Stellate ganglion blockage
definition
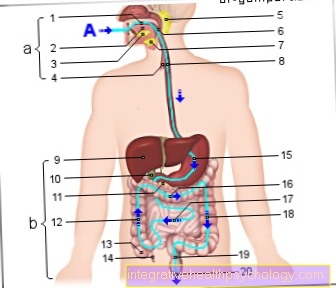
The stellate ganglion is a plexus of nerves in the area of the lower neck. It supplies parts of the head, chest and chest organs with sympathetic nerve fibers. In the case of a stellate ganglion blockage, these nerve fibers are specifically switched off by infiltration of local anesthetic. After a short exposure time, vasodilation (vasodilation), reduced sweat secretion and Horner's syndrome consisting of: constriction of the pupil (Miosis), Drooping of the upper eyelid (Ptosis) and receding of the eye into the eye socket (Enophthalmos).

Indications for a stellate ganglion blockage
This is one of the indications for stellate ganglion block complex regional pain syndrome (CRPS): After injuries in the arm area, adhesions in the area of the nerve plexus can lead to dysregulation of the sympathetic nerve. By numbing the nerves, symptoms can be reduced.
A nerve block is also an option in trigeminal neuralgia and post-zoster neuralgia. The sometimes severe pain can be alleviated in this way.Stellatum blockade can also be considered if Raynaud's syndrome is present. Here one makes use of the vasodilating effect.
preparation
In addition to a detailed anamnesis and explanation of the patient, the blood clotting is checked by means of a blood test. If the patient is taking blood-thinning medication, advice should be given about a possible break.
Before the procedure, an ECG should be written in order to identify possible cardiac arrhythmias that may be a contraindication. No special precautions need to be taken on the day of implementation. After the blockade, the patient is not allowed to drive for 24 hours and should not operate heavy machinery.
procedure
The stellate ganglion blockade is initially performed in the supine position with the patient awake. During the entire procedure, the vital parameters (blood pressure, pulse, oxygen saturation) are continuously measured in order to immediately counteract any possible circulatory decline. The ganglion is only anesthetized on one side in order to avoid life-threatening bilateral vocal cord paralysis.
The anesthetist first feels the carotid artery (External carotid artery). After carefully disinfecting the area in the lower area of the neck, the carotid artery is moved slightly outwards. The puncture is performed vertically between the artery and the trachea, while the cannula is advanced to the transverse process of the 6th cervical vertebra. The needle is advanced either blindly, and the attending physician must be able to feel and identify the surrounding structures well.
In patients with a larger soft tissue covering, the puncture can also be checked with an ultrasound. If the needle is correctly placed, after aspiration, 5-10ml of the local anesthetic (bupivacaine, mepivacaine) is injected. After removing the needle, the patient is seated immediately to cause the local anesthetic to sink. The local anesthetic is now distributed in the tissue of the lower neck and numbs the entire nerve network.
If the sympathetic nerve fibers are successfully blocked, the skin in the affected area is warm, dry and well supplied with blood. The circulatory and neurological status of the patient is then closely monitored. To achieve the desired effect, a series of 5-10 blocks is usually carried out at intervals of 1-3 days. The therapy should be carried out in a painless period.
Duration of a stellate ganglion blockade
Experienced anesthetists only need a few minutes for the puncture and injection. With preparation and subsequent monitoring, a blockade takes about 1 hour. If a series of blocks is carried out with up to 10 sessions at an interval of 1-3 days, the therapy can extend over a month.
What are the risks?
A possible risk is injection of the local anesthetic into the vertebral artery (Vertebral artery) that runs past the back of the transverse processes. If the local anesthetic is injected intravascularly (into the vessel), a seizure is immediately triggered. Therefore, the procedure should be performed with readiness for intubation. The spread of the local anesthetic in the tissue can lead to recurrent palsy, i.e. damage to the recurrent nerve (Recurrent laryngeal nerve). The consequences are hotness, coughing and even shortness of breath. If the recurrence is anesthetized on both sides, the vocal cords are completely closed and breathing is no longer possible in this case.
Therefore a Stellatum block is only carried out on one side. In addition, the nerve plexus of the arm can be numbed for a short time. Affected persons can temporarily move the arm / hand with difficulty (please refer: Brachial plexus paralysis). If a patient takes blood thinners or has a bleeding disorder, bruises can occur in the area of the puncture canal. The consequences are swelling, pain or symptoms of paralysis due to the narrowing of neighboring nerves.
Inserting the needle can injure the tip of the lungs and cause a pneumothorax. The affected lung shrinks and makes breathing difficult. If there is already a pneumothorax on the opposite side or if breathing has failed, a stellate blockade must not be performed! In extremely rare cases, the windpipe (coughing irritation) or esophagus are injured.
What results can be expected?
First, the effectiveness of the nerve block should be tested. For this purpose, at least two diagnostic punctures should be performed. If there is a significant reduction in pain after 4 days, the therapeutic blockade series can be started. After the 5th block, a break is taken to check the success of the therapy.
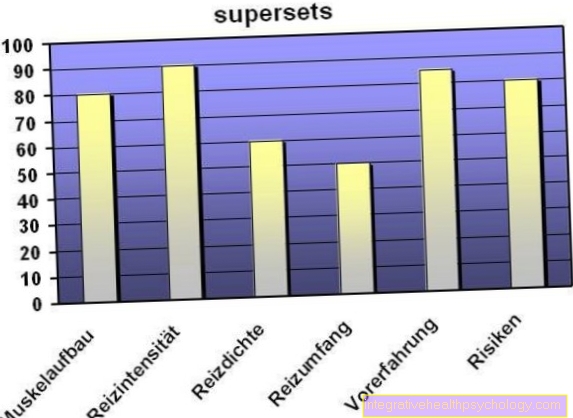
In order to be able to show the success of the therapy, it can be helpful to keep a pain diary. If pain occurs again, the series can be continued. Nerve blocks have a high placebo effect. It is always necessary to critically question the success of the therapy. The success rates vary significantly between 30-90% depending on the symptoms.
In order to achieve long-term success, additional physiotherapy and relaxation exercises should not be avoided.