Epidural hematoma
introduction

A epidural hematoma is a bruise in the Epidural space is located. This one is between the extreme Meninges, of the Dura mater, and the Skull bones localized. Normally, the space mentioned does not exist in the head and is only caused by pathological changes such as bleeding.
It is different in the Spine: here the epidural space exists in every person and is with Vessels and Adipose tissue filled. Instead of the skull bones form here Vertebral bodies the outer limit. Hematomas occur more frequently intracranial on, so in the head. Epidural bleeding in the spine is possible, but less common in everyday clinical practice. An epidural hematoma is caused by a previous bleeding. This can be caused in various ways, but is usually traumatic (caused by mechanical influences, e.g. an act of violence or an accident). A hematoma in the head or spine calls for urgent medical intervention and can cause severe damage to the patient as well as to the death to lead.
causes
Because trauma-related bleeding is the prime cause of an epidural hematoma, bleeding of this type is closely related to the occurrence of traumatic brain injury. Most of the trauma is caused by an accident, particularly a car crash, in which the head is injured.
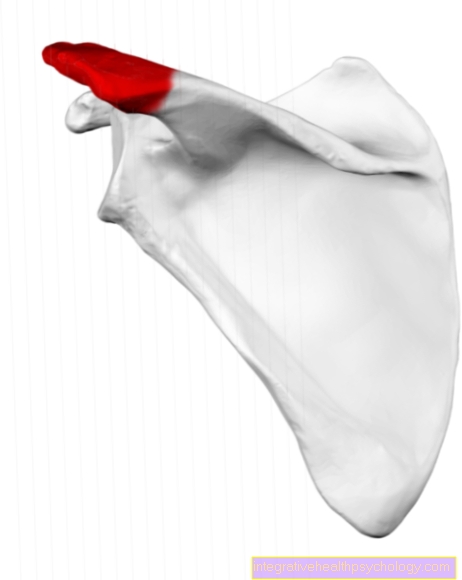
The extreme forces that act on the skull during an impact can damage vessels that cause bleeding and, as a result, bruises. A distinction can be made between arterial and venous hematomas. Due to the higher pressure in the arterial system of our circulation, a corresponding bleeding is more dramatic than a venous type. Usually the artery is affected by the injury, which supplies the meninges with blood - the arteria meningea media. If venous bleeding is the cause of the epidural hematoma, it is oozing bleeding that develops more slowly and also occurs less frequently due to the lower pressure in the system.
Since the epidural space in the spine exists physiologically (naturally), other causes are also represented here. In addition to traumatic effects, a spinal epidural hematoma can be triggered by vascular malformations, defects in the coagulation system or tumors. In addition to uncontrolled mechanical influence, the vessels in the epidural space of the spine can also be triggered by medical actions (iatrogenic), such as the administration of injections. The use of blood thinners as part of the treatment of a disease can also promote the development of an epidural hematoma.
Read more on the topic: What are the causes of a cerebral hemorrhage
according to PDA / PDK
The Epidural anesthesia (PDA) is a procedure in which the anesthetic is poured directly into the Epidural space (also epidural space) is injected. For a single administration of the drug, a needle is passed between the vertebral bodies and the anesthetic is injected directly. If the duration of the drug treatment is to last a long time, a stiff needle can also be used Peridural catheter (PDK). This thin plastic tube can remain in the epidural space for a long time and enables the patient to be anesthetized repeatedly.
There can be several complications with one intraspinal drug administration occur, including epidural bruising. If a vein lying in the epidural space is injured during the puncture, it usually occurs automatically Bleeding stopped without corresponding symptoms. If the bleeding does not stop by itself, a spinal hematoma forms, which is neurological and in the worst case scenario permanent consequential damage can trigger on the spinal cord. However, with a probability of 1 in 150,000, such a complication is extremely rare and can be corrected with the help of emergency surgery. Since coagulation disorders generally increase the risk of bleeding, bleeding occurs more often during an epidural (probability 1 in 3000).
Symptoms
The Symptoms with an epidural hematoma is very characteristic. In the majority of cases, after the patient is injured, one follows Faint. After the patient has cleared up and regained consciousness, it may happen that no symptoms are noticeable. A Phase of complete freedom from symptoms is not uncommon. An easy one Headache often accompanies this resting phase and is often perceived as a minor phenomenon.
