Cataract
Synonyms in a broader sense
Lens opacity, cataract, old age cataract
English: cataract
Medical: cataract
definition
Cataracts (like the “green star”, this term should no longer be used because of the risk of confusion with the “other” star). The cataract (cataract) generally denotes any form of lens opacity. The normally transparent lens lies behind the pupil in humans and belongs to the optical apparatus with which the eye can adjust the focus.
In advanced cataracts, a gray haze can be seen behind the pupil. This is where the term “cataract” comes from: “gray” because of the veil and “star” because of the rigid gaze that can be observed in blind people.
The word cataract originally comes from the Greek (cataracta) and means "waterfall". At that time it was assumed that the gray veil was a congealed liquid that had flowed down in front of the pupil. The resulting clouding of the field of vision gave the impression of looking through a waterfall.

How common is cataract?
In those over 65, almost 100% have cataracts and around 50% notice the visual disturbances when they have reached the age of 75. Every year between 400,000 and 600,000 people in Germany are operated on for cataracts (cataracts).
Overall, if left untreated, cataracts are the leading cause of blindness in the world. The most common form is the old age cataract = cataract.
Recognizing a cataract
What are the symptoms of cataracts?
During cataracts, the lens in the eye becomes cloudy. This clouding is also known as a cataract. One speaks of cataracts as soon as the opacity of the lens has a severe impact on daily life. The clouding makes the lens impermeable to light and there is a gradual decrease in vision up to complete blindness and a deterioration in visual acuity (VA). Cataracts are the leading cause of blindness in the world.
The main symptom of cataracts is deteriorating eyesight.
Due to crystals that come from altered structural proteins in the eye lens, the light no longer reaches the retina unhindered and the lens loses its transparency.
The gray veils are typical signs of an incipient cataract. Contrast and colors are increasingly difficult to see, as if through fog. The comparison, as seen through a steamed-up window, expresses how limited those affected are, especially in the later course of the cataract. At this point in time, the gray coloring of the pupil is usually also visible to others, and those affected no longer have so-called “red eyes” in photographs.
In addition, the incident light is additionally scattered by the cloudiness and thus leads to an increased sensitivity to glare in backlighting, which can be another sign. This is clearly noticeable when driving in the dark and is very uncomfortable.
Contrasts or colors are also only perceived in a weakened manner. In addition to a decrease in eyesight, cataracts often also have double vision.
Existing presbyopia improves seemingly for no reason, which can also be seen as a sign of a cataract. In the short term, there may be an improvement in near vision, so that glasses no longer have to be worn while reading for a certain period of time. Various mechanisms, such as the thickening of the lens, change the refractive power in favor of myopia. However, this improvement decreases again in the course of the disease due to increasing cloudiness.
90 percent of all cataract cases are cataracts (Cataract senile). If left untreated, a cataract can lead to blindness. In many older people, however, cataracts cause their eyesight to deteriorate so slowly that an operation is not necessary.
Read more on the topic: Cataract symptoms
Comparison of cataracts and healthy eyes


How is a cataract diagnosed?
The specialist in ophthalmology makes the diagnosis of "cataracts" based on the symptoms described and by examining the lens on the slit lamp (device with which the eye is illuminated) and visual acuity. If the opacity is so pronounced that it is not possible to examine the fundus, an ultrasound examination can also be useful for cataracts.
It can be carried out quickly, is painless and can provide information about:
- thickness
- consistency
and - Changes
of the sonicated tissue, here the posterior segment of the eye.
How can cataracts be classified?
Comparison of a pair of eyes. On the left, the milky color of the pupil from the cataract was noticed, while on the right a healthy eye is shown.
The types of cataracts (forms of cataracts) are first classified according to the acquired and the innate types. The acquired cataract forms make up about 99% of all cataracts (cataracts).
Acquired cataracts include:
- the old age cataract (over 90% of all acquired cataracts) = this disease is usually referred to as "cataracts"
- Cataracts caused by common conditions such as:
- diabetes mellitus
- Galactose intolerance
- Diseases of the kidney / kidney failure
- Tetanus (tetanus)
- various other muscle and skin diseases
- Cataracts from eye infections
- Postoperative cataracts after vitreous removal
- Injury-related (traumatic) cataracts after
- Accidents
- foreign bodies penetrated
- Electric shocks
- Radiation exposure
- toxic (pharmacological or poisonous) cataracts
- Cortisone - containing drugs
- certain eye drops used in glaucoma therapy (glaucoma = glaucoma especially parasympathomimetics)
Strictly speaking, congenital cataracts (cataracts) can also be classified according to acquired (congenital) and genetically determined (congenital) development in the birth canal and therefore also with development that is otherwise uninfluenced by the outside:
- acquired in the birth canal through viral infections
- rubella
- Mumps (rather rare)
- genetically conditioned
- either inherited X-linked
- Trisomy 13 and 15
- Down syndrome and other syndromes
- metabolism-related in galactosemia (an intolerance to a certain sugar component)
This is different with congenital cataracts, because the child's vision has yet to develop. This is a very complicated process and can only happen in the first few years of life.
