Haglund exostosis
definition
Exostoses (or singular exostosis: from ex = out, out and os = bone) always denote in medicine Over legs, so additional compact bones, the after Outside to grow.
Mr Patrik Haglund was a Swedish orthopedist and surgeon after whom this exostosis is named.
The terms Haglund exostosis, Haglund syndrome, Haglund's pseudoexostosis can be used synonymously.
anatomy
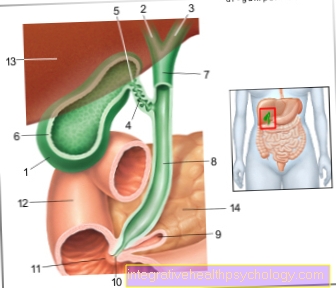
One of seven tarsus bones is the Calcaneus (the calcaneus). This forms the heel. On the calcaneus, more precisely on the Calcaneal tuberosity sets the Achilles tendon on. In this area it can be too bony extensions (Exostoses) are coming. An exostosis on the upper edge of the calcaneus, where the Achilles tendon attaches, is distinguished from an exostosis on the sole edge of the calcaneus. One speaks of cranial (upper) resp. plantar (on the sole) Heel spur.
Haglund's exostosis is the term given to the exostosis at the upper edge of the calcaneus in the area of the calcaneal tuberosity
frequency
A Haglund exostosis can be at about 10 percent of the population. However, not all those affected suffer from the symptoms typical of Haglund syndrome.
Appointment with ?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
Athletes (joggers, soccer players, etc.) are particularly often affected by diseases of the foot. In some cases, the cause of the foot discomfort cannot be identified at first.
Therefore, the treatment of the foot (e.g. Achilles tendonitis, heel spurs, etc.) requires a lot of experience.
I focus on a wide variety of foot diseases.
The aim of every treatment is treatment without surgery with a complete recovery of performance.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Cause and origin = ethiopathogenesis

In the Haglund exostosis (also Haglund heel) there is an increased ossification at the base of the Achilles tendon at the heelwhich makes the sufferer especially when wearing shoes Tenderness feel in this area.
The cause of the ossification has not yet been fully clarified. For one, there is the theory that the Haglund exostosis innate other experts suspect that the disease is also secondary Overload the Achilles tendon with the following Achilles tendonitis or badly seated Footwear can be caused. It is discussed whether a combination of these factors can also be the cause, whether the Haglund exostosis is partly congenital and can be worsened by incorrect / overstressing the heel.
This theory is supported by the fact that the Haglund exostosis is very common boys, physically active People occurs. The pressure of the edge of the shoe on the calcified tendon attachments in particular provokes the pain and is often secondary Bursitis in this area. These manifest themselves in severe discomfort when walking, pronounced pressure pain and, in many cases, swelling, reddening and overheating of the tissue.
Symptoms
Not every person with one Haglund exostosis suffers from ailments that can be traced back to this protruding bone.
trigger for Symptoms can be too strong athletic stress, wrong footwear (chronic pressure on the area of exostosis) or Misaligned feet be.
Constant strain on the surrounding structures leads to characteristic complaints. The reason for this is one irritation up to inflammation of the Achilles tendon, of Bursa between the Achilles tendon and the calcaneus (bursa subachillea, in case of inflammation one speaks of the bursitis subachillea) or the periosteum of the calcaneus.
This is noticeable by the following symptoms:
- Pain on pressure on the lower achilles tendon / the Attachment point on the calcaneus
- Pain in the field of heel above all under stress (e.g. sport)
- swelling and Redness of the heel area
Diagnosis
Often the description of the Pain and the typical local findings (Redness and Tenderness over the heel) already suspects a Haglund syndrome. To back up the diagnosis, a X-ray image of the foot and in particular the heel where the exostosis described can be seen.
A Subachillic bursitis can by means of Ultrasound examination the affected region can be detected.
therapy

Initially, Haglund's exostosis should always be attempted conservatively, i.e. without surgery.
Conservative therapy options
Usually one is sufficient for this Relief of the affected area. This is achieved through one Change the sport-) Shoes. Soft shoes are preferred. In addition, the shoes should not end at the level of the exostosis in the heel area. In addition, special manufactured insoles help to correct causal misalignments and thus prevent permanent irritation of the exostosis.
