Heart attack
synonym
Medical: Myocardial infarction
Definition of myocardial infarction
Heart attack (myocardial infarction) is defined as the destruction of heart muscle cells due to an oxygen deficiency (ischemia) of the heart or a circumscribed region of the heart. In technical jargon, this is also known as ischemic myocardial necrosis. The heart muscle cells are no longer (sufficiently) supplied with oxygen and nutrients, which is why they die (cell necrosis) and are converted into connective tissue cells that can no longer perform any cardiac activity. This creates a scar on the heart.

Most heart attacks take place on the basis of coronary heart disease (CHD), which is mainly caused by a narrowing of the blood vessels (atherosclerosis) of the coronary arteries. In a healthy (physiological) state, the coronary vessels supply the heart muscle cells with oxygen and nutrients. If these vessels are affected by atherosclerosis and are narrowed or even blocked by deposits on the vessel walls, the cells receive an insufficient amount of oxygen and die. This leads i.a. excessive pain and a feeling of weakness in the patient.
The World Health Organization (WHO) speaks of a heart attack when there are markers of unstable angina pectoris in the blood that show damage to the heart muscle. Angina pectoris means chest pain ("tightness of the chest") as a result of a critical coronary artery constriction, which occurs at rest and whose duration, severity and frequency are increasing.
The heart muscle proteins troponin I and troponin T have established themselves as sensitive markers for cardiac muscle damage: they are released into the bloodstream when the cells die and their increased concentration can be determined by taking a blood sample.
Heart attack, together with CHD, is referred to as acute coronary syndrome because the symptoms (symptoms) of these two diseases are very similar and the unstable angina pectoris is often followed by a heart attack.
In addition, an EKG change and the angiographic findings are sensitive markers of a heart attack.
A comprehensive designation and a common diagnostic and therapeutic approach was therefore found.
Occurrence / frequency
Heart attack is the leading cause of death for the population in industrial nations. Die annually in Germany about 200,000 people on one Heart attack. Men have a risk of about 30% of suffering a heart attack in their life, for women in Germany this risk is about 15%.
Cause of the heart attack
Heart attacks arise in over 95% of cases due to coronary heart disease: The walls of the coronary arteries are damaged by atherosclerosis, as so-called plaques attach to the vessel walls. If these deposits tear off the vessel wall, it is injured and a blood clot (thrombus) closes the tear-off site. This wound closure constricts the vascular cross-section or completely relocates it, which results in a reduced blood flow to the downstream organ, the heart.
The main risk factors for the occurrence of atherosclerosis of the coronary arteries and a subsequent heart attack are:
- To smoke cigarettes
- High blood pressure (arterial hypertension)
- high total cholesterol in the blood
- a low level of HDL cholesterol, which has a protective effect on the vascular condition
- a high level of lipoprotein-a in the blood
- Age (men over 45 years and women over 55 years have an increased risk of heart attack)
- a diabetes mellitus and
- the occurrence of CHD and / or heart attacks in first-degree relatives
to call.
Other risk factors for a CHD or a myocardial infarction are
- Overweight (obesity)
- physical inactivity
- wrong diet
- Lipid metabolism disorders
- Glucose tolerance disorder with increased blood sugar levels and
- Tendency to thrombosis (vascular occlusion tendency)
Also read our topic: Heart attack risk, atheromatosis
Much rarer causes of a myocardial infarction (less than 5% of cases) are vascular inflammation (vasculitis), embolism (thrombi carried into the bloodstream), (congenital) vascular malformations that have existed since birth and vascular spasms that can be caused by medication.
Factors that can be partly responsible for the occurrence of a heart attack are, in addition to physical exertion and emotional stress, the time of day and the pre-existence of unstable angina pectoris. If the patient already had angina pectoris complaints in the medical history, i.e. a tightness in the chest, sometimes with shortness of breath (dyspnea) and reduced performance, his heart attack risk is 20%.
The frequency (incidence) of a heart attack is increased in the early morning hours, as the blood tends to form thrombi (vascular occlusion) more at this time.
In 70% of cases, the left half of the heart is affected by an infarct. It is bigger and stronger than the right half and therefore needs more oxygen. The myocardial infarction is further classified into transmural and
non-transmural infarction.
In transmural myocardial infarction, more than 50% of the wall thickness of the myocardium is affected by cell death and is associated with visible changes in the echocardiogram (ECG); in non-transmural myocardial infarction, the cell damage is limited to the inner layer of the heart wall and there is no correlate in the ECG.
The portion of myocardium that becomes functionless due to an infarction depends on the location of the vascular occlusion. If the constriction or the occlusion of the vessel is due to the vascular stem, large areas of the heart muscle are undersupplied and an extensive infarct zone with a high loss of function results.