If the development is disturbed during this time, life-long visual disturbances up to blindness arise.
Treating a cataract
How is a cataract treated?
So: When diagnosing a cataract or "cataract" do not be unnecessarily alarmed, in most cases it is a natural phenomenon that can be treated well nowadays.
Read more on the topic: Cataract therapy
How does the cataract follow-up treatment work?
Since the artificial lens can be used to adjust the focus close up or at a distance (Accommodation) is no longer possible, the patient still needs glasses. Either for the distance or reading glasses for close up.
After a cataract operation, you should initially take some rest for the next 4 - 6 weeks. That means no unnecessary hard physical work, no competitive sport, if possible not going swimming, avoiding saunas and also not allowing pressure on the eyes.
Before there were artificial lenses, star glasses were prescribed. Nowadays this is only necessary very seldom if either no artificial lens could be used or there is an intolerance to contact lenses.
The star glasses are very strong plus glasses with approx. 12-15 dioptres. This means that you perceive all objects about 25 percent larger. But here, too, care must be taken that the difference in refractive power between the right and left eye is not too great, since otherwise an image will be perceived differently in size in both eyes. For this reason, star glasses often only had one lens with the particularly strong refractive power.
Contact lenses are better if there is no lens on one side because the closer distance to the eye also means that there is a smaller difference in image size.
Can a cataract be operated on?
If the cataract-induced lens opacification deteriorates significantly and normal vision is severely impaired, surgery is the only treatment option. This operation is now a routine operation in Germany and is almost always successful.
- Procedure: The cataract operation can be performed on an outpatient or inpatient basis. An inpatient stay after such an operation takes about 2-3 days. Both eyes are never operated on at the same time. Initially, only one eye is subjected to the procedure and, after it has healed, the other eye. The operation is usually only performed under local anesthesia. For this purpose, an anesthetic is either dripped directly into the eye to be operated on in the form of drops or it is injected near the eye with a syringe. During the subsequent operation, the clouded eye lens is removed and replaced with a new plastic lens (so-called. Intraocular lens). The most commonly used procedure is the so-called Phacoemulsification. A small incision is made in the shell of the eye lens (Lens capsule) set. The lens nucleus can then be liquefied by means of ultrasound and sucked off together with the lens cortex through the incision in the capsule. The new, artificial lens is then inserted into the capsular bag. This is usually painless for the patient. Finally, the eye is covered with an ointment bandage, which should be left for a few days, especially at night, for protection.
- After the operation: There are some things that need to be considered urgently after the eye operation. Under no circumstances should the operated eye be rubbed. In addition, it should not come into contact with water for the first few days. Special care is therefore required when washing your hair. Physical exertion should only be resumed after consulting a doctor. This also applies to participation in road traffic, which should only be practiced after a satisfactory eye test. Since the eyesight can fluctuate greatly in the first few weeks after the procedure, you have to wait before fitting new glasses. Most patients also need sunglasses after the operation, as the new lens is more translucent than the old lens.
- Time: The time when cataract surgery should be performed depends on the individual patient. On the one hand, it depends on how far the eyesight is already restricted and whether it is already hindering the patient's everyday life; on the other hand, age plays a major role. Younger patients who, for example, still actively participate in road traffic, should be operated on if they have less vision loss than older people who are mainly in the home. In congenital cataracts, the child should be operated on as soon as possible, as this is the only way that they can learn to see without complications.
- Lens types: The new lens used can be individually adapted to the patient. Various materials are available (e.g. polymethyl methacrylate = plexiglass, silicone, acrylic). In addition, the new lens can produce one or more focal points and can be set for near or far vision. Nowadays mostly "soft“, Foldable lenses used. These can be transplanted into the eye in a rolled up form and therefore require a smaller incision than the "tough" Lenses. This reduces the occurrence of complications. Finally, special lenses are also available, but they are not suitable for all patients. They can contain special color filters and also enable varifocal.
