cervical cancer
Synonyms in a broader sense
Synonyms in the broader sense: cancer of the uterine entrance, uterine cancer
English: cervical cancer / cervix cancer
definition
This tumor / cancer is the second most common tumor in women after breast cancer. 20% of all new cancers are cervical cancer (Cervical cancer).
It is believed that the cause of the cervical cancer is caused by the wart virus (Human papilloma viruses) is triggered.
Read more about the topic here: Human papillomavirus (HPV)

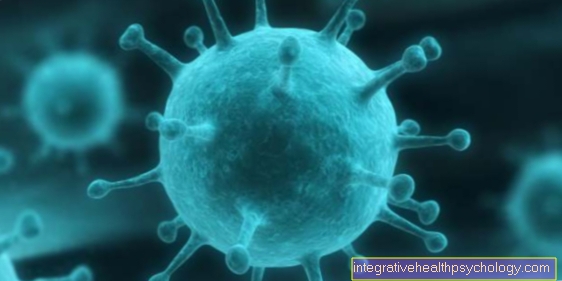
HPV virus
HPV viruses belong to the Papillomaviridae family. These non-enveloped DNA viruses are by no means all the same. It exist over 100 different typesthat can trigger different clinical pictures. The spectrum of possible diseases ranges from benign warts to malignant cancers such as cervical cancer or penile cancer.
One distinguishes so-called Low risk-Types, these include the HPV types 11 and 6, of the High risk-Viruses, to which for example the types 16, 18 and 33 belong. High-risk viruses can lead to the development of malignant diseases of the genital area, such as cervical cancer, penile / vulva and anal cancers. But these viruses can also cause cancer of the mouth and throat.
Low-risk viruses favor the development of benign warts.
The transmission takes place mainly through the Sexual intercourse instead of. Condoms do not reliably protect against infection, since skin contact is sufficient for transmission. The virus remains in the body after infection and can lead to illness after several years. However, an infection can also heal, especially in young women.
Occurrence in the population (epidemiology)
Of the Cervical cancer (cervical cancer) power 20% of malignant cancers in women. It used to be one of the most common cancers.
Today it is about half a million women worldwide cancer on second most common site of malignant tumors.
Every year ten to twenty new cases of less than 100,000 residents in the Federal Republic of Germany are added. The frequency of occurrence is greatest between the ages of 35 and 60. Preliminary stages can occur at a younger age.
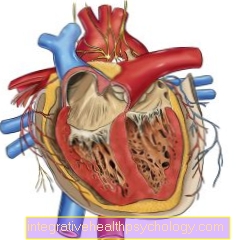
Anatomy and histology

- Uterus -
uterus - Uterine tip -
Fundus uteri - Uterine lining -
Tunica mucosa - Uterine cavity -
Cavitas uteri - Peritoneum cover -
Tunica serosa - Cervix -
Ostium uteri - Uterine body -
Corpus uteri - Uterine constriction -
Isthmus uteri - Sheath - vagina
- Cervix - Cervix uteri
- Ovary - Ovary
- Fallopian tubes - Tuba uterina
You can find an overview of all Dr-Gumpert images at: medical illustrations

- Uterus - uterus
- Uterine tip - Fundus uteri
- Uterine lining -
Tunica mucosa - Uterine cavity - Cavitas uteri
- Peritoneum cover - Tunica serosa
- Cervix - Ostium uteri
- Uterine body - Corpus uteri
- Uterine constriction - Isthmus uteri
- Sheath - vagina
- Pubic symphysis -
Pubic symphysis - Urinary bladder - Vesica urinaria
- Rectum - Rectum
Of the cervix puts the out of the vagina (vagina) The part of the uterus leading into the body of the uterus. The part of this cervix that protrudes into the vagina (i.e. the section further away from the body of the uterus is called the portio and is the most common place of origin of cervical cancer.
Natural changes in the cervical mucous membrane during sexual maturity are responsible for this: under hormonal control, the cervical mucous membrane (which contains small glands that form an antibacterially effective mucus) outwards towards the vagina to protect against ascending infections.
Before puberty, the vagina is covered only by flat, stacked surface cells (so-called squamous epithelium). Due to this Remodeling processes is the Mucous membrane of the anterior cervix (the portio, see above), particularly sensitive to bacterial, mechanical, i.a. Stimuli.
Frequent inflammations therefore favor the development of tumors on the basis of previously damaged cells.
The various previous damages (summarized as cervical intraepithelial neoplasias, CIN for short, i.e. as new formations of the cervix limited to the superficial cell structure, and divided into levels from I to III depending on the extent of the cell changes) initially do not grow into the surrounding tissue ( = invasive growth), but can be detected by smear examination and colposcopy (see below)
root cause