The longer the ischemia time (time in which the heart muscle is insufficiently supplied with oxygen), the more pronounced the process of cell death and the more serious the impairment of cardiac output.
Read more on the subject at: Causes of a heart attack
What role does blood pressure play in a heart attack?
Arterial hypertension (high blood pressure) is a widespread disease in the population of industrialized nations. The high blood pressure can cause turbulence within the vessels. This favors the deposition of various substances on the vessel wall. The deposits lead to more turbulence occurring and even more substances to be deposited. In a sense, there is a vicious circle, because the substances constrict the blood vessels and in turn lead to higher blood pressure values, which gradually put more and more stress on the heart. These deposits are particularly dangerous with regard to a heart attack if they occur in the coronary arteries. These vessels are responsible for supplying the heart muscles with oxygen and other nutrients. A constriction can mean that, over time, too little blood with nutrients reaches the heart muscle cells. This results in damage up to and including the death of the cells that lead to a heart attack. Blood pressure can also provide important information in the case of an acute heart attack. The heart can be so badly damaged by the infarct that it no longer has enough strength to maintain blood pressure. A sharp drop in blood pressure (often accompanied by dizziness or fainting spells) can therefore be a sign of a heart attack.
Heart attack from stress?
It has long been known that prolonged stress can be detrimental to the cardiovascular system. There are several mechanisms behind this. On the one hand, chronic stress increases blood pressure and pulse over time. High blood pressure values in particular increase the risk of suffering a heart attack.
In addition, the body produces more white blood cells during stress. In stressful situations, these are primarily intended to help the immune system to defend itself against foreign substances. The white blood cells do not only have positive effects on the body. Especially in people who already suffer from atherosclerosis (calcification of the vessels), these blood cells tend to form additional plaques and deposits inside the vessels and thus lead to additional narrowing.
Heart attack risk - how can you assess it yourself?
Your personal heart attack risk should primarily be assessed by your doctor or cardiologist (heart specialist). Nevertheless, there is the possibility of doing your own risk calculation, especially on the Internet.
The different websites calculate the risk based on different data. This includes your own age, because the older someone gets, the higher the risk of suffering a heart attack. Blood pressure also plays a major role. The higher the blood pressure, the more likely a heart attack becomes. Gender is also an important factor in risk assessment, because men have a higher risk of heart attacks than women, especially when they are younger. Blood fat levels also play an important role. HDL and LDL (both are cholesterol levels) are important parameters. A high HDL value has a positive effect on the cardiovascular system, high LDL has negative effects. In addition, diabetes and active smoking increase the risk of a heart attack. Most computers also ask for family history (i.e. whether a relative has already had a heart attack), since heart diseases often also have a genetic component.
Harbingers
A heart attack usually comes as a surprise, but in most cases an acute heart attack is preceded by the first signs of a heart attack, which, however, are not perceived as such.
Heralds of a heart attack are, for example, unspecific abdominal pain, nausea, sleep disorders, tiredness or dizziness. These symptoms can occur many weeks before the actual heart attack, but are often misjudged.
A typical sign of a heart attack is a feeling of pressure or tightness in the chest, which is usually associated with physical exertion (e.g. Climb stairs) occurs. Pain in the left arm as a sign of a heart attack is also not uncommon.
This uncomfortable feeling in the chest, which is also called a tight and pressing chest pain or even a "Annihilation pain"is described as angina pectoris. Typically, an attack of angina pectoris lasts anywhere from a few seconds to a few minutes. If the attacks are more frequent, more intense or the chest pain lasts longer (15 is over 30 minutes) this is characteristic of a heart attack.
But not all pressure in the chest has to come from the heart. Pressure in the chest can also be caused by the lungs or esophagus. You can read more about this under: Chest pressure- what to do
But not everyone feels the symptoms that are triggered by a heart attack in the same way. Some heart attacks cause no, only minor or atypical symptoms (so-called "silent heart attack"). These silent heart attacks occur more frequently in people with diabetes and are only rarely announced by unspecific symptoms.
The harbingers of a heart attack are often different alarm signs in women than in men. Symptoms that indicate a heart attack in women include, for example, severe shortness of breath, recurring nausea, vomiting and, in particular, upper abdominal discomfort. These complaints are often misinterpreted as stomach problems.
The so-called NAN rule can help in recognizing heart attack symptoms in women: If inexplicable pain occurs in the body area between the nose, arm and navel that lasts longer than 15 minutes, an emergency doctor should be called in any case, as this is a sign for you Heart attack.