In the course of the following 2 hours, the symptom construct slowly builds up. The headache worsens and nausea (possibly with Vomit) uses. This worsening of the condition should be alarming for both the patient and the treating person and should lead to hospitalization if this has not already happened. The Consciousness becomes cloudy again after a while and an increased sleepiness dominates the patient's appearance.
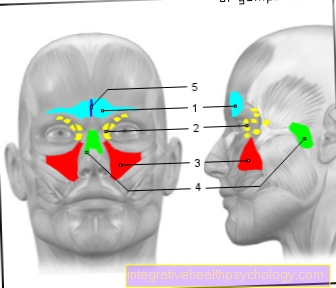
The expansion of the hematoma results in progressive compression of the brain tissue. Nerves can also be affected if they are close to the bleeding area. For example, one-sided pressure can enlarge the pupil (homolateral mydriasis), which is achieved through the participation of the Occulomotor nerve, which is responsible for their control, is caused. It can be on the opposite side of the body Motor disorders or for complete paralysisg come because the movement control in the brain is reversed.
The symptoms of an epidural hematoma must be Toddlers be viewed in a differentiated manner. Through the low bone hardness vessels can be more easily damaged by falls. The ductility of the soft bones and the incompletely closed fontanelles give the hematoma some leeway. The first symptoms usually only appear 6 to 12 hours after the accident occurs due to the compensation of the expansion. The clinical picture is similar to that of an adult. In addition to neurological symptoms, blood loss in the circulatory system is becoming more relevant in young children. The size of the head allows it to hold a relatively large amount of blood, creating a Lack of blood (Anemia) can develop.
For more information, also read: Cerebral hemorrhage symptoms
The clinical picture of one spinal epidural hematoma presents itself differently, of course The patient's consciousness remains unaffectedas long as there is no additional injury to the head (a combination of both injuries in serious car accidents, however, is not unlikely). The increasing pressure on the spinal cord initially leads to local pain before deficits manifest themselves below the hematoma. A Paraplegic Syndrome can be the result of the action on the spinal cord, with the patient initially losing his motor skills and developing sensory disorders. Surgery can often restore the previous condition.
Diagnosis
By the characteristic clinical picture of a epidural hematoma diagnostics is often abbreviated. The doctor's knowledge and interpretation can be supported or confirmed with imaging procedures. The clinical picture is due to the Symptoms staggered over time and the uneven pupil size marked. In addition, the one-sided failure of various body functions and the progressive deterioration of the condition can be interpreted as an indication of a bleeding. In many cases, a physical examination is impressive abnormal reflex status. The patient's reflexes are reinforced by an existing paralysis, while voluntary movement is not possible.
With the help of Computed Tomography (CT) can diagnose or confirm 90% of epidural hematomas. The hematoma appears in the CT image as lightened (high density; hyperdense), sharply demarcated area, which is biconvex (lenticular) the Skull bone from the inside. The one-sided pressure caused by the bleeding has probably shifted the midline of the brain to the healthy half of the head.
The Magnetic resonance imaging (MRT) can also be used for diagnostics. If a spinal epidural hematoma is suspected, MRI is increasingly chosen as the imaging method. The search for the cause can be carried out in the laboratory Control of the coagulation values and checking the Platelet count be accelerated if a traumatic origin of the bruise can be excluded.
Complications and long-term effects
An epidural hematoma can be a complication Entrapment Syndrome as a result of the ongoing pressure situation in skull entail. A distinction is made between two different locations. The upper entrapment is caused by the Displacement of the temporal lobewhich is located under the tentorium cerebelli (Cerebellar tent) pushes. This scaffold consisting of meninges sits on the Cerebellum (Cerebellum) and separates it from the Cerebrum (Telencephalon).
Due to its stabilizing and protective function, the cerebellar tent is relative robust built and not very movable. This displaces the temporal lobe towards the center and puts pressure on it Diencephalon (Mesencephalon), which contains important control centers of the human body. If the pressure increases, an epidural hematoma can cause death of the patient.
