Gonarthrosis
introduction
The medical term "Gonarthrosis“Describes the Osteoarthritis of the knee joint. In osteoarthritis, the cartilaginous joint surfaces are the Knee joint attacked and worn out, which can be seen from the origin of the word. The word "arthrosis“ (Greek) means joint and the final syllable "-eyelet“Stands for non-inflammatory processes or changes in the basic state.
The osteoarthritis of the knee is an end point of various diseases that lead to a progressive one Damage to the cartilaginous joint surfaces lead and all with one wear (degeneration) of the knee joint.

Risk factors
In osteoarthritis of the knee it comes to progressive wear and tear of articular cartilage. One differentiates between primary and secondary osteoarthritis of the knee. The primary osteoarthritis of the knee, also called idiopathic, occur independently of other underlying diseases, for example in old age age-related wear and tear, on. Genetic causes are also discussed in primary osteoarthritis.
Secondary osteoarthritis of the knee is the result of traumatic events (Cartilage injuries, broken bones, operations), congenital or acquired Misalignment and strain on the knees (Bow-leg and knock-leg) or other underlying diseases.
These include metabolic diseases, such as Obesity or a Diabetes mellitus. But also Changes in hormonal balance can lead to cartilage and bones being built up incorrectly or increasingly broken down, for example in gout.
These different diseases can lead to osteoarthritis of the knee, as destroyed cartilage cells cannot regenerate themselves. In addition, the cartilage substance is broken down by enzymes that are attracted by the destruction of the cartilage cells. In this context, the cartilage loses its most important properties, strength and elasticity, and loses its thickness and resilience. If the strain on the knee is not reduced under these conditions, it can Changes in Synovial membrane, bone and Tapes come. Other changes that are caused by osteoarthritis can be detected in the context of imaging procedures, e.g. X-ray or CT.
Frequency distribution
The frequency of the Osteoarthritis of the knee joint varies depending on the age group between 12 and 55%, is however in the advanced age one of the most common joint diseases.
Appointment with a knee specialist?
I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Symptoms
Often, osteoarthritis can already be diagnosed on an X-ray without the patient having already experienced symptoms. The typical symptoms of osteoarthritis are Joint painthat at the beginning under stress and after unfamiliar activities occur. The patient often finds it difficult to describe the pain, the joint is often perceived as stiff. Also Swelling around the joint can occur and additionally limit mobility.
Read more on the subject here Knee Pain - What Do I Have?
As the disease progresses, the pain under stress turns into one Pain when moving. The pain is felt most strongly at first, especially when moving after long periods of rest (Starting pain), but after a few steps it settles again until it occurs again after prolonged exertion (Fatigue pain).
When the pain occurs in the joint permanently even at rest osteoarthritis is at a late stage.
It often happens then Bad posture, the muscles are restricted in their function and the joint capsule shrinks. Due to the constant pain, movements are deliberately avoided, which stiffens the joints (Contracture). The osteoarthritis symptoms can rarely be identified acoustically as crepitation (Rubbing noise) perceive. This occurs when the joint is so severely damaged that the joint surfaces can no longer be guided smoothly past one another.
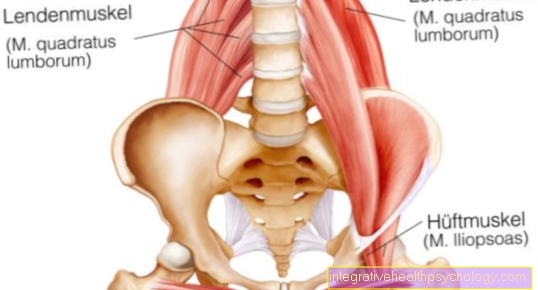
In the case of osteoarthritis of the knee, the symptoms provide an assessment of the spread of the osteoarthritis. Pain during passive movements, i.e. without muscle exertion, suggest changes that can be made limit to the joint. In contrast to this, osteoarthritis is no longer limited to pain during active movements, but also has due to the restricted movement Muscles and Tendons included.