An increase in blood pressure can also be a harbinger of a heart attack, especially if typical symptoms such as chest pain, shortness of breath or blurred vision occur at the same time. The affected person often experiences cold sweats and has cold and clammy hands.
The slightest indication of a heart attack must be taken seriously, regardless of the type of complaint, as sudden cardiac arrest can occur at any time without further notice.
Read more on the subject at: Signs of a heart attack
Complaints / symptoms
Only about forty percent of those with a heart attack show typical symptoms.
The main symptom, the most frequently occurring symptom, of the heart attack is the chest pain (unstable angina pectoris, also called "tightness of the chest"). This is very pronounced, is usually described as lying behind the breastbone and has a "devastating" character for many patients.
Read more on the topic: Pain in the region of the heart
Compared to the stable angina pectoris attack (moderate lack of oxygen in the heart muscle cells), the unstable angina pain during a heart attack does not improve with the administration of nitro preparations (drugs that stimulate blood circulation in the heart). In addition, it lasts longer (over 20 minutes) and does not subside when the body is at rest, so that patients are often scared to death.
The pain usually radiates into the arms (more often on the left), the upper abdomen or lower jaw and the shoulder joint and occurs in more than half of the patients before a heart attack occurs.
Women, diabetics and elderly patients often report upper abdominal complaints when they have a heart attack, so that such pain must not only be thought of a cause in the stomach and intestines, but also of a back wall infarction as the trigger for the pain.
In addition to the main symptom of angina pectoris, many patients experience a feeling of weakness, they sweat more, are pale, have cardiac arrhythmias and suffer from shortness of breath, as well as nausea and vomiting.
Read more on the subject at: Symptoms of a heart attack
20-30% of patients have a so-called "silent" heart attack, i.e. it does not cause pain in the patient. This is often the case with diabetics (diabetes mellitus) or very old patients who have a nerve change (neuropathy) and can hardly or no longer feel pain. In the event of a heart attack, these patients primarily suffer from shortness of breath, physical weakness, or pass out and suddenly lose consciousness. The heart attack is the first clinical appearance (first manifestation) of the coronary artery disease in these patients.
95% of the patients have cardiac arrhythmias during the infarction, which can extend to ventricular fibrillation (ventricular tachycardia). The heart's actions are so fast that no more blood is transported. Ultimately, this means the same as cardiac arrest (asystole) without any cardiac action by the muscle cells.
Shortness of breath or rattling noises detected with a stethoscope when listening to the lungs are signs of left heart failure (left heart failure), i.e. a weakened and inadequate function of the left half of the heart, which can be seen in about 1/3 of the patients. In the course of the left heart weakness it comes to the lung congestion with the typical wet rattling noises.
At the cellular level, the symptoms are based on the following reasons:
The under-supplied and dying heart muscle cells lose their function in the event of a heart attack. They can no longer contribute to the pumping function of the heart, which maintains blood pressure and blood flow in the circulatory system. As a result, signs of illness (symptoms) such as a drop in blood pressure, shortness of breath due to the restricted blood circulation and oxygen supply to the organs, mainly due to the undersupply of the brain, as well as a feeling of physical weakness.
In short, it can be said that the picture of a heart attack is very variable. From an unimpaired patient to an unconscious patient, anything is possible. A typical overall impression is a pale, anxious, painful patient who is cold sweaty and may vomit.
also read: Sternum pain.
Left arm pain
Pain radiating from the chest to the left arm can be symptoms of a heart attack. In women in particular, isolated pain in the left arm can occur, which is initially independent of pain in the heart region.The pain basically arises from the fact that the heart muscle cells are not adequately supplied with oxygen and other nutrients. This is often the case when the vessels that supply blood to the heart become blocked. The lack of blood circulation leads to the destruction of the heart muscle cells, which often causes very severe pain, which can also be presented as burning or stinging. The fact that the pain is not limited to the heart region is due to the interconnection of the nerve cells that direct the pain stimulus to the brain. Pain fibers from the heart and left arm are brought together at one point and continue from there into the brain. Because of the common end route, the brain sometimes cannot tell where exactly the pain is coming from. That is why the brain projects the feeling not only onto the heart, but also onto the left arm.
Read more on the topic: Left arm pain as a sign of a heart attack?
Back pain from a heart attack
Sometimes the sharp pain of a heart attack isn't felt right in the chest. Instead of causing pain in the heart, the heart attack can also lead to back pain, which is particularly common between the shoulder blades. The fact that the pain in the back is perceived is due to the interconnection of the pain-conducting nerve fibers. The pain fibers from the back and those from the heart area are routed together on a nerve plexus to the next nerve fiber and are therefore bundled at the brain. The brain can therefore often no longer “calculate” the region from which the pain actually comes and therefore interprets the pain of the heart attack as back pain.
