Hip osteoarthritis
Synonyms
Arthrosis of the hip joint, coxarthrosis, coxarthrosis, arthrosis deformans, osteoarthritis, osteoarthritis deformans, arthrosis deformans coxae, coxarthrosis
Also osteoarthritis of the knee joint: Knee osteoarthritis, Gonarthrosis
Medical: Coxarthrosis
English: hip arthritis
Definition of hip osteoarthritis
The term "Hip arthrosis / hip arthrosis“ (= Coxarthrosis or coxarthrosis) includes all degenerative diseases in the area of Hip jointcaused by illness (e.g. congenital disorder of the functional unit femoral head - acetabulum or circulatory or metabolic disorders, ...), Accident (e.g. Femoral neck fracture) or wear and tear.
Common to all causal diseases is the increasing destruction of the joint cartilage, which ultimately also affects other joint structures such as the joint capsule, bone and the associated Musculature harms and one Hip osteoarthritis causes.
Stages
Hip osteoarthritis (Coxarthrosis) can, depending on the condition of the articular surfaces and function in different stages to be grouped. This staging also enables doctors to do one Assessment about the Severity the present osteoarthritis and also serves to Assessment of the appropriate therapy.
At Grade 0 are the Articular surfaces of the hip still intact and smooth. Of the Cartilage is healthy and elastic.
At Grade 1 shows a roughened cartilage surface. The cartilage can also be reduced in its mass and softer than healthy cartilage.
At Grade 2 lies a visible damage to the articular cartilage in front. Still that is Cartilage coating still intact.
Against points Grade 3 already a significant damage to the cartilage which can affect up to 50-100% of the entire cartilage layer on the joint surfaces.
Grade 4 is finally the furthest advanced so that the Cartilage worn out completely becomes and the bone has become visible. The patient also has one here Loss of movement and often permanent pain.
Appointment with a hip expert?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The hip joint is one of the joints that are exposed to the greatest stress.
The treatment of the hip (e.g. hip arthrosis, hip impingement, etc.) therefore requires a lot of experience.
I treat all hip diseases with a focus on conservative methods.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Signs of hip osteoarthritis
Hip osteoarthritis (Coxarthrosis) expresses itself in the initial stage with diffuse pain in the hip area after prolonged exposure. Initially, the pain can only occur through exercise, long hikes or climbing stairs. The disease progresses and the protective one Cartilage layer on articular surfaces increasingly less.
Of the After all, wear and tear becomes more and more evident until he too Pain with light exposure caused. The symptoms appear more and more frequently until they finally do stay permanently and also appear at rest. This is typical of advanced osteoarthritis of the hip Start-up pain after a long period of rest or after sitting for a long time. The pain subsides as soon as the person concerned has warmed up a bit.
Furthermore, it can also be caused by the wear and tear of the joint Friction occurs that can even be heard from outside can. Some patients also report feeling like her Hip joint is blocked. In addition to the characteristic complaints Side effects on. Due to the pain in the hip, many patients adopt a balancing posture and may go wrong. Because of this bad posture, after a while Back pain occur.
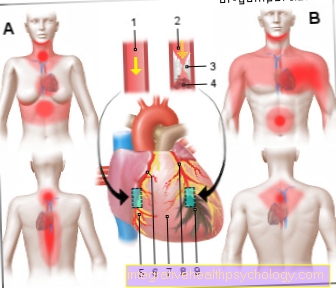
Hip pain / pain with osteoarthritis of the hip
You are searching for the cause of your Hip pain or you don't know exactly what is causing your hip pain?
Then let yourself be guided by our diagnostic Hip pain guide and come to the most likely diagnosis.
If it is known that you suffer from hip osteoarthritis and are in pain, we recommend our topic: Hip osteoarthritis pain - what can I do?
Age
In cases where the Cause of hip arthrosis is unknown (= primary hip osteoarthritis) hip arthrosis usually only develops in old age (Malum coxae senile), so usually only after the 50th-60th Age.
Frequently includes osteoarthritis both sides of the Hip joint.
Arthrosis of the hip joint, which are due to hip joint diseases that have not completely healed or anatomical variants in the femoral head or socket area (= secondary hip osteoarthritis), usually appear earlier and usually only affect one side of the hip joint.
Medically, one-sided joint involvement is called monoarticular.
