Urea decreased
What does a decrease in urea in the blood mean?
Urea is a metabolic product that is produced when proteins (proteins and amino acids) are broken down in the body. These are first converted into ammonia, which is toxic to the body, and then broken down into urea in the so-called urea cycle. This can then be excreted through the kidneys.
A decrease in the urea level in the blood is far less important than an increase. In most cases, the lower value is due to insufficient protein intake or an increased protein requirement. As a result, the lowering of the urea in the blood is mostly harmless.

What symptoms can indicate a low urea?
Since low urea levels can have various causes, it is difficult to determine specific symptoms for such a level. Symptoms of malnutrition, which is one of the most common causes, are, for example, a general feeling of weakness, tiredness, fatigue, brittle nails and hair.
Rarer causes such as liver damage can sometimes be seen in other symptoms. A feeling of fullness or pressure in the upper abdomen, skin changes, in extreme cases also ascites, but also fatigue and tiredness dominate here.
Still other symptoms are caused by a very rare clinical picture that can also lead to lowered urea levels: a defect in the urea cycle, the breakdown pathway for toxic ammonia. When manifesting in adulthood, there are mainly psychological symptoms, but also vomiting, loss of appetite and states of confusion, including coma. In infants, such a defect is usually even more serious. They act lethargic, barely drink, and develop seizures that can even lead to death. Since the symptoms are so diverse and unspecific, a lowered urea level in the blood is mostly discovered by chance.
Which diseases lead to a lowered urea level?
As already mentioned, in addition to rather harmless and common causes, there are also rare but more serious reasons for a too low urea level in the blood.
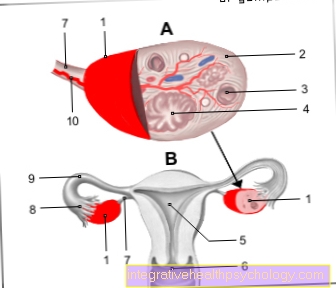
The most common cause is a protein deficiency, which can arise, for example, from special low-protein diets or malnutrition. These are mostly harmless conditions that are easy to fix. In addition, athletes, pregnant women and children have an increased need for protein, which is also reflected in a reduced urea value.
Less common causes are liver damage, such as can result from alcohol abuse or viral hepatitis. In the later stages of the disease, the liver can no longer convert the ammonia produced during protein breakdown into urea as well. A defect in one or more enzymes of the urea cycle, the breakdown pathway for ammonia, has similar effects. Here, too, it is not possible for the body to convert ammonia into urea. So the urea level remains low.
Also read our topic: Malnutrition
diagnosis
The determination of a lowered urea value is mostly done by chance during the blood test and does not initially result in any further tests in healthy adults. If one of the more serious causes of this degradation is suspected, further examinations can be carried out.
For example, if liver damage is suspected, an ultrasound image of the liver is made and the patient is asked precisely about the possible origin of the damage. A test for hepatitis (inflammation of the liver) can also be done. If there is a suspicion of a defect in the urea cycle, questioning the patient is also very important here. In addition, other blood values (e.g. the ammonia value) are collected.
also read: Elevated liver values
therapy
The therapy of a lowered urea value depends on the underlying cause.
The most common cause, insufficient protein intake, usually does not require any special therapy. The only thing to watch out for is a protein-rich diet. In addition to fish, pulses and nuts are particularly suitable for this. If there is already malnutrition, it must be ensured that, in addition to proteins, other important nutritional components are also present in sufficient quantities. In doing so, vitamins and trace elements such as iron and magnesium should be taken into account.
The therapy of more serious causes of a lowered urea value is individually tailored to the respective clinical picture. Here the disease is primarily treated and not the lowered value. This increases by itself when the therapy is successful.
This is how I eat properly when I'm low on urea
As long as the cause of the low urea is an unbalanced or even malnutrition, it makes sense to change your diet.
The low-protein diet is the most common reason for low urea levels. Accordingly, particular attention should be paid to an adequate protein intake. Animal foods that are particularly rich in protein: chicken breasts, lean beef, fish, quark and cheese (e.g. parmesan). The following plant-based foods are particularly suitable for vegans and vegetarians: chickpeas, lentils, almonds, soybeans and oatmeal.
Read more about this under: Foods containing protein
What can the long-term consequences be?
Since the causes of a reduced urea value are very different, it is not possible to name any specific consequences of a value that has been reduced over a long period of time.
Consequences do not occur because of the reduced value but on the basis of the underlying disease. The most common cause, the low-protein diet or malnutrition, can lead to a breakdown of the muscles. There is also a persistent feeling of weakness or constant fatigue. In extreme cases, the breakdown of the muscles can also affect the heart muscle, which results in reduced cardiac output.
What is the urea to creatinine quotient?
The urea-creatinine quotient is a measure of protein metabolism. The values of urea and creatinine in the blood serum are measured and the value for urea is divided by that for creatinine. A quotient is obtained.
A reduced quotient usually indicates a lack of protein intake or, in more rare cases, liver damage. Diseases associated with increased protein breakdown lead to increased values for the quotient. These include, for example, a massive breakdown of red blood cells (hemolysis) or a serious accident. Therapy with cortisone and similar drugs (glucocorticoids) can also lead to an increase.
This topic may still be of interest to you: Hemolytic anemia




.jpg)