The knee joint can usually be turned around Bend 180 degrees and around 10-20 degrees stretch. With osteoarthritis of the knee, these movements are restricted. In the initial stages, the ability to bend first decreases and then the extension. The pain intensity increases particularly when going down stairs or when walking downhill. Osteoarthritis of the knee progresses faster than osteoarthritis in other joints, as the reduced strain on the leg muscles means that the cartilage that is still present is also supplied with less nutrients.
to form
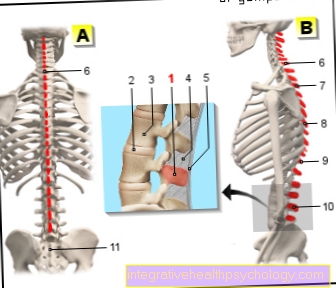
Because the knee joint is from three sections Together, different forms of osteoarthritis of the knee are distinguished depending on their location. Any group can individually affected be or together with the others. A group provides that Femoropatellar joint represents, i.e. the joint surface between the thigh bone (Femur) and the kneecap (patella).
The retropatellar arthrosis that occurs in this area manifests itself primarily in the Sit, at the Climb stairs or in Transition from crouching to standing with Pain.
The joint between the thighbone and the shinbone (Femorotibial joint) can be divided into two further groups. One distinguishes the medial gonarthrosis, i.e. the inside of the femorotibial joint from the lateral gonarthrosis (Outside). If all three areas are affected by osteoarthritis, one speaks of one Pangonarthrosis.
If the lateral gonarthrosis occurs with a X-leg deformity (Valgus), one speaks of valgus gonarthrosis. The varus gonarthrosis includes the medial gonarthrosis O-leg misalignment (Varus) together. The arthrosis is of a secondary nature and is promoted by the uneven strain on the knee joint, which results from the deformity.
diagnosis

Knee joint pain can have various causes. First, the doctor will go through a conversation and carefully examine the characteristics of the pain to make a suspected diagnosis. This will change in the course of the clinical examination hardening. During the examination, the doctor pays attention to the appearance of the legs and knees. They are especially important Leg axes, the Musculature and the Gait pattern. The shape of the knee can also tell whether there is swelling or something similar.
The doctor then manually examines the knee and checks whether there is swelling due to an effusion, checks the mobility and tests whether crepitation can be heard when the knee joint moves. Some specific tests enable the examiner to determine whether osteoarthritis of the knee is responsible for the pain.
roentgen
However, diagnosis also includes imaging procedures to. Especially the X-ray of the knee joint is a quick and inexpensive way to diagnose osteoarthritis. Recordings of the knee are made in two planes, which can be supplemented with special recordings if necessary.
In the X-ray you can Typical signs of osteoarthritis be detected. This includes the Narrowing of the joint space, which is the first visible sign of osteoarthritis on radiological images. Due to the increasing stress on the bones in osteoarthritis, the bone is strengthened, so to speak, the bone tissue thickens (subchondral sclerotherapy) under the former or remaining cartilage layer of the joint.
As part of the bone changes, new bone tissue is also formed, especially in the edge area of the joint, one speaks of osteophytic peripheral structures. In advanced stages of osteoarthritis form Rubble cysts out. These cysts arise from the undamped contact between the bone surfaces in osteoarthritis. The resulting small traumas trigger the death of small regions in the bone. These regions show up in the X-ray image as Recesses in the bone.
In summary, the x-rays give a very good overview of the processes in the joint. Through the Ultrasound examination can mainly be a Knee joint effusion be detected. Other possible investigations are the Computed Tomography, Magnetic resonance imaging or one Skeletal scintigraphy.
Also read our page MRI of the knee.
Classification according to degrees of severity
Different degrees of severity can be distinguished in the course of osteoarthritis of the knee. The classification is based on the appearance and degeneration of the articular cartilage.
Grade 1
At this stage the articular cartilage appears slightly frayed. At this stage, the affected person's knee joint is functional not yet affected and mostly as well symptom-free.
Grade 2
Now you are through osteoarthritis wide fraying on the surface of the cartilage and half-layer tears recognizable. But the patient is mostly still at this stage symptom-free.
Grade 3
However, from grade 3 gonarthrosis leads to the patient Pain and Function losses. The first thing you notice in grade 3 is that the surface of the cartilage in the knee joint is no longer smooth. The cartilage is from deep cracks and craters interspersed and very frayed.