Gender distribution
Since women are more likely to take a Hip dysplasia suffer and the cartilage is less resilient than the male cartilage due to its nature, women tend to Hip osteoarthritis as men.
Illustration of the hip (CT pelvis)

- Spine
- Iliac blade (os ilium)
- hip joint
- Femoral head
- Femoral neck
- Symphysis
- small rolling hillock (trochanter lesser)
- large rolling mound (greater trochanter)
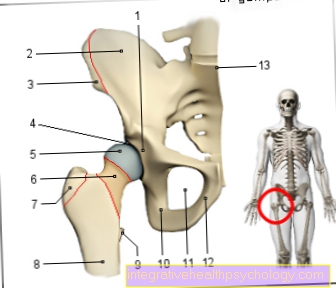
- Acetabulum - Acetabulum
- Iliac scoop - Ala ossis ilii
- Iliac crest - Iliac crest
- Articular lip of the acetabulum -
Labrum acetabuli - Femoral head (= femoral head) -
Head femoris - Femoral neck - Collum femoris
- Great Rolling Hill -
Greater trochanter - Femoral shaft -
Corpus femoris - Small rolling hill -
Lesser trochanter - Ischium - Os ischii
- Hip hole - Obturate foramen
- Pubic bone - Pubis
- Lumbar and sacrum kink -
Promontory
Three bones fuse to form the hip bone:
Ilium, pubic bone and ischium
You can find an overview of all Dr-Gumpert images at: medical illustrations
frequency
Since wear and tear as a trigger for hip osteoarthritis must ultimately be seen as the cause, it does not seem surprising that the risk of hip osteoarthritis increases with age. Studies show that from the age of 70, around 70 to 80% show signs of wear and tear on the hips and / or other joints.
This is a major risk factor for the development or acceleration of an existing hip arthrosis Obesity (Obesity).
Risk factors
Overweight:
Obesity has an aggravating effect on the aforementioned preopthritic changes. Thus, the occurrence of a Hip osteoarthritis as one of the Consequences of being overweight elevated. If there is already arthroplasty in the hip joint, the excess weight usually increases the pain. Obesity has an aggravating effect, but is not an isolated cause and is therefore not the only one causing osteoarthritis.
- Incorrect loadswhich, for example, as a result of poorly positioned acetabular cups (Hip dysplasia), unfavorable femoral neck angle (Coxa valga antetorta), etc. arise.
- endocrine factors (hormonal factors), e.g. a cortisone-producing tumor
- genetic influences, familial accumulation of hip arthrosis due to inherited hip dysplasia and cartilage quality
X-ray of the hip joint (hip arthrosis)
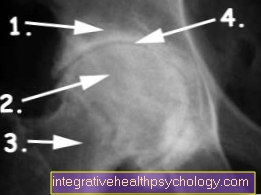
- Acetabulum
- Femoral head
- Femoral neck
- used joint space
diagnosis

What should be examined to diagnose hip osteoarthritis?
Clinical diagnostics:
- Assessment of range of motion and pain in motion
- Assessment of the gait pattern
- Leg length difference
- Muscular atrophy
- Assessment of tender points
- Assessment of neighboring joints
- Assessment of blood flow, motor skills and sensitivity
Apparative diagnostics:
Necessary examinations:
- X-ray image: Pelvic overview recording (BÜS)
Useful investigation in individual cases:
- X-ray image: axial / lateral view
- X-ray: functional images and special projections
- Sonography (Ultrasonic)
- Computed Tomography (CT)
- MRI of the hip (Magnetic resonance tomography / NMR)
- Scintigraphy
- Clinical-chemical laboratory for differential diagnostics
- Puncture with synovial analysis (tissue examination of the synovial membrane cells)
As a rule, osteoarthritis is limited to one or more joints, and in most cases it initially remains symptom-free for years. Even if you can diagnose coxarthrosis, i.e. the wear and tear of the hip joint, on the X-ray, pain or pain-related movement restrictions etc. are not necessarily present.
