the clinically impressive and trend-setting clinical picture, the primary examination if bacterial meningitis is suspected is the removal and examination of the nerve fluid (liquor). It should be obtained before antibiotic therapy is initiated and examined for pathogens, cells, protein, sugar and lactate. These factors provide an indication of the type of inflammation.
The normal, healthy liquor is clear as water.
It is filtered off by the blood at certain points in the brain and then spreads over the brain and spinal cord within the meninges. To remove it, use a hollow needle to go into one of the spaces between the 3rd and 5th lumbar vertebrae in the spinal cord space below the spinal cord (lumbar puncture). The nerve water then drips through this needle into sterile tubes.
Read more on the subject below Lumbar puncture.
Its appearance alone can give clues to the type of disease and possible pathogens: In the case of purulent meningitis, it is cloudy to purulent, in viral meningitis it is clear to at most a little cloudy. In addition to the liquor (nerve water), blood is always examined and both findings are compared with one another.
This examination is called liquor diagnostics (examination of the nerve water). A lumbar puncture is not done if the patient becomes comatose quickly or if there are other signs of increased intracranial pressure or signs of abnormal clotting.
Read more on the topic: CSF diagnostics in purulent meningitis
To secure the diagnosis, see Grief staining of the pathogen Detected under the microscope (color visualization of the pathogen), bacteriologically detection is carried out by creating a culture. Pathogen detection is possible in 70-90% of cases.
The Blood culture (Blood smear on culture media) is positive in 30-50% of cases. One can still be found in the blood Leukocytosis (Accumulation of white blood cells) and an increase in CRP (C.-ractive Pred, CRP value), which is a non-specific marker for the course of inflammatory processes in the body.
That too Procalcitonin is in the serum, as opposed to one viral meningoencephalitis, elevated.
A PCR (Polymerase cgrove reaction) for the detection of bacterial DNA or the detection of bacterial antibodies only takes place if the CSF findings are unclear or the pathogen is not detected.
In addition, there is usually also a CT (= Computed tomography) of the head (CCT = C.raniumC.computerTomography) made to the Sinuses (Maxillary sinuses, Frontal sinuses, ethmoid cells) as well as possible melting points of the mastoid (mastoid process) from which meningitis can be propagated.
Likewise, other foci of pus can be like a Brain abscess, Bleeding or Infarcts (problems with the blood supply to the brain) be recognized.
Also the extent of the existing Intracranial pressure by Brain edema or Hydrocephalus (Head of water) can thus be estimated.
Complications
Complications:
- Cerebral edema (swelling of the brain) with increased intracranial pressure
- Waterhouse-Friedrichsen Syndrome (10-15% of Meningococcal sepsis cases)
- Hydrocephalus (= Water headi.e. the Nerve water cannot run off and builds up) due to inflammation-related adhesions of the meninges
- Collections of pus in the cavities of the brain that are normally used for cerebrospinal fluid (Cerebral ventricle; Ventricular empyema)
therapy
Therapy of purulent meningitis is based mainly on:
- Treatment with Antibiotics
- surgical removal of inflammatory foci, if any
- Brain pressure therapy
- Therapy of complications
If the pathogen has not yet been identified, an intravenous antibiotic treatment consisting of several antibiotics is started as soon as possible, depending on the suspected pathogen.
Information on this can be obtained from the previous history:
- In previously healthy adults, but also in immunocompromised and alcoholics, a broad spectrum antibiotic is initially combined, which crosses the blood-brain barrier well (Cephalosporins 3rd generation, e.g. Cefotaxime or ceftriaxone, 3x / day 2 g), with ampicillin (3x / day 5 g).
- In patients who have likely acquired the germ in hospital (nosocomial infection), after surgery or trauma, one combines Vancomycin (2 g / day every 6-12 hours) with Meropenem or Ceftazidime (each 3x / day 2 g).
- In adolescent patients with skin symptoms, meningococci are relatively likely to be present. Here you treat with high doses penicillin G. A pathogen must still be detected.
If there is evidence of germs, the antibiotic treatment is changed specifically for the pathogen. So there are several recommended ones Therapeutic shamata, which depend on the pathogen and its resistance behavior (ineffectiveness of certain antibiotics due to the development of resistance).
The sensitivity of the pathogen to different antibiotics is in a so-called Antibiogram tested.