Symptoms of a heart attack in women
The typical symptom of a heart attack, namely the strong stabbing pain or the feeling of pressure in the heart area, can also be found in women, but heart attacks in women often make themselves felt as very unspecific signs. The heart attack in women often presents with pain in the stomach area. This can be accompanied by nausea and vomiting, and in some cases diarrhea. Furthermore, women are more likely to show signs such as shortness of breath and shortness of breath. This often also includes a general poor performance and increased tiredness. In addition to chest pain, women often feel a stinging in the left arm or one that extends into the back to between the shoulder blades. Pain in the area of the neck to the jaw can also indicate a heart attack in women. Likewise, dizziness and fainting attacks are not atypical signs in women. Overall, heart attacks occur more frequently in women from the age of 50. In diseases that favor heart attacks, these can also occur at a young age.
Read more on the subject under: Heart Attack in Women
Symptoms of a heart attack in men
In men, the heart attack usually proceeds according to the "typical" scheme. There is a sudden sharp pain in the heart. Often there is a feeling of tightness and pressure on the chest. The sudden appearance in combination with the strong feeling of tightness can lead to symptoms of anxiety up to fear of death. Even before the heart attack, signs such as a decline in performance and reduced physical resilience can appear. Likewise, if you are short of breath and become increasingly tired, you should consider a possible subsequent heart attack. Heart attacks are most common in men between 65 and 75 years of age. However, the risk of suffering a heart attack is already increased from the age of 40. If there are diseases that favor a heart attack, more attention should be paid to a possible impending heart attack even at a young age. These disorders include disorders of the blood lipid balance. High blood pressure or atherosclerosis (calcification of the vessels) can also be involved in the development of a heart attack. The same applies to diseases such as diabetes mellitus (“diabetes”).
How long is the duration of the symptoms?
There are several non-specific symptoms that can herald a heart attack well in advance. These include, for example, increased fatigue, reduced performance and reduced resilience. These are the first signs that the heart is no longer performing as well. The underlying problem can be blocked coronary arteries, which are also involved in the development of heart attacks. Sharp pains can also occur long before the actual infarction, because these are also caused by an insufficient supply of the heart muscle cells. This pain can occur particularly during physical exertion. Some people have had these symptoms for months without having a heart attack.
The actual symptoms of a heart attack should be taken seriously after just a few minutes. Depending on the severity of the heart attack, they can last longer than half an hour. However, an emergency doctor should have arrived by then at the latest, provide first aid and relieve the symptoms with medication.
Can you have a heart attack without realizing it?
There is a possibility of having a heart attack without even realizing it. This type of heart attack is also called "silent heart attack" because its typical "symptom" is lack of symptoms. Above all, the sharp pain or tightness that usually occurs suddenly is not perceived during a silent heart attack. Early warning signs such as tiredness, poor performance, reduced resilience or nausea and vomiting can occur days or weeks beforehand. However, these signs do not immediately suggest a heart attack. A silent heart attack occurs particularly when the pain-conducting nerves are damaged in any way. In this case, the resulting pain cannot be passed on to the brain. So this is not felt either.
A typical illness in which silent heart attacks occur more often is diabetes mellitus (“sugar disease”). The increased sugar levels firstly increase the risk of a heart attack and secondly, nerve damage occurs, so that pain transmission from the heart to the brain is not always available. Other neurodegenerative diseases, i.e. diseases in which nerve fibers perish, can also be the cause of the lack of symptoms in a heart attack.
Read more on the subject at: Silent heart attack
Course of the heart attack

The heart attack is divided into the following pathological changes in the heart muscle:
- Phase of early undersupply of the heart muscle
The cells receive less energy than they need for their function, the heart contraction (contraction of the heart to carry the blood into the body). The contraction force of the heart decreases. - Phase of cell death
The insufficient supply of the cells leads to their death. - Phase of scarring
The myocardium (muscle cells) begins a remodeling of the left ventricle in the early phase of the heart attack, which is known as remodeling.
The wall thickness of the heart muscle decreases at the infarct site, so that the heart chamber expands here and changes its original shape as a whole. Due to the breakdown of the muscle cells, the wall tension of the heart increases, which increases the expansion of the heart chamber. At the same time, the oxygen consumption of the still intact heart muscle tissue increases.
