Inflammation of the jaw
introduction
The human teeth are firmly anchored in our jawbones in a tooth socket provided for this purpose, the alveolus.
The upper jaw, the maxilla, and the lower jaw, the mandible, together form a functional unit. Untreated mouth sores can spread to the jawbone and cause severe pain that requires prompt treatment.

Type of inflammation
Periostitis, osteomyelitis, ostitis ... many confusing terms that all refer to inflammation in the jawbone, but, viewed more differently, mean different inflamed areas. Ostitis is an inflammation of the small canals, the Havers and Volkmann canals, that occurs together with periostitis or osteomyelitis.
Periostitis describes an inflammation of the skin of the bone (periosteum).
Osteomyelitis is acute or chronic inflammation of the bone marrow, usually caused by an infection, which can spread further and thus bring about ostitis and / or periostitis. It occurs more often in the lower jaw than in the upper jaw.
The different types of inflammation often occur together, as inflammation of one component quickly spreads to the other.
Periosteum inflammation
Periosteum inflammation is an inflammation of the connective tissue skin that envelops the bones and is rich in blood vessels and nerves. The Latin term for it is periosteum and derived from it, the medical name for the form of inflammation, periostitis.
It usually arises from bacteria or also mechanically and can either be acute or chronic. It is possible that small pieces of bone detach from the outer area during the inflammation process, but the reverse phenomenon, new bone formation, can also be stimulated by an inflammation.
Inflammation of the jaw muscle
Inflammation of the jaw muscles can occur due to overuse of the masticatory muscles.
But also through classic forms of development, such as mechanical stimuli (injuries, pressure, foreign bodies), physical factors (UV light, ionizing radiation, heat, cold), chemical substances (acids, alkalis, bacterial toxins) or pathogens.
Inflammation in the temporomandibular joint
Temporomandibular joint inflammation is caused by incorrect and overloading of the structures involved in the temporomandibular joint and the chewing process. Inflammation in the temporomandibular joint is more related to the protected structures in a capsule and is then referred to as so-called capsulitis. But the masticatory muscles in interaction with the surrounding tissues can also be involved. One speaks of the so-called craniomandibular dysfunction.
With various hand movements and guided movements of the lower jaw, the dentist can act specifically to make a diagnosis. Physiotherapy and splint therapy are then followed by a targeted initial therapy.
Maxillary sinus infection
An inflammation of the maxillary sinus is shown clinically on the one hand by percussion sensitivity (sensitivity to knocking) of the superficial skin structures on both sides of the nose and the areas under the eye sockets. On the other hand, headaches and an increased feeling of pressure can be a sign of this. The paired maxillary sinus, which is always air-filled in a healthy state, is also called the maxillary sinus.
The diagnosis of maxillary sinus infection can be confirmed by an ultrasound examination or radiologically with the help of an orthopantomogram (overview of the upper and lower jaw and the lower part of the frontal sinus). In stubborn cases, it is possible to determine the germs from the secretion flowing through the throat. Pathogens are usually bacteria that, especially in smokers, find their entry into the nasopharynx through the damaged nasal mucosa and therefore usually only allow the disease to heal completely with antibiotics.
Read more on the topic: Maxillary sinus infection
causes
The causes of jaw bone inflammation are wide-ranging.
It can be caused by a fracture that is associated with an opening to the oral cavity. But also one of the teeth that e.g. if left untreated for a long time in a very advanced carious state, outgoing infection or an accumulation of pus can lead to it. This is also the most common cause, as poor oral hygiene and the bacteria that have accumulated with it attack the hard tooth structure. The bacteria come a little closer to the bone. If left untreated, they work their way to the tooth pulp, where pus forms. From there, the bacteria can spread into the bone tissue and form an abscess in the jaw.
Furthermore, such a disease can occur when removing a tooth that is in a highly inflammatory stage. This could be possible with a wisdom tooth removal. Pus can build up in the maxillary sinus and cause jaw inflammation. If bone tissue dies for various reasons, the risk of inflammation is just as present as with a cyst. A jaw cyst in particular can cause severe discomfort.
Various external factors can promote the development of such an inflammation. These include smoking and the use of drugs, diabetes mellitus, poor immune defenses and inadequate nutrition. Radiation of the bone due to cancer therapy can also promote the development. Such a type of inflammation is also possible in infants and children.
You might also be interested in this topic: Root canal treatment
Inflammation of the jaw from a cold
Most common colds are caused by viruses. Jaw infections, on the other hand, are caused by colonization by bacteria. These mostly get into the bones through fractures, caries, periodontitis or other inflammatory changes in the surrounding tissue. If you have a cold, the maxillary sinuses may become inflamed (sinusitis).