The exact origin of the cervical cancer is not known in detail. However, according to current knowledge, the disease is an example of a cancer caused by viruses.
Extensive studies have shown that infection with the human papillomavirus (HPV) is a prerequisite for disease. The virus is transmitted through sexual intercourse. Two of the approximately 200 different types of human papillomavirus (HPV) represent a particularly high risk (types 16 and 18); to other types of the virus (types 6 and 11) are e.g. Genital warts of the genital organs (so-called. condyloma acuminata).
Human papillomaviruses are, in the broadest sense, viruses that cause warts on the skin.
Infection with the human papillomavirus is not necessarily linked to cervical cancer. The body's self-healing powers prevent the disease from breaking out in around 80% of all those infected with the virus.
Bad hygiene and frequent partner changes increase the likelihood of illness, while male circumcision and childlessness lower the risk.
Read more about this under: Are genital warts contagious?
Symptoms and signs of cervical cancer
Symptoms rarely occur at first. Sometimes a discharge that smells sweet and Spotting (especially after sexual contact) first indications of a cervical cancer be. In the advanced stage, the tumor spreads further into the wall of the cervix as well as into the vagina, pelvic wall, rectum (rectum), and the connective tissue holding apparatus of the uterus in the pelvis (the so-called parametria).
Settlements (Metastases) of the tumor can initially spread via the lymphatic system, later also through ingrowth into blood vessels liver, brain, lung and bone (so-called hematogenous metastasis, i.e. settling on the bloodstream) resulting in severe pain.
diagnosis

Annual health check-ups are recommended from the age of 20, as infection with the cancer-causing virus can occur very early. The detection of cancer precursors is possible by means of smear examinations.The cells obtained in this way are stained for visualization (the method was developed by George Nicolas Papanicolaou, a Greek doctor and pathologist who lived from 1883-1962 and is still carried out today in a modified form). The assessment takes place in classes PAP (Papanicolaou) from I to V, according to a normal finding up to cell changes, the urgent suspicion of a tumor confirms the need for immediate clarification by taking a tissue sample.
Classification according to Papanicolaou
- PAP I - Normal cell structure
- The finding is normal, there are no abnormalities, check-up after one year as part of the cancer screening examination.
- PAP II - Inflammatory and metaplastic changes
- The cell changes are not suspect, mostly caused by bacteria or other germs, if necessary an examination after 3 months and a possible treatment of the inflammation.
- PAP III - Severe inflammatory or degenerative changes, an assessment of whether the
Changes are malicious is not possible with certainty- The finding is unclear; possibly antibiotic or hormonal treatment; short-term check-up after approx. 2 weeks; if Pap III persists, a tissue-based (histological) evaluation (histology) important.
- PAP III D - Cells show slightly to moderately atypical cell changes
- The finding is unclear; this change is mostly related to the common HPV infection. A check-up after 3 months is sufficient; a histological investigation is only necessary if it occurs again.
- PAP IV a - severe cell dysplasia or carcinoma in situ (precancerous disease)
- Histological examination with the help of a curettage (scraping) and a colonoscopy / hysteroscopy.
- PAP IV b - severe cell dysplasia or carcinoma in situ (early stage cancer), cells
a malignant cancer cannot be excluded- Requires a fine tissue (histological) clarification by means of conization (see below) or biopsy (obtaining a tissue sample), therapy depending on the findings and family planning of the patient.
- PAP V - Cells of a presumably malignant cancer (malignant tumor), tumor is clearly malignant
- Require tissue-based (histological) clarification by means of conization (see below) or biopsy (obtaining a tissue sample). Therapy: removal of the uterus (hysterectomy).
During the gynecological examination, the cervix is accessible by means of colposcopy (literally: “mirroring the vagina” from Greek kolpo = vagina, skopie = peek / look at). This diagnosis, which is used for the early detection of cervical cancer, was introduced in the 1920s by Hans Hinselmann. The cervix is examined with a special microscope (Colposcope) viewed under optimal lighting with six to twenty times magnification.
Using the acetic acid sample, precursors (so-called. Precancerous lesions) and changes in the mucous membrane associated with an increased risk of cancer are made visible (e.g. as Metaplasia designated transformation of uterine lining into vaginal lining as a result of constantly recurring inflammation; To a certain extent, however, this mucosal transformation is also normal and can be detected in all women after puberty).
However, since normal mucous membranes are also stained by the acetic acid sample, the dark brown to black staining of exclusively healthy cells using the so-called Schiller's iodine test is helpful to differentiate between healthy and diseased tissue.
The basis of this proof is the chemical reaction of the glycogen contained in normal cells (a giant molecule consisting of several thousand sugar components and serving as a storage medium) with iodine to form a brown reaction product.
Pathologically altered mucous membrane (so-called metaplastic mucous membrane caused by inflammation or cancer precursors), on the other hand, contains little glycogen and therefore stains little or no staining.
The colposcope itself is not inserted into the vagina, but positioned in front of it. To unfold the vaginal walls, the gynecologist uses a speculum (Latin: hand mirror; tube-shaped, funnel-shaped or spatula-shaped for insertion into natural body cavities). With special small forceps it is possible to remove small pieces of tissue and examine them under the microscope. In addition to the mere observation, a colposcope also enables the creation of photos and video recordings for documentation purposes.
The aim of colposcopy is to classify the degree of severity when a pathological change is detected. The decisive factors include Color, surface quality, and the dyeability of the suspicious part of the tissue with iodine. Superficial whitening of the mucous membrane (called leukoplakia) can be harmless or indicate an underlying cancer precursor. Red dots or bars (called "mosaic") correspond to the vessels reaching the surface and are always suspect for a malicious change.
So far, a positive effect in cancer prevention has not yet been proven. However, a colposcopy seems to us to be very useful as a preventive measure. The colposcopy is not included in the scope of services of the GKV (statutory health insurance).
Also read the article: The biopsy of the cervix.
Therapy of cervical cancer
There are different levels of treatment:
- Prevention (prophylaxis)
- Conization
- Removal of the womb (hysterectomy)
Pension options
There are very good preventive measures against cervical cancer, so there has been a clearer one in recent years Decrease in this disease in the industrialized nations. Primary prevention is to prevent infection with HPV viruses. For this purpose there is the HPV-vaccination (see below).
Secondary prevention is supported by the annual check-up at the gynecologist realized. Every woman, regardless of whether she is vaccinated or not, should undergo this examination. The investigation will Recommended from the age of 20. This check-up includes an assessment of the cervix by the gynecologist and a smear (cervical smear). This smear is taken from 2 places with a wooden spatula / cotton swab. The sample is then spread evenly on a slide and stained using the Papanicolaou staining method. Therefore, the test is also known colloquially as the PAP test. With this smear, precancerous and pre-existing cancer can be detected early so that rapid therapy can take place.
Vaccination against cervical cancer