Complications
The complications after a heart attack are manifold and almost always depend on how quickly the affected person is treated after the heart attack. A heart attack often leads to a pumping weakness (insufficiency) of the heart. If the heart attack is particularly severe, the affected person can remain in a coma for a long time. Many medications are administered, and the person is ventilated. This creates complications such as infections that can lead to pneumonia. In addition, a long rehabilitation period must be expected. Furthermore, complications such as decreased performance, decreased resilience, fatigue, etc. can occur.
The complications are divided into early and late complications.
The first include all events that occur in the first 48 hours. It is the most dangerous period, 40% do not survive the first day after a heart attack. One of the early complications is left heart failure, in which up to 20% of the left ventricle is affected by the infarct and dies. If more than 40% are affected, this usually results in a cardiogenic (heart-related) shock, which is 90% fatal. This leads to a drop in blood pressure and failure of the heart to pump. Cardiac arrhythmias are another complication. These include additional ventricular contractions that increase the risk of ventricular fibrillation. Ventricular fibrillation often occurs within four hours of the myocardial infarction and is fatal in 80% of patients.
The late complications include:
- arterial emboli
- Pericarditis
- Heart wall aneurysm (bulges in the heart wall)
- Heart failure
- Arrhythmias
Duration of a heart attack
Since a heart attack plays out differently for every person, the exact duration cannot be predicted. Signs such as nausea and vomiting, which are very unspecific symptoms, can appear weeks or days before a heart attack. However, it cannot be used to determine when the heart attack occurs. If symptoms, such as chest pain and tightness in the chest, persist for more than 5 minutes, a heart attack is a likely diagnosis and an emergency doctor should be called immediately if such symptoms occur. It is entirely possible that the symptoms persist for more than 30 minutes if the person is not properly cared for in the meantime.
Diagnosis

laboratory
When the blood is taken, the inflammation values are always determined, which show an increased reactive protein C and possibly increased white blood cells. In addition, the sedimentation rate is increased. However, these inflammation values are very unspecific and do not necessarily indicate a myocardial infarction. Another non-specific marker is LDH, an enzyme called lactate dehydrogenase that is used for late diagnosis. It only returns to normal after a week or two.
More specific markers of a HI are troponin T and I. They are heart muscle-specific markers that rise about three hours after the infarction, reach their maximum after 20 hours and only return to normal after one to two weeks. They are considered very safe when measured over a period of 10 hours and 5 days. On the fourth day, the troponin T correlates with the size of the infarct.
Unfortunately, positive troponin levels can also occur in cases of pulmonary embolism, heart muscle inflammation, acute and chronic heart muscle weakness, kidney failure or a stroke.
The enzyme creatine kinase can also be determined. It is the lead enzyme that increases when there is muscle or cardiac damage. Here, too, the level of creatine kinase and the size of the myocardial infarction correlate with one another. There are four subgroups of the enzyme. Creatine kinase MB stands for the myocardial type and is important for the diagnosis of a heart attack. If this increases between 6-20% of the total creatine kinase, this speaks for a release from the heart muscle. The reason can be a heart attack, but inflammation of the heart muscle or an operation on the heart can also be the cause.
There is a quick test for a protein called "heart fatty acid binding protein" (German: heart-typical fatty acid binding protein). This is already positive 30 minutes after a heart attack has occurred.
EKG
The electrocardiogram is an important diagnostic tool to better visualize myocardial infarction. It shows the sum of the electrical activity of all heart muscle fibers. It can often be negative in the first 24 hours after the heart attack-like symptoms. A second ECG must therefore be performed after 24 hours to confirm or rule out a myocardial infarction if necessary.
An infarction can only be excluded if the ECG is negative twice and no troponin T or troponin I or creatine kinase MB abnormalities are present.
The EKG can be used to describe the extent and location of the infarction and to determine the age of the myocardial infarction. The typical sign of a heart attack is the so-called ST elevation. There are several waves in the EKG. The area between S and T is the distance in which the excitation of the chamber recedes and the heart muscle relaxes again. Elevation in this area increases an oxygen deficiency, is indicative of an infarction and is also referred to as STEMI (ST-segment elevation myocardial infarction = ST-segment elevation myocardial infarction). There are three stages, each with their typical EKG changes, which show the age of the infarction. In addition to the STEMI, there is an NSTEMI, a non-ST elevation myocardial infarction. There is more likely to be a lowering of the ST segment. The typical laboratory with troponin T / I and the enzyme increase in creatine kinase MB are proof here. With the EKG, several leads are made along the heart. In this way, the doctor can also tell where the infarction is, because precisely these leads then look suspicious.