The nerve tracts that mediate the movement of the body (Pyramid tracks), run close to the diencephalon and are also compressed in the process. Does it come to a sudden Signs of paralysis, this can be a sign of incipient entrapment.
In addition to the upper one, there can also be a lower entrapment. This one as well life threatening process is mediated by the cerebellum, which is pushed down. It can happen that the cerebellum enters the Foramen oval (oval hole) is squeezed. The foramen ovale is located on the underside of the skull and represents the portal of entry of the Backmarks in the head. Likewise, the hole contains part of the Brain stem - especially those Medulla oblongata. Among other things, this is responsible for breathing control. If the cerebellum presses on the brain stem, it can lead to a loss of essential functions, for example Apnea come through which the patient dies.
The long-term effects can vary with prolonged or severe pressure on the brain as a result of the epidural hematoma. Symptoms of paralysis are usually reversible, but they can also be permanent if the brain is not relieved of pressure quickly enough. Furthermore, neurological deficits can occur that are related to the Localization of the bleeding related. For example, that Language center remain impaired even after a successful operation. About 20% of patients suffer permanent disability from such an injury.
At a spinal epidural hematoma possible long-term consequences also depend on the speed of medical help. All symptoms that arise in the course of the process can be completely reversible. Long-term impairment of the spinal cord through the bruise can also lead to permanent damage. As a rule, cross-sectional syndromes develop, in which the patient loses motor skills as well as the sensation of touch, temperature and pain from the bleeding level.
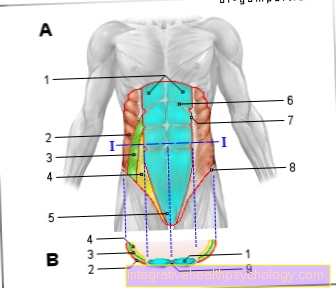
Effects on the spine and spinal cord
In the Spine there is of course not much space. That fills most of the space Spinal cord with the surrounding Liquor (Brain water) out. If there is a bleeding in the epidural space, a Hematoma, this can quickly affect the spinal cord. While the initial pressure can be very painful, but does not cause any damage, it begins Spread of the bruise cause neurological symptoms. Depending on the bleeding level, the segments below are affected by motor and sensory failures. At the height of the Thoracic vertebrae the arm and leg regions are conspicuous, below only the legs. In addition to movement and sensation, other bodily functions whose control center is in the spinal cord can also be restricted. So are Micturition disorders (Micturition = urinary control) a typical abnormality in severe spinal cord failure. The vertebral bodies themselves, if they are otherwise healthy, usually do not take any damage from the resulting pressure.The condition of osteoporotically weakened or otherwise already injured vertebral bodies can worsen due to an extensive hematoma.
Therapy / OP
At a epidural hematoma is it a medical emergency. In both intracranial and spinal localization, immediate action must be taken and the Admission to a hospital to be guaranteed. The standard therapy here is a neurosurgical operation. Medicinal treatment can be used as an accompaniment, but does not solve the problem in itself.
In the OP will the Skull bones initially carefully opened what is called Trepanation designated. On the one hand, this provides access to Bleeding site on the other hand, pressure is relieved - which is important for preventing long-term effects. After the tissue has been protected from further deterioration due to pressure, the hematoma can be cleared out. This involves scraping off coagulated blood and sucking off liquid blood. The vessel from which the bleeding originates is obliterated and then the wound is closed again. At a Surgery on the spine attention must be paid to the surrounding nerves exiting the spinal cord and spinal canal laterally.
forecast
Due to the serious complications, the death rate from epidural hematomas is relatively high. Even with a relief operation and removal of the bruise, the patient dies in 30 to 40% of cases. If the patient survives the injury, there is the question of consequential or long-term damage. A fifth of all survivors are permanently disabled from the disease. Exercise therapy and other supportive measures can increase independence in the case of existing disabilities. Half of the patients who are admitted with an epidural hematoma survive without any consequential damage and regain all abilities even with existing neurological symptoms. The prognosis of spinal hematomas is rather positive, since with competent treatment a complete remission (decrease) of the cross-sectional symptoms can be achieved.
Read more on the topic: What are the chances of recovery after a cerebral hemorrhage?



.jpg)