Penicillins intervene in the cell wall structure of the bacteria and thus prevent them from growing. They are particularly good at contributing gram positive bacteria how Pneumococci and gram negative cocci like meningococci, which are treated with high doses of penicillin G for 10 to 14 days. In principle, penicillin allergy Cephalosporins are used.
If purulent meningitis has developed through a corresponding focus of inflammation, this focus (paranasal sinuses, mastoid, middle ear; Brain abscess; visible on CT) must be surgically removed immediately.
The treatment of cerebral edema poses a particular difficulty. Conventional therapy is performed by elevating the upper body to about 30 °, giving sufficient pain reliever medication and normalizing the body temperature.
In rare cases, the patient is put under anesthesia (Thiopental anesthesia).
Still exist Intracranial pressure sign (Vomiting, clouding of consciousness), attempts are made with intravenous administration of hyperosmolar solutionslike glycerol, mannitol or dextrose solutions to draw the water "from the brain tissue into the blood vessels" (Osmotherapy). The water molecules flow from the place of low concentration to the place of higher concentration, i.e. from the tissue into the blood.
The gift of Steroids like that Cortisone, which have anti-inflammatory effects has long been controversial, but has ultimately proven to be ineffective for treating cerebral edema. Only for Dexamethasone (Fortecortin) a certain beneficial effect has been demonstrated.
It is recommended that 10 mg of dexamethasone be administered immediately prior to administration of the antibiotic and that this should be continued every 6 hours for 4 days.
More recent studies show that this has reduced mortality and the frequency of unfavorable courses as well as hearing disorders, which is more likely to be attributed to a general positive influence on the disease process than to a reduction in intracranial pressure (Deutsche Gesellschaft für neurology).
Does the intracranial pressure persist or is there Hydrocephalus before, one must consider Ventricular drainage to put on. This is done using a hose (Shunt) placed directly in the cerebrospinal fluid spaces of the brain so that the nerve water can flow outwards and the intracranial pressure is reduced.
In the case of an infection with meningococci and severe meningococcal sepsis (blood poisoning by meningococci and meningococcal toxins), the so-called. Waterhouse-Friedrichsen Syndrome occur in which an activation of the body's own coagulation system with the consumption of coagulation factors dissolved in the blood is in the foreground, which leads to numerous smaller and larger bleeding into the skin and other organs.
These coagulation factors must be replaced under constant laboratory control. That's why you give in addition Blood plasma (Fresh Frozen Plasma = FFP), because it contains coagulation factors.
From puberty onwards, blood clot formation is also inhibited (thrombosis) with anticoagulants (Heparins) as Thrombosis prophylaxis recommended.
forecast
Since the development of penicillins, the mortality rate from bacterial meningitis (meningitis) has been reduced from 80% to 20% (5 - 30%). Nevertheless, it has not changed significantly since then: antibiotic therapy has improved, but as the age of the patients has increased, the overall mortality rate has not decreased.
Unfavorable factors for the prognosis of bacterial meningitis are:
- Rapid development of the clinical picture
- Disturbances in consciousness within the first 24 hours
- Duration of a coma
- Little or no pus formation, although bacteria are the cause (apurulent course): this indicates a weakened immune system
- Older age
- Complications such as hydrocephalus (congestion of the cerebral fluid), pus-filled brain ventricles (ventricular empyema) or vasculitis (inflammatory changes in the blood vessels)
After the acute symptoms have subsided, general impairments such as poor concentration, irritability or dizziness may persist for a few weeks or months.
For permanent damage (Defect healing) is in some cases with
- Hearing impairment through to deafness due to damage to the sensitive auditory nerve (acoustic nerve) can be expected. Facial paralysis caused by damage to the facial nerve (facial nerve palsy) or other cranial nerves can also occur.
- Adhesion and scarring of the meninges can lead to impaired drainage of the nerve water and thus to an increase in pressure inside the skull (hydrocephalus).
- Pathogens remaining inside the skull can form an encapsulated abscess.
- Epilepsy can also occur more frequently.
In general, severe permanent damage can be traced back to too low a dosage or too short a duration of antibiotic therapy.
In meningococcal meningitis with sepsis (blood poisoning) there is more than 50% the risk of the defect healing with a reduced intelligence / dementia.
rehabilitation
Rehabilitation can be carried out as an inpatient in a rehabilitation clinic or as an outpatient in a neurological therapy center.