Imaging procedures
With echocardiography, like an ultrasound, the heart and its structures can be displayed. The valves, the vessels and the size are clearly visible to the trained examiner. The entire heart function can be assessed from the atrium to the chamber filling to the pump function. A missing increase in thickness of the infarct zone and a regional wall movement disorder are recognizable. In a very fresh infarct, such wall movement disorders occur very early, even before the EKG changes and the enzyme increases. If there are no wall movement disorders, a myocardial infarction can be ruled out 95% of the time.
Magnetic resonance imaging can also show structural changes in the heart. However, the gold standard of imaging is left heart catheterization. The examination takes place under sterile conditions. The patient lies on the examination table and receives a local anesthetic at the puncture site. This is either in the groin on the femoral artery or on the wrist on the radial artery. A catheter (wire) is then advanced to the heart. The catheter is used to fill the left ventricle with contrast medium. At the same time, X-ray images are made, which are transmitted to a monitor. Any constrictions or occlusions in the coronary arteries can thus be clearly displayed.
Read more on the subject at: Diagnosis of a heart attack
Illustration heart attack
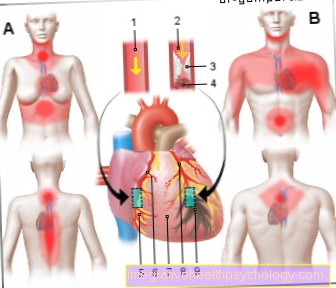
Heart attack (HI)
Myocardial infarction (MI)
- Healthy coronary artery
(Coronary artery)
Coronary artery - Occluded artery
Atherosclerotic plaque
with blood clot (Thrombus) - Fat deposits (plaque)
- Blood clot -
thrombus - Healthy muscle tissue
- Coronary artery right -
Coronary artery dextra - Pericardium -
Pericardium - Left coronary artery -
Left coronary artery - Destroyed muscle tissue
(Infarct area with cell death)
Typical areas of pain in a heart attack:
Woman - chest, upper abdomen, neck,
Lower jaw, spine, back,
NAN rule (nose - arm - navel)
Man - chest, stomach,
Emanation in the arm and shoulder,
Lower jaw, back
An overview of allhe images by Dr-Gumpert can be found at: medical illustrations
What tests / rapid tests are there for a heart attack?
In order to correctly diagnose a heart attack, the anamnesis, i.e. questioning the patient, plays an important role. If the suspicion of a heart attack is confirmed, blood tests are mainly used. This involves testing various substances in the blood that are normally found within the heart muscle cells. Because in a heart attack, the cells break and pour their ingredients into the blood so that they can be detected there. A substance that generally indicates the death of cells is LDH. LDH is found in almost all cells and is involved in their metabolism. The typical marker for the presence of a heart attack is troponin T.Troponin T is an enzyme that is only found in heart muscle cells. So if there is too much of it in the blood, it clearly indicates damage to the heart. In addition to the blood tests, an EKG will be consulted. The electrical activity in the heart is recorded by means of electrodes. These are recorded as waves and peaks. If these deviate from the typical pattern, a heart attack is suspected. Most often the change is that the distance between the S wave and the T wave is higher. One therefore speaks of an ST elevation infarction.
Treatment of myocardial infarction

According to the guidelines, the treatment of a heart attack should be in the following order:
- General measures (securing life)
- Reperfusion therapy (reopening of occluded coronary arteries)
- Coronary re-thrombosis prophylaxis
- Therapy of complications
The emergency doctors are usually the first to see a heart attack patient. You immediately give oxygen and a nitro (a drug used to improve blood flow to the heart) is sprayed under the tongue. Anticoagulants and acetylsalicylic acid are given through a venous line. One study showed that early administration of acetylsalicylic acid (aspirin) reduces the risk of death by 20%.
Furthermore, the patients receive beta blockers, provided they have no contraindications such as low heart rhythm, asthma, heart failure, age> 70 years or conduction disorders in the heart. These lower the resting heart rate and blood pressure. This reduces the risk of developing ventricular fibrillation.
As soon as the affected person arrives at the hospital, the circulatory system is closely monitored. If the pain is severe, nitrates or morphine (a potent opiate) can be given if the pain is severe. The acetylsalicylic acid medication (ASA) is continued and additional anticoagulants are administered. The beta blockers are also retained as medicinal products if there is no contraindication.
There are two possible approaches to reperfusion therapy. In the conservative, so-called fibrinolytics are given, which split and thus dissolve the blood clot that closes the coronary artery. These drugs include:
- Streptokinase
- Alteplase (r-t-PA) or
- Reteplase (r-PA)
They may only be used if the heart attack was not more than 6 hours ago, there are no contraindications and a confirmed ECG change has been determined.