Depending on the disease, the increasing destruction of the hip joint is initially in the foreground. The first cracks appear in the articular cartilage, which increasingly expand and subsequently become a result of small, dying cartilage abrasion particles Synovitis (Synovitis) trigger. It is she who then sometimes causes very severe pain in the patient. Osteoarthritis alone is not painful! The increasing pressure on the joint tries to reduce the same pressure by increasing the joint surface. This leads to bone additions. The consequences of the changes caused by destruction and deformation in the area of the acetabulum, as well as capsule shrinkage and bone growth, are reflected in a painful reduction in function.
The x-ray shows worn-out articular cartilage, which can be recognized by the absence of a joint gap. The changes are particularly clear when you compare them with an X-ray image of a healthy hip (see above).
Consequences of hip osteoarthritis
- Pain
The descriptions show that hip osteoarthritis as such is a chronic disease that develops over the course of several years. Nevertheless, there are phases of acute pain, one then speaks of so-called activated hip arthrosis.
- The first clues usually include a feeling of stiffness and a rather diffuse joint and muscular pain (= Myalgia, hard instep). In addition, so-called overload pain occurs more and more frequently, as well as joint pain, which occurs especially early in the morning (after sleeping) and after prolonged sitting, the so-called starting pain after resting. This initial pain usually disappears as soon as the joint "arrived“Is. However, it can recur after long periods of running, standing or working with a feeling of muscle fatigue. One then speaks of what is known as fatigue pain. Occasionally, there can also be so-called pinching pain in the groin area. They are, for example, caused by detached osteophyte particles (osteoarthritis-related attachments). Entrapment pain is suddenly shooting and usually associated with severe pain. Later, there is stress pain with stress-dependent free intervals, which then ends in a more or less pronounced rest pain in the end stage.
- Localization of pain:
Groin, outside hip (Trochanteric region), Glutes, front of thighs to knees. Since a radiation of pain into the knee is possible, the patient may misinterpret the pain. If the knee is unremarkable during an examination, the attending physician should always think about possible hip diseases.
- Restriction of movement:
Depending on the severity of the pain, different movement restrictions occur in one Hip osteoarthritis on. As a rule, the first restriction is the rotation (Internal rotation), then the ability to splay, which can be considerably restricted under certain circumstances, becomes more and more difficult. The is also listed below Leg shorteningwhich occurs when the patient is no longer able to fully straighten their hips. One then speaks of a so-called flexion contracture, which can lead to functional shortening of the leg. It is worth mentioning that the restriction of movement is initially caused by the painful muscle tension, while it is later caused by the capsule shortening.
- Disturbances of the gait pattern - The patient usually avoids painful movements with osteoarthritis of the hip. As a result of hip osteoarthritis, it is noticeable that patients tend to lean more over the diseased hip joint when walking (this appears as a staggering gait)
- Reduction of the muscles in the buttocks and thighs.
Shortening of the legs, up to 3 cm is possible.
forecast
1. Natural course
The course of a Hip osteoarthritis is subject to many variables that do not allow an exact prognosis to be made for the individual case:
- The individual course
- The various causes of hip osteoarthritis, which in addition cannot always be clearly defined.
It is therefore not possible to give a scientifically exact prognosis with regard to the course of the disease and pain, the possible need for conservative or surgical therapies.
What is certain, however, is that the degree of osteoarthritis increases with the duration of the disease.
2. Prognosis after certain therapeutic procedures
- Conversion osteotomy / corrective osteotomies
Here, primarily, a pressure reduction is brought about. It is important to mention, however, that the more the arthritis stage and age, the lower the chances of success of these surgical procedures. You can find out more about this further down in the text.
- Hip Arthroplasty
The likely success after implantation of a artificial hip joint is very important to achieve complete freedom from symptoms. The exchange rate, i.e. the exchange of components of the hip joint, is approx. 0.5% per year, after 10-15 years the annual exchange rate increases. You can find more about this in the description of the artificial hip joint.
Further on the topic: Therapy of hip arthrosis
Preventing hip osteoarthritis
The arthrosis is a disease that often occurs at an advanced age and then often already one causes enormous damage to the joint Has. It is therefore all the more important that those not affected, but also those who already suffer from osteoarthritis, prevent it and stay active.
Moderate exercise, which does not stress the joints too much, can counteract the wear and tear of the cartilage. Suitable sports include Cycling, swimming, walking and cross-country skiing. From Doctors advise against sports that put a lot of stress on the joint and pose a risk of injury.