Following promising results in animal experiments, scientists have now been able to demonstrate in clinical studies that a newly developed vaccine is highly effective with few side effects.
The vaccine consists of proteins that correspond to those from the envelope of the human papillomavirus. The vaccination stimulates the immune system to produce self-protecting proteins (so-called antibodies) against the viruses that cause cancer, comparable to training. The effect of the vaccination is enhanced by an auxiliary substance that also activates the immune system (a so-called adjuvant). Effective protection over 4.5 years for women between 25 and 55 years has been proven.
The vaccine was first approved in the US in 2006.
Vaccination against cervical cancer has also been possible in Germany since 2007.
However, since this does not offer 100% protection, it cannot replace preventive smear tests (the vaccine has so far only been effective against the two most dangerous high-risk types of the virus, which are responsible for around 70% of all cancers of the cervix).
Broad vaccination programs are planned for the population, as the human papilloma virus infection is high: between 70% and 80% of all women in Germany, Austria and Switzerland will be infected with HPV in the course of their lives.
The infection usually heals itself within 12 to 18 months, so that a positive test for the virus, for example, is in no way linked to an existing or later developing cancer. However, it is important to note that a vaccination is only of a preventive nature: an infection with the virus cannot be cured by it.
Therefore, it is planned, especially the age group of nine to twelve year olds (puberty) before the first sexual contact to vaccinate. The vaccination would not only benefit girls, but also boys: The vaccine introduced in Germany at the beginning of 2007 is also intended to protect against the viruses that cause benign warts of the genital organs (which are harmless in relation to cervical cancer and are therefore referred to as low-risk types) .
The future goal is to use vaccinations to limit cervical cancer and all preliminary stages to a minimum that can no longer be reduced.
Vaccination costs
For the prevention of cervical cancer, three vaccines are currently approved in Germany that protect against various HPV viruses. The vaccine Cervarix protects against the virus strains HPV 16 and 18, whereas Gardasil protects against the HPV types 16, 18, 11 and 6. The latest approved vaccine Gardasil9 also protects against the virus strains 31, 33, 45, 52 and 58.
The Cost per injection amount to about 155 euros. With three injections for basic immunization, the costs are 465 euros. If you only need two injections, it is 310 euros. The cost of vaccination will be for Girls between the ages of 12 and 17 are covered by health insurance. However, many health insurance companies also cover the vaccination up to the age of 26. It is therefore advisable to ask the health insurance company.
Conization
Tissue changes suspected of being cancer should be cut out of the cervix in a cone shape (so-called conization). An estimated 50,000 of these surgical interventions are currently carried out in Germany each year.
A general conization is not necessary in every case, but a stage-dependent procedure according to the individual findings in accordance with the current guidelines.
Removal of the uterus (hysterectomy)

In more advanced stages, the entire uterus is removed (med. hysterectomy) including the connective tissue holding apparatus, a vaginal cuff and the surrounding area Lymph nodes the means of choice (so-called Wertheim radical operation). Sometimes there are still radiotherapy and or chemotherapy required.
As with any cancer, it is important to follow up with care: every three months for the first three years, every four months for another two years and every six months after five years.


.jpg)