If this is not sufficient, there is a possibility physical forms of therapy alleviate the discomfort. This includes the use of cold- and Heat treatments, as well as local Ultrasound therapy. In particular, this should bring about a decrease in the inflammatory activity or the irritative state.
Also the Shock wave therapy offers a way to alleviate the discomfort. Here, high-energy ultrasonic waves are used to inflammation to reduce and Limescale deposits to minimize. However, the costs for shock wave therapy are usually not covered by health insurance.
In addition, various Medication i.a. be used for pain relief. Often a combination of cortisone and local anesthetic injected into the painful area. While the local anesthetic takes the pain away, cortisone causes the inflammation to decrease. In addition, classic painkillers can be taken temporarily for severe pain.
Operative therapy options
If the conservative measures show no improvement over a period of 9 to 12 months, surgery should be considered.
Here the Bony prominence removed with a chisel. With chronic inflammation of the bursa (Subachillic bursitis) this may also have to be removed. Also the Achilles tendon becomes part of the operation away and then using Bone anchors reattached to the heel.
Around 80% of the operated patients are after the operation symptom-free. After the operation, a Plaster splint be worn for a few weeks before the foot can be fully loaded again. The full Sports ability is with a complication-free course after three months reached.
However, the surgery offers some Complications. So it happens, among other things for the training of Scar tissue in the operating area, which in turn is very painful can be.
insoles
Orthopedic footwear can help alleviate the symptoms of Haglund exostosis. The aim is through targeted upholstery or Recesses in the shoe insoles the burden of the ossified transom at the heel reduce.
There are, for example, special Haglund pads that cushion the heel in the shoe and thus prevent overstimulation of the heel including the tendon attachment. One variant is custom-made Heel cups made of silicone, which can be inserted into different shoes at will. In addition, it is important in general spacious shoes with if possible high shoe edge to wear, as this also puts as little pressure as possible on the painful area.
Deposits, the one slight increase effect of the heel (by about 1cm) can also help to relieve the insertion of the Achilles tendon. are other misalignments of the feet one of the causes of the Haglund exostosis, these can also be corrected using orthopedic shoe insoles. Since in connection with the Haglund exostosis there is often a Flatfoot deformity occurs, deposits that Longitudinal vault of the foot and bring it back to its anatomically correct position.
In summer it is recommended to wear shoes open heel region to wear. Running shoes should be individually adapted and sit optimally, as complaints occur especially after running stress.
Operative treatment
Surgical treatment of Haglund's exostosis is an intervention that is possible Specialists should be reserved. Usually this operation is done endoscopicthat means it's only one small cut necessary, through which the surgeon has access to the ossified zone on the calcaneus. Of the Bony prominence it will then worn away and the calcaneus as a whole narrowed. At the end of the procedure, the patient is often given a special one Shoe put on, which serves to stabilize the foot in the normal position and additionally with Cork boards is equipped for heel elevation.
This shoe is worn continuously for a few days (including at night) and is only removed to assess the wound. After about 4 days the patient may start with a light load on the operated foot. The heel is first around with the cork sheets 2.0-2.5cm increased so the Achilles tendon relieved becomes. Wound healing disorders are also prevented in this way.
After about a week Depending on the patient's complaints, the foot can be fully loaded again. To ten days the stitches are usually removed. One closes physiotherapy treatment which especially the mobility in the upper ankle should promote. The patient can then train against slight resistance on the bicycle ergometer.
After about four weeks can then begin that Heel elevation gradually increasing to reduceso about seven weeks after the operation to return to normal footwear can be tried, but a heel height of approx. 1 cm should first be inserted in normal shoes. Only after at the earliest ten weeks can the patient again without restriction burden. With heavier running loads, however, a wearing of Stable shoes recommended.
The complete treatment is finally after about 14-20 weeks completed. Overall, good results can be achieved with operative therapy. In particular the adequate aftercare and the consistent wearing of the Stable shoes with heel raised is relevant for the surgical outcome. In some cases, relapses can still occur afterwards, but these are mainly due to insufficient removal of the ossified upper leg or due to inadequate follow-up care.