In addition, physical measures such as Massages, physiotherapy, heat and cold treatments act preventively by the Promote blood circulation and thus the joint structures with important nutrients supply.
A healthy diet and age and size adjusted weight are also very good. Overweight should try her with a healthy diet To reduce weight, because the joints are also stressed by an additional weight, and so is the Sports is much more difficult. If you already have osteoarthritis, a healthy diet can relieve and delay the symptoms. Patients should be on To a large extent do without noxae such as nicotine, alcohol and caffeine.
Sport and hip osteoarthritis

Hip osteoarthritis is a widespread disease. Many of those affected are alive without proper explanation in the mistaken belief that they arthrosis got because of them possibly too much exercise have driven. Eventually, they often stop exercising, but that is exactly the wrong approach. But exercise can also be good and useful for osteoarthritis.
Through the Move becomes in the joint space the Production of synovial fluid stimulated. This is very important for the intake of Nutrients and water for the cartilagecovering the articular surfaces. The cartilage becomes like this smooth kept and this counteracts increased wear and tear with existing osteoarthritis. Without exercise, the cartilage will not be supplied with nutrients. Osteoarthritis makes the cartilage rough and brittle until it eventually loosens. This can lead to the fact that the bone is exposed and thereby strong pain caused.
Accordingly, exercise can in a healthy measure Slow down osteoarthritis and also relieve the symptoms. The patient can decide for himself how much physical activity he or she can do and which sport is beneficial. Doctors recommend sports that do not stress the joints too much, but still move continuously to a certain extent. These sports include Cycling, swimming, aqua jogging and walking. Additionally can strength-building gymnastics exercises be performed.
Doctors and physiotherapists also advise osteoarthritis patients Targeted training of muscles. You can use this to create a Support and relieve damaged hips more. What kind of sports and to what extent can be done, a patient can also do in one Sports rehabilitation center work out with doctors and therapists. Care should be taken that the sports no risk of injury represent. If there is pain, the patient should stop exercising and take a break. Initial Stress pain or also the typical sore muscles can occur, but should subside after a while. At a acute inflammation or a relapsing worsening of osteoarthritis, should briefly renounced the sport until the inflammation subsides.
Exercise / gymnastics
The Hip osteoarthritis is used in medical terminology as Coxarthrosis designated. It is one progressive wear and tear of the cartilage surfaces of the hip joint. The patient experiences more and more Pain and notices one Deterioration in movement. With targeted exercises the wear and tear of the cartilage surfaces should be delayed. Regular gymnastics should also the Strengthen muscle groups.
In addition to light sports like Walking or Cycle can do gymnastics exercises very good at home be performed. Before the patient begins his exercises, he can do the Hip muscles warm up a little by standing with one leg on a sports bench or a thick book, for example. The free leg can now be moved easily forwards and backwards. So can Prevents strains or injuries to the various muscles become.
An exercise for Strengthening the gluteus muscles takes place on a mat in the supine position. The legs are conveniently set up parallel to each other. Now the buttocks are stretched upwards. The upper body, pelvis, buttocks and legs should now line up. This position should only be held for a short time, after which it can be repeated several times. At the beginning, for example 15 repetitions and the exercise is then slowly increased.
The little one Glutes can be trained while standing. This requires a chair or a wall to hold on to. The patient stands up to the back of the chair so that he can hold on to it and has a secure stance. The upper body should be kept in an upright position. Now we stretch one leg to the side as far as possible and move it upwards. The foot can be turned outwards while moving. This makes the effect on the small buttocks muscles noticeable. The upper body should stay in the starting position and not make any compensatory movement. This exercise can also be done depending on the patient's ability as often as you like be repeated.
Classic squats are very good for Training the front thigh muscles suitable. To do this, the patient first stands upright and the feet are about shoulder-width apart. The knee is now bent, but the knee should not be bent beyond the feet. Before straightening your legs again, hold the position for a brief moment if possible. This exercise can be done in a similar way in a step position with the legs about half a meter apart.
At the end of the exercises, the Hip muscles still loosened and stretched become. To do this, you again need a chair, on whose seat one leg is first placed while the other leg remains on the floor. Now the upper body is pushed forward and the leg is bent on the chair at the knee. The hip is stretched. The position is for a few seconds and then repeat the exercise on the other side.













.jpg)