Contraindications that speak against lysis therapy (dissolving the thrombus by means of special drugs) are:
- Stomach and intestinal ulcer (ulcer)
- Fundus bleeding
- a headache
- History of bleeding disorders
- pregnancy
- a stroke less than 6 months ago (apoplexy)
- Aneurysms (abnormal bulging of the blood vessels)
- an operation less than 1-2 weeks prior or an accident
The second method is an operational approach. During the left heart catheter examination, a "percutaneous transluminal coronary angioplasty" carried out. It is the gold standard of heart attack therapy. In this procedure, a guide catheter (small tube) is inserted either through the inguinal artery (femoral artery) or the forearm artery (radial artery) and advanced to the aortic valve and coronary arteries. A balloon catheter is inserted through this. An attempt is made to reopen the constricted or closed vessel in the heart by means of the balloon, which can be expanded manually. A stent, a small net-like, cylinder-shaped vessel, can be used as additional support.
Nowadays, as long-term therapy, anticoagulants and beta blockers are prescribed permanently. The anticoagulants include, on the one hand, those that directly inhibit platelet clumping (acetylsalicylic acid or clopidogrel) and, on the other hand, the coumarins, which indirectly prevent blood clotting via vitamin K. In addition, the patient should take cholesterol-lowering drugs, as they clearly lower the second infarction rate and the mortality rate.
Read more on the subject at: Therapy of a heart attack
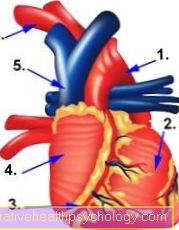
Figure anatomy heart
- Main artery (aorta)
- ventricle
- Coronary arteries
- Forecourt (atrium)
- Vena cava
- Carotid artery
What does first aid look like in a heart attack?
When caring for a heart attack, there are two goals that the first aider should pursue: The main thing is to relieve the heart. In addition, the patient's complaints should of course be alleviated as successfully as possible.
Since the circulation often collapses in a heart attack, it can lead to fainting spells. Therefore, the patient should be laid down. Ideally, the upper body should be raised a little. This means that less blood flows back to the heart, so that the heart can save some energy. People who have been known to have heart problems for a long time often have a nitro spray. There is a substance in it that can expand the vessels. Since the constriction in the coronary arteries is the cause of the heart attack in most cases, the drug is ideally suited to widen the arteries again in an emergency.
Of course, if a heart attack is suspected, the emergency doctor should be called immediately. The paramedics can then provide further help. For example, they provide the person with oxygen. They can also give painkillers to relieve the acute symptoms.
Read more on the topic: First aid
Stent after a heart attack
In most cases, a heart attack occurs when one or more of the coronary arteries is blocked. This means that enough blood can no longer flow into the tissue behind the constriction. This leads to an insufficient supply of oxygen and other nutrients. As a result, the heart cells die, which can lead to irregularities in the heart's pumping action. In order to restore the supply of the heart muscle cells, the constriction or blockage must be overcome. This is often possible with a stent.
A stent can be thought of as a round wire mesh. Usually the stent is brought into the coronary artery with a catheter. So a long wire is pushed from the artery on the thigh or forearm to the heart, from where the catheter goes into the coronary arteries. The stent is placed in the coronary artery in such a way that it rests all around the vessel wall and henceforth keeps the vessel open. In order to prevent the obstructing material from being deposited again, the stent is often additionally coated with certain substances. In this way, the affected coronary artery can be kept open for a long time, which prevents new heart attacks.
Read more on the subject at: Implantation of a stent after a heart attack
Bypass after a heart attack
A heart attack is often caused by a blockage or narrowing of the coronary arteries. Because the vessel has a narrow point, the tissue behind it is no longer adequately supplied with blood. The obvious therapy is therefore to restore the blood supply to the cells. One way to do this is through bypass surgery. Usually an endogenous vessel from another region of the body is used to bridge the constriction. This vessel is connected to the main artery and connected to the coronary artery behind the constriction. This allows the blood to flow past the narrow point and supply the heart muscle cells again.