However, in these cases the inflammation of the mucous membranes of the maxillary sinuses does not spread to the bone. In conclusion, this means that a viral cold is, in most cases, not a cause of jaw inflammation.
Read more about this: Sinusitis
Inflammation of the jaw after a dental procedure
Infections of the jaw can relate to the bone or the periosteum surrounding it. They can occur after an operation and e.g. be of bacterial origin. However, thermal (temperature-related), pressure-induced or chemical influences can also cause inflammation.
Inflammations that develop after a root canal treatment are usually the result of a previously treated gangrene of the pulp (cell death of the nerves) and the resulting bacterial residues that are located in the branches of the root tip and were not completely removed during the rinsing process.
The term peri-implantitis is used for inflammation around the dental implant. Here, too, the cause are mostly invaded bacteria. However, a consequence of incorrectly loaded prosthetics (dentures) can also be shown by inflammation.
Read more on the topic: Risks of a dental implant
Symptoms
A distinction must be made here between acute and chronic osteomyelitis. The acute form is not so common due to the wide spread of antibiotics. If you suffer from it, your body temperature is increased, you feel down and you are not really fit, the number of white blood cells is increased and your blood pressure falls faster. Pus accumulates intra- or extra-orally, which can spread diffusely (please refer: Pus in the jaw). If the inflammation is left untreated, the tooth can loosen and bone tissue can die.
In chronic osteomyelitis, abscesses, fistulas or an inflammatory accumulation of substances usually develop in the lower jaw. In the more advanced stage, dead tissue can be rejected. The symptoms just mentioned include Tooth loosening can occur. Pain occurs because the supplying nerve is affected and its supply area is affected. This can lead to numbness of the area supplied by the nerve.
In both cases, a tumor can also be the cause, which must be clarified by means of a tissue sample (biopsy).
In the upper jaw, osteomyelitis is mostly limited to the alveolar process, which is thickened. The surrounding gums appear swollen and reddened. The upper lip and cheek region can also be swollen. The affected teeth are loosened and pus flows out. Abscesses, fistulas, etc. can also develop. Dead pieces of tissue are rarer than in the lower jaw and there is a risk of it spreading into the maxillary sinus.
Find out more about this under: Abscess in the upper and lower jaw
Earache
A possible symptom of an inflammation of the jaw is an earache. Due to the anatomically very close proximity between the jaw, especially the jaw joint, the external auditory canal and the middle ear, jaw problems can also spread to the area of the ear. Inflammation of the jaw can irritate certain facial and / or cranial nerves.
Read more on the topic: Pain in jaw and ear
Since these usually supply several areas, the irritation in this case can also cause pain in the ear area. In the case of an inflammation of the jaw, however, the earache usually does not occur alone, but is accompanied by other symptoms such as paralysis or pain in other areas of the face.
Can you have an inflammation of the jaw without pain?
In the case of inflammation in the jaw, a distinction can be made between an acute and a chronic form.
The acute inflammation is usually accompanied by severe pain, fatigue, fever and other symptoms. In contrast, chronic inflammation can be accompanied by phases with severe discomfort and phases without symptoms.
Depending on the location of the inflammation in the jawbone, pain-free phases are also possible. This is particularly dangerous as the inflammation can spread over a large area unnoticed. However, as soon as it gets into the area of a nerve, severe pain occurs.
diagnosis
In most cases, an X-ray provides a clearer indication of the disease situation, including in the case of jawbone inflammation. In acute osteomyelitis, cloudy changes can be seen after 2-3 weeks. They are lightened unevenly and continue to spread. Dead tissue can also be made out.
In this case, a quick method to clarify the disease situation is skeletal scintigraphy, which reveals changes after 48 hours. It provides information on how the bone metabolism is in different parts of the upper jaw. A radioactive substance is administered to the patient. The higher the metabolism of the affected area, the more radiation it emits, which is measured with a special camera. If bone metabolism is increased in one area, this indicates inflammation.
In the case of chronic osteomyelitis, the x-ray shows rather blurred, irregularly occurring lightening, in which a good bone structure can still be seen from time to time. Dead tissue appears as differently shaped pieces of bone that are slightly loosened.
therapy
Therapy with Antibiotics turns out to be the fastest helpful in acute jawbone inflammation. Antibiotic therapy is initially untargeted until an antibiogram provides more precise information about which antibiotics the pathogen is particularly sensitive to. This is then given in high doses for about 3 weeks. The earlier antibiotic therapy is started, the higher the chances of recovery, especially in the first few days. If there is an abscess, it will open. If carious teeth are to blame for the jawbone inflammation, they should only be removed after the inflammation has healed.