Early support for recognizable defect healing or late damage is useful and depends on the remaining deficits, in particular:
- Speech therapy
- Hearing aids such as cochlear implants or hearing aids
- Concentration training
- Memory training in groups or computer-aided
- Occupational therapy to restore fine motor skills
- Physiotherapy (physiotherapy) for balance disorders, dizziness and to promote mobility.
Prophylaxis / mandatory notification
A patient with Meningococcal infection should be isolated after initiating antibiotic therapy, as meningococci are easily transmitted by droplet infection and direct contact. After 24 hours there should be no more infection.
During this time, hospital staff and visitors must observe certain hygiene measures, such as wearing protective gowns, nose and mouth protection as well as gloves and hand disinfection.
Close contact persons of the sick person becomes one Antibiotic prophylaxis recommended.
The family doctor can prescribe this.
Mostly it will be as early as possible either Rifampicin (600 mg twice a day for 2 days) or one tablet Ciprofloxacin (500 mg) given. Alternatively, you can get a single dose Ceftriaxone Inject into the muscle (adults 250 mg, children half).
Since the incubation period for meningococci is 2 - 10 days, antibiotic prophylaxis after 10 days is no longer useful. Such measures are not necessary for other meningitis pathogens.
Furthermore, in the case of justified suspicion, in the event of illness or death in the case of meningococcal infection (meningitis and / or Blood poisoning due to meningococci) according to the Infection Protection Act in Germany, a report to the responsible health authority should be made within 24 hours.
If a suspicion has not been confirmed, this must also be reported immediately.
vaccination
There are vaccines (active immunization) against Meningococci, pneumococci and Haemophilus influenzae. However, not everyone has to be vaccinated against meningococci and pneumococci. Please refer: Vaccination against meningitis.
The vaccination against Haemophilus influenzae type B (HIB) was recommended for all children by the Standing Vaccination Commission (STIKO) in 1990 because this bacterium (which has nothing in common with the influenza virus that causes the flu) causes dangerous purulent meningitis in infancy, which if not detected and treated in time leads to severe consequential damage (untreated mortality is 60 - 90%!).
In addition, some strains are now resistant to common antibiotics.
Is vaccinated with one Dead vaccine (i.e. with capsule components of the bacterium that are coupled to a protein and thus generate an immune response in the body.
This means that no infection can occur during the vaccination!) From the completed second month of life, usually as a combination vaccination with other vaccinations that are usual at this age (tetanus, diphtheria, whooping cough, poliomyelitis and Hepatitis B.).
There are three vaccinations every four weeks, the fourth in the 2nd year of life (with a single vaccine only three vaccinations, the third in the 2nd year of life).
Children who are not vaccinated against HIB and are older than 18 months will only receive one vaccination.
In addition to meningitis, it also protects against sometimes life-threatening inflammation of the airways and the epiglottis (Epiglottitis) by the same pathogen.
HIB infections are rare after the age of 5, so older children and healthy adults are not vaccinated. Exceptions are made for people who have been born or have had an operation without a spleen, which is important for the immune system, and for other disorders of the defense against infection (vaccinations for adults).
Against Meningococci (Neisseria meningitidis) there is a quadruple vaccine that includes serotypes A, C, W-135 and Y, and a dual vaccine against serotypes A and C.
Serotype (or serogroup) means that different strains of a bacterium have different surface properties (antigens) against which our body also forms different antibodies.
In Germany, meningococcal serotype B is predominant with almost 70%, against which no vaccine has yet been developed. The frequency of serotype C has risen to around 30% in recent years, which can be protected against by vaccination.
The Meningococcal vaccination is recommended for the following risk groups:
- People who plan a longer stay in areas where meningococcal infections frequently occur (so-called endemic areas), e.g. Development workers in the "Meningitis belt"From Africa (serotype A), aid workers, backpackers to India,
- Adolescents or young adults planning a longer stay in countries where vaccination against serotype C is recommended for this age group (e.g. semesters abroad in England, Ireland, Spain, Greece),
- People with immune system disorders, a dysfunctional or absent spleen,
- Pilgrims to Mecca. Saudi Arabia requires vaccination with the quadruple vaccine no more than three years and at least ten days ago,
- Laboratory personnel at risk.












.jpg)