Grade 4
In contrast to grade 3, the bone at grade 4 is no longer completely covered by cartilage. Lots of places are exposed (Bald bone). The bone rubs against each other on this. It comes to serious complaintssuch as stiffeners or joint effusions.
therapy
Gonarthrosis is a progressive (progressive) Clinical picture, which is why in addition to the Pain relief also the Progression should be contained. Numerous conservative forms of therapy try to reduce the suffering and to keep the joint as long as possible.
Conservative therapy of gonarthrosis
The conservative methods of treating osteoarthritis of the knee are limited. Relief measures are recommended, including on the one hand dampening the shock in the knee special orthopedic buffer heels on the shoes, but also on the other Weight reduction. Non-drug measures are furthermore physiotherapy, physical therapy and physical therapy (Electrotherapy / cold and heat applications), which is used to maintain or build up the atrophic thigh muscles.
The medical therapy serves to relieve pain and reduce inflammation in the knee joint. This is particularly common nonsteroidal anti-inflammatory drugs (NSAIDs) used. These include the following drugs: Ibuprofen, Aspirin® or Diclofenac. However, due to their side effect profile, these medications should not be taken over a long period of time without prior consultation with a doctor as they can be harmful to the digestive tract, liver and kidneys. Also at Cardiovascular disease their use should be weighed very carefully.
An orthopedic specialist can also prescribe stronger morphine-based pain relievers. These substances should be considered because of their side effects careful be taken and the dosage adjusted and controlled by a specialist. If necessary, the pain therapy can also be performed by a Pain therapists (anesthetist) can be further optimized.
The drug therapy is im Initial stage It is used as an accompaniment or is used to alleviate existing symptoms after conservative or surgical therapy. In addition, drug therapy is used in patients who Contraindications for further therapies exhibit.
Please also read our page Knee osteoarthritis - which drugs help?
The drug too Cortisone is used in the therapy of gonarthrosis. However, not in tablet form, but applied locally to the knee joint. The cortisone reduces the current irritation and relieves pain and effusion. However, when the cortisone is administered in crystalline form, the cartilage is roughened even further. However, nothing changes in the poor initial state of the knee.
This process is technically not too difficult to carry out, but it is Risk of infection relatively high for intra-articular injection. The application of the drug must under sterile conditions The patient's skin must be disinfected very precisely and the tools required must be sterile. Otherwise, bacterial infections from the knee can spread throughout the body and become one sepsis (Blood poisoning) to lead.
Another way to improve the suppleness of the joint is to inject Hyaluronic acid the effectiveness of which is assessed very differently.
Also read: Knee osteoarthritis - when can it be treated conservatively?
Knee supports for osteoarthritis of the knee

It is also possible to use Knee braces. However, gonarthrosis bandages are only helpful to a very limited extent, as they cannot directly influence the wear and tear of the cartilaginous joint surfaces. Nevertheless, the use of gonarthrosis bandages can be recommended by the doctor, for example to ensure stability during movement and the practice of knee-friendly sports (Swimming, yoga).
Knee orthoses for osteoarthritis of the knee
In contrast to the bandages, which are mainly made of soft material and have a compressing effect, the Knee braces. Orthoses are made of harder material and stabilize the knee more strongly. In addition, the knee orthoses with their belt systems can reduce pain and the Increase quality of life. Operations can be delayed somewhat by using knee braces.
Depending on which region of the knee is affected, the orthotics can provide relief. If several regions are involved, Knee guide orthoses be applied. Such orthoses can also individually made to measure depending on how badly the knee is affected.
Operative therapy for osteoarthritis of the knee

In the surgical therapy of osteoarthritis of the knee, joint-preserving and joint replacement Differentiate operations. In the case of damage to the knee joint that is not too advanced, an attempt should be made to operate to preserve the joint. Misalignments of the leg axes, like Varus or valgus deformities (O- or knock-knees), which lead to arthritic changes in the joint in the long term, can be caused by a Corrective osteotomy corrected in order to prevent the development of osteoarthritis of the knee or to relieve the affected area in the case of an existing osteoarthritis of the knee.
At an initial stage, the cartilage can also be arthroscopically (through a joint specimen) to contain the progression of the damage and to reduce the irritation of the joint.