Figure heart valves
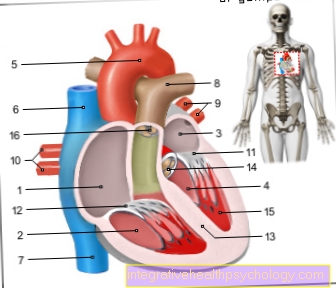
- Right atrial -
Atrium dextrum - Right ventricle -
Ventriculus dexter - Left atrium -
Atrium sinistrum - Left ventricle -
Ventriculus sinister - Aortic arch - Arcus aortae
- Superior vena cava -
Superior vena cava - Lower vena cava -
Inferior vena cava - Pulmonary artery trunk -
Pulmonary trunk - Left pulmonary veins -
Venae pulmonales sinastrae - Right pulmonary veins -
Venae pulmonales dextrae - Mitral valve - Valva mitralis
- Tricuspid valve -
Tricuspid valva - Chamber partition -
Interventricular septum - Aortic valve - Valva aortae
- Papillary muscle -
Papillary muscle
You can find an overview of all Dr-Gumpert images at: medical illustrations
After a heart attack in an artificial coma
People who suffer a very serious heart attack are often put into an artificial coma. As a result, the body uses less energy so that the heart can recover better. The people are artificially ventilated, and they also have various accesses (mostly connections to the veins) through which medication can be administered. These drugs are supposed to support the heart and the circulatory system, as long as the heart is not able to do this on its own. However, the artificial coma also has disadvantages. The body functions run “on the back burner” for a while, so after waking up, people have to get used to everyday stresses again.
forecast

Unfortunately, a large number (almost 40%) still die on the first day after a heart attack. Without revascularization in the hospital, another 15% die. This increases the risk of dying from a heart attack to around 50% within the first month.
In the first two years after discharge, 5-10% of all those affected suffer sudden cardiac death.
The long-term prognosis depends on several factors. On the one hand, on the size of the infarct area and the signs of ischemia (chest tightness and EKG signs) and, on the other hand, on the cardiac arrhythmia and the number of vessels involved.
The persistence of risk factors is also an important factor.
- LDL cholesterol increase
- high blood pressure
- Smoke
- Diabetes mellitus
- Age (over 45 years for men and over 55 years for women)
If possible, the above risk factors need to be brought under control to improve the prognosis a little.
Read more on the subject at: Heart attack prognosis
Arrhythmias after a heart attack
A heart attack occurs when heart muscle cells do not receive enough blood and other nutrients. This is often the case when the coronary arteries are blocked. Heart muscle cells die off due to the insufficient supply. The signal that stimulates the heart muscle cells to contract is passed on from cell to cell and via fine nerve bundles. The cell death can result in interruptions in this stimulus transmission. As a result, the heart is no longer beating in a coordinated manner. The rhythm gets mixed up. These cardiac arrhythmias can persist even after the acute infarct situation. However, they can be treated with medication.
What are the chances of survival after a heart attack?
About half of the people who suffer a heart attack die in the acute situation. Mostly this is due to the cardiac arrhythmias that are triggered by the infarct and cannot be corrected quickly enough. For long-term survival after a heart attack, the first 2 hours after the heart attack are particularly crucial. The faster the affected person is treated and the faster the constriction in the coronary arteries is expanded again, the better the prognosis. In addition, survival is of course dependent on the size of the affected area and thus on the subsequent complications. About 5 to 10% die of sudden cardiac death in the first 2 years after a heart attack. The rate of new heart attacks is also high.
prevention
How can you prevent a heart attack now? A healthy lifestyle is the most important thing. Smoking is linked to a three-fold increased risk of heart attack. It should be finished as soon as possible. A healthy so-called “Mediterranean” diet makes sense. Little animal fat and meat should be eaten. Vegetable oils and plenty of vegetables and fruits should be consumed. Exercising regularly can lower the risk of myocardial infarction. Anyone suffering from risk factors such as diabetes mellitus or high blood pressure should keep the values in the normal range under strict control.
Read more on the topic: How can you prevent a heart attack?
rehabilitation
Rehabilitation, or rehabilitation for short, is intended to help people with heart disease to regain physical and mental health as much as possible and to return to everyday life.
There are four areas of heart rehab.
- Somatic (physical): An individually designed training measure should help those affected to become productive and resilient again.
- Educational: A healthy lifestyle should be acquired. In addition, the medication is discussed. Why this is important and the consequences of not taking the medication. So those affected are more sensitive and take them more regularly.
- Emotional: Heart attack patients often suffer from psychological problems such as depression or anxiety. Trained staff is on site and can support those affected.
- Social: A supervisor helps the patient get back into everyday life. Tips and information on various areas such as air travel, driving a car, job, sexuality are given.
The rehab is divided into three phases:
Phase 1 begins in the hospital. Rapid mobilization is sought. Phase 2 takes place either as an inpatient or outpatient in a rehab clinic. The four areas of heart rehab mentioned above are on the program. Phase 3 includes lifelong follow-up care for the infarct patient. The aim is that those affected can lead a normal everyday life again and are only slightly or not at all restricted by the consequences of a heart attack.
Read more on the subject at: Rehabilitation of a heart attack












.jpg)