- Complications: The operation is very successful in the majority of patients (90% have better eyesight). However, comorbidities in the patient can significantly influence the success of the operation. The operation is for patients with other eye diseases, such as retinal diseases, circulatory disorders of the optic nerve or age-related macular degeneration (AMD) bring about less improvement in visual performance. Another risk of the operation is that the capsular bag will be damaged when the clouded lens is removed and it will then no longer be possible to insert a new lens. As a rule, however, alternative methods are available in such a case, in which the new lens is inserted, for example, directly behind the pupil. Other complications include swelling or detachment of the retina, the vitreous humor slipping out when the lens capsule is damaged, or infections in the surgical area. However, these are usually easy to get under control with modern drugs.
- Post-cataract: In some cases, several weeks or months after the operation, there is a gradual loss of the initially improved visual performance. This so-called secondary cataract can, however, easily be remedied in an additional small operation with a laser.
Read more on the topic: Cataract surgery
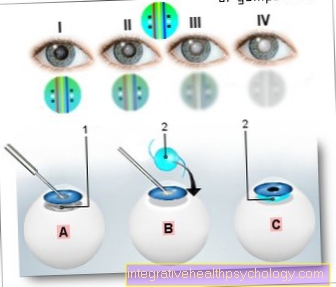
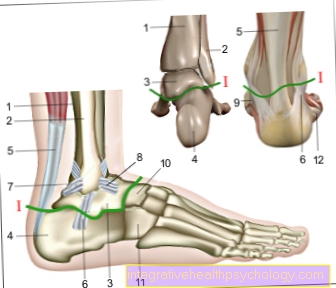
Cataract surgery
(cataract)
- Cloudy lens of the eye
- Intraocular lens (IOL)
Procedure:
A - distance the murky
Eye lens
B - introduction one
Artificial lens (IOL)
C - IOL is implanted
Development stages:
I - Cataracta incipiens
II - Cataracta provecta
III - Cataracta matura
IV - Cataracta intumescens
You can find an overview of all Dr-Gumpert images at: medical illustrations
Can cataracts be treated with the laser method?
In addition to the surgical operation method, there is now the possibility of treating cataracts with lasers. With this new technology, a special laser (Femtosecond laser) the cuts in the eye that were previously made manually by the surgeon. The laser sends light pulses in the range of femtoseconds (1/14 of a second), which releases a lot of energy that can be used for the surgical incision. The cuts are planned beforehand by the surgeon and continuously monitored via a microscope during the operation.
Treatment with the laser should enable a more precise and safer therapy of cataracts and better quality of vision through more precise alignment of the artificial lens. Irritation symptoms that can occur on the eye after surgical treatment are also rarer: the laser only needs a fraction of the ultrasonic energy to smash and suction the old lens, as with conventional surgery. Another advantage is that the corneal curvature of the eye is also present, as this can be corrected by the laser during the operation. The procedure can be carried out under local anesthesia using eye drops and on an outpatient basis. But because of the high acquisition costs, treatment with the femtosecond laser is not yet possible in all clinics.
Cataract prevention
What causes a cataract?
The causes of cataracts (cataracts) are very diverse.
The most common is old age cataract (cataracta senile = cataract), which cannot be attributed to any specific cause. Most likely, this form of cataract can be attributed to the deterioration in the supply of nutrients to the lens in old age.
Other acquired cataracts can be better assigned to the cause.
For example, injury to the eye (Traumatic cataract) and radiation exposure (especially X-rays, infrared rays and UV light).
Chronic inflammation of the choroid (Cataracta complicata), as occurs with bacterial or viral infections, can of course also cause a cataract. Malnutrition (especially vitamin A deficiency, often a problem in developing countries) and many diseases that affect lens metabolism (such as diabetes mellitus) are possible factors in cataracts.
Basically everything that can disrupt nutrition and oxygen supply to the lens.
A cataract does not always have to be acquired, but can also be congenital (Cataracta congenita) or during pregnancy (Connatal cataract) result from intrauterine, i.e. prenatal, infection of the mother (for example from measles and rubella virus).
Read more on the topic: Infections in pregnancy
Then you have to operate on the cataract as quickly as possible, because otherwise the risk of weak vision (Amblyopia) consists.
Read more on the topic: Cataract causes

Figure eye
- Optic nerve (Optic nerve)
- Cornea
- lens
- anterior chamber
- Ciliary muscle
- Vitreous
- Retina (retina)
Course of a cataract
What is the prognosis for a cataract?
The prospect of better vision after a cataract operation is in principle very good. The prerequisite is, of course, that no other eye disease disturbs vision and that any underlying disease is treated appropriately. In the treatment of cataracts in children, it is particularly important that the therapy is started on time.