Please also read our page Arthroscopy of the knee joint.
Since the basic problem of osteoarthritis is the decrease and destruction of the joint cartilage, various measures are used to try to reduce the amount of cartilage receive or restore. One possibility is that Microfracturing (also abrasion arthroplasty or Pridie drilling). During this procedure, the exposed bone is injured. This leads to an exit of in the course of the healing process Stem cells from the bone, from which fiber cartilage is formed. This cartilage fills the gaps in the articular cartilage and closes the previously existing defect. A disadvantage of this procedure is that the newly formed fiber cartilage not so tough is like the articular cartilage.
A further development of this process is the Cartilage transplant In the laboratory, healthy cartilage cells are grown on a collagen fleece and this fleece with the cartilage cells is surgically attached to the damaged area in the joint. This procedure is on Patients under 50 years of age restricted having a fresh cartilage defect with a Size over 2.5 square centimeters exhibit.
Also with the Cartilage-bone transplant should be the patient younger than 50 years be. However, it is better here if the cartilage is damaged less than 25 millimeters is. In the process of cartilage-bone transplantation, small cylinders of bone are removed from areas of the joint that are not under stress, and the defective areas are replaced. The removal points are in turn filled with the removed cylinders from the defective region.
Joint replacement operations are operations in which the joint affected by osteoarthritis of the knee is against a Knee prosthesis is exchanged. There are different types of prostheses. There are so-called Sled prosthesesthat guarantee a one-sided resurfacing. This type of prosthesis is only used when just a bone roll (either outside or inside) is damaged, as is and still is often the case with osteoarthritis in connection with leg axis misalignments all ligaments in the knee intact are.
The so-called Total knee replacement refers to a complete surface replacement of the knee joint. You replaced all articular surfaces in the knee joint, occasionally even the back of the kneecap. It is only important that the stability in the knee is largely guaranteed by the strap systems.
In the event that not only bones and cartilage but also the Tape apparatus of the knee joint is destroyed is one axis-guided knee prosthesis indicated, which stabilizes the knee in the longitudinal axis.
All prostheses are made of special metals, plastics or ceramics. Titanium alloys can also be used for patients with metal allergies.
Every prosthesis consists of at least three parts: A share for the Thigh (Femoral component), a share for that Shin (Tibial component) and one Plastic overlay for the tibial component. Depending on the bone quality and the physical activity of the patient, the knee prosthesis can either be in the bone cemented in be or cementless be anchored. A mixed form of both is possible.
Also read: Knee osteoarthritis - when do you have to operate?
OP risks
As with all operations, you can numerous complications occur: damage to surrounding structures (Soft tissue, nerves, vessels) with blood loss, swelling and pain, thrombosis, infections and wound healing disorders. In addition to the general complications, there are also special complications for operations with knee prostheses. Just like the wounds, so can the prostheses infect bacterially and this infection can lead to a sepsis (Blood poisoning) to lead. However, these are very rare complications that usually do not occur.
Furthermore leads lack of exercise of the knee joint after the operation Adhesions and Scarring the prosthesis what a Restriction of movement may result. In addition, the prosthesis may loosen over time. This loosening expresses itself with Pain, one Instability in the knee joint and in extreme cases a misalignment of the leg axis. Such loosening of the prosthesis must be corrected, otherwise the surrounding bone will be damaged.
In general, it should be said that knee prostheses are not durable for life. To 15-20 years the prostheses must be replaced.
Summary
Gonarthrosis is a progressive clinical picture, in which the articular cartilage in the knee joint is destroyed and then bony remodeling in the joint is carried out. The causes of osteoarthritis of the knee are diverse. Next Aging processes and genetic predisposition can also different clinical pictures or a Obesity favor the development of gonarthrosis. The gonarthrosis also results from Incorrect loadscaused by misaligned legs or excessive strain on the knee (pport, profession) can be justified.
The clinical picture initially leads to symptoms Pain when moving and later also in peace. The functionality of the knee is limited, it can too Stiffeners come. The doctor reproduces the diagnosis of gonarthrosis physical examination and based on imaging procedures. Conservative and drug therapy is limited, in most cases one will be surgical joint replacement necessary from a certain point.