In the chronic course of the disease, the dead and poorly perfused tissue is removed and targeted antibiotic therapy is applied.
All teeth that are not worth preserving and represent a focus of inflammation will awayTeeth that have been loosened, but which one would like to keep, are stabilized in their position with a splint. The inflamed tissue is spooned scratched out.
The resulting hole in the bone is tamponade or filled with bone substitute material to which autologous blood and antibiotics are added.
If such an inflammation occurs in the upper jaw, it heals much faster than in the lower jaw, but unfortunately the bone structure there will not regenerate completely.
Which antibiotics are used?
There are three different types of jaw inflammation.
There may be ostitis, inflammation of the bone and blood vessels in the bone itself. There is also what is known as osteomyelitis. In this case, the bone marrow is affected by the inflammation. The third option is so-called periostitis. In this case, the inflammation spreads to the periosteum (the periosteum).
Antibiotic therapy is used in all forms of jaw inflammation. In most cases, penicillins are used.
If you have a penicillin allergy, clindamycin is the drug of choice. Both antibiotics work against a wide range of bacteria.
Read more on the topic: penicillin
Home remedies for inflammation of the jaw
Proven home remedies for inflammation of the jaw only relieve their symptoms, i.e. they work without adequately treating the cause of the inflammation.
External cooling of the jaw relieves pain. After 10-15 minutes, however, you should take an equally long cooling break. An attempt can be made to keep the focus of infection small by rinsing the inside of the mouth with disinfecting rinses. Patients also sometimes find chewing cloves helpful.
You might also be interested in this topic: Mouthwash
Which doctor treats the jaw inflammation?
In the case of an inflammation of the jaw, in most cases a dentist is visited.
The causes of an inflammation of the jaw are in most cases of dentogenic origin. This means that the cause usually lies in defects or inflammation of the tooth. An inflammation of the bone manifests itself in an X-ray image as a lightening (an area that is darker than the surrounding tissue).
In the event of an acute inflammation of the jaw, an antibiotic is administered for about 3 weeks to combat the inflammation. In the case of a chronic form, e.g. an abscess has developed that often first has to be removed. This is followed by antibiotic therapy to prevent further inflammation.
Is jaw inflammation contagious?
Inflammation of the jaw itself is not contagious.
In most cases the inflammation is deep. However, the degree of infection risk also partly depends on the original cause of the jaw inflammation. If, for example, periodontitis, i.e. an inflammation of the tooth support system, was the cause, this periodontitis itself is contagious.
However, infection can only occur if, for example, one partner is ill and both partners subsequently use the same toothbrush. Once the jaw inflammation has generally been treated with antibiotics, there is no longer any risk of infection.
Structure of the jawbone
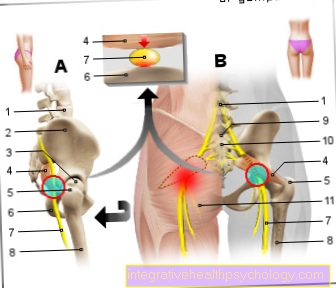
The bone tissue consists of cells and basic bone substance.
The outer and inner surfaces are covered by connective tissue structures, the periosteum (outer periosteum) and the endosti (inner periosteum). Bone cells include stem cells, osteoblasts (cells that are built up and remodeled), osteocytes (to maintain the basic bone substance) and osteoclasts (cells that break down and remodel).
The basic bone substance consists of an inorganic matrix with hydroxyapatite and an organic matrix. The bone has a lamellar structure and the individual lamellae are arranged in several circular layers around small canals, the Haversian canals. Blood vessels and nerves run in these channels.
Transverse canals, the so-called Volkmann canals, connect the Haversian canals with the periosteum, which is very sensitive to pain. The outer wall of the bone consists of a very compact layer, the compacta, the inner wall of the cancellous bone, which is very spongy. The bone marrow, the place where blood cells form, is present in the gaps in the cancellous bone.
Summary
Inflammation of the jaw can be caused by several factors, which must be considered in a differentiated manner.
A quick remedy is to be provided in any case, since a life-threatening situation can develop due to the possible further risk of spread of the bacteria, especially in the neck and face area. A specialist should be consulted immediately if symptoms occur. If the inflammation is recognized early, however, good antibiotic therapy can be used to achieve rapid recovery.