Side note:
Sometimes so-called "anti-cataractics" are prescribed. These are drugs that are supposed to work against clouding of the lens. There is currently no proven effective drug for cataracts (cataracts)!
What complications can cataracts have?
Rare complications of cataract treatment include rupture of the posterior capsule and bacterial infection.
In most cases, the bacteria are not transmitted by unclean instruments, but rather come from the patient's conjunctival sac itself. Patients with a weak immune system (e.g. AIDS) or general diseases such as diabetes mellitus or neurodermatitis are particularly at risk.
A special late consequence of the cataract operation can be the after cataract. A clouding of the posterior capsule is called a cataract. The opacity is due either to a change in the tissue or to a regeneration of cells on the lens surface (lens epithelial cells) that were not completely removed during the operation.One can then try to cut through the central part of the posterior capsule with a laser or to remove the regenerated cells with a suction device.
Further questions about cataracts
Is there a replacement with an artificial lens?
In addition to wearing special star glasses or contact lenses, the removal of your own lens and the simultaneous replacement with an artificial lens can also be considered as therapy. Surgical removal of the lens should be considered as soon as the cataracts drastically restrict everyday life.
The lens of the eye is made up of three parts: the capsule, the cortex, and the nucleus. When the lens is removed, the capsule is retained and the new artificial lens is inserted into it. The surgical procedure is carried out as an outpatient procedure under local anesthesia. Before the operation, the exact strength of the new artificial lens is calculated individually for each patient, which is based on the total refractive power of the affected eye.
The intraocular lens (IOL) is the most widely used medical implant worldwide. It is an artificial lens that is available in various material and lens types, so that a suitable lens can be found for every patient. The lenses can be made of PMMA (Plexiglass), Silicone or acrylic. The latter two materials are foldable and therefore require a smaller incision to be made. However, they can only be used in the manufacture of posterior chamber lenses, while PMMA can be used for anterior and posterior chamber lenses. A classification according to the place of implantation is also possible: there are lenses that are inserted behind the iris (posterior chamber lenses) and lenses that can be placed in front of the iris (anterior chamber lenses). The method of choice are posterior chamber lenses, as these cause fewer complications and the location has proven to be the best.
Another classification is based on the number of existing focal points: Monofocal lenses are the standard model of intraocular lenses, they only generate one focal point and enable sharp vision in the distance or near. However, with this model, glasses for near or far must always be worn even after the operation, since the artificial lens cannot change its curvature and so the adaptation of near and television (Accommodation) not possible.
Multifocal lenses, on the other hand, have several focal lengths and should enable sharp vision near and far. Therefore, glasses do not have to be worn for most everyday activities, but glasses may be necessary in the dark or to read small letters. The disadvantage of multifocal lenses is poorer contrast vision than monofocal lenses, greater sensitivity to diaphragm and less sharp vision.
The decision which type of lens to insert must therefore be made for each patient individually according to their needs. A regenerative cataract can occur months to years after the operation, which manifests itself in a renewed deterioration of vision. Then another surgical procedure may be necessary.
What is the history of the cataract?
The cataracts (cataract) treated by the so-called Starstecher.
A cut was made in the side of the eye, the so-called cataract needle was pushed up to the lens and the lens was pressed down to the base of the eyeball. As a result, the view was clear again, even if it was no longer possible to focus. However, infections often occurred, which not infrequently led to blindness.
Such operations were carried out in this country in the Middle Ages. Mostly by traveling wound healers who offered their services at festivals and fairs. They could therefore often not be prosecuted if they became blind weeks later. The composer Johann Sebastian Bach was treated like this in both eyes. He did not recover, went blind and died as a result.
Figure cataract
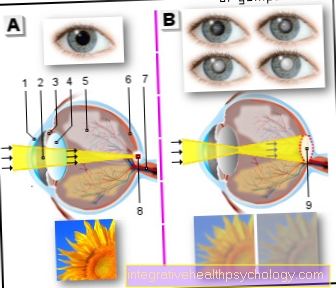
Cataract (cataract)
A - clear lens
(healthy eye)
B - clouded lens
(Cataract eye)
- Cornea - Cornea
- pupil
- Iris - iris
- Eye lens - Lens
- Vitreous - Corpus vitreum
- Retina - retina
- Optic nerve (2nd cranial nerve) -
Optic nerve - Punk-shaped, sharp figure
on the retina - Scattered light on the retina out of focus
You can find an overview of all Dr-Gumpert images at: medical illustrations

.jpg)


















.jpg)