Inflammation of the testicles
introduction
As testicular inflammation, or orchitis, is the inflammation of the male, paired gonads (Gonads).
A testicular inflammation is almost always accompanied by intense pain, because the testicles are supplied by a strong network of nerves. In the event of swelling or heating, this immediately transmits pain impulses to the body. In this way, the body signals that something is wrong and, if there is no treatment, there is a risk of irreversible loss of function.

causes
The causes of testicular inflammation are mostly due to inflammation of the surrounding structures, since testicular inflammation alone is relatively rare. It is usually the result of epididymitis or a systemic infection. Infections that lead to inflammation of the testicles can be caused by viruses and bacteria. While bacteria usually get to the testes via the ascending urinary tract, viruses in this case tend to spread hematogenously - i.e. via the bloodstream.
Typical viral pathogens that can cause testicular inflammation are the paramyxoviruses, which occur in mumps. Mumps can therefore cause inflammation of the testicles (testicular mumps). Therefore, vaccination in the form of measles-mumps-rubella vaccination is an important preventive measure.
In addition to the paramyxoviruses, varicella can also trigger testicular inflammation. Varicella is better known as the causative agent of chickenpox. It is also a disease typical of childhood, which in itself is relatively uncomplicated. Other viruses that can be responsible for testicular inflammation are echoviruses and coxsackieviruses.
While viral infections tend to be more typical in childhood, bacterial infections occur more frequently in sexually active men. Frequent changing of sexual partners or frequent intercourse increases the chance of becoming infected with bacteria. Accordingly, the spectrum of pathogens also resembles that of urinary tract infections: In addition to Neisseria (Neisseria gonorrhoeae), the pathogen causing gonorrhea, chlamydia and E. coli bacteria are also part of the typical bacterial pathogen spectrum for testicular inflammation. These pathogens are typical of urinary tract infections, but are not necessarily due to poor hygiene, but rather to sexually active behavior.
However, this does not have to be the case, some other pathogens that cause testicular inflammation are relatively unspecific: staphylococci and streptococci are just as much a part of the spectrum of pathogens as pseudomonads and brucellae. These are very widespread pathogens that can also cause infections of the respiratory tract or the skin, for example. Testicular inflammation almost always occurs as a concomitant disease of epididymitis or inflammation of the urinary tract. Due to the anatomical proximity and the close connections among each other, infections quickly spread from one organ to the other.
In the prostate, the two vas deferens open into the urethra. These lead directly to the epididymis, and ultimately to the testicle. Ascending urinary tract infections are therefore responsible for a large part of testicular inflammation.
Read more about this in our main article: What are the causes of testicular inflammation?
Cause mumps
Mumps is a disease caused by the mumps virus that typically affects the salivary glands. As a complication of the infectious disease, inflammation of the testicles can also occur. The viruses are distributed through the blood from the salivary glands and particularly like to settle in the testicles.
While children with a mumps infection are often spared this complication, orchitis after mumps infection affects up to 30% of all men with mumps after puberty. In men with a mumps infection, the testes should therefore be examined as standard.
Read more on the subject at: Testicular mumps
Symptoms of inflammation of the testicles
Due to the anatomical proximity of the testicles, epididymis and the urinary tract, infections usually spread across several organs. The testicle is, so to speak, the end piece, in a chain of urethra, spermatic duct, epididymis and testicles. Only when any bacteria have passed the previous structures do they reach the testes. Accordingly, testicular inflammation is usually associated with epididymitis or urinary tract infections. A singular testicular inflammation is relatively rare.
The symptoms of inflammation are classically: swelling of the testicles, redness, testicular pain and loss of function. The pain can vary from a slight tugging in the testicle to a very violent intensity. Mostly they correlate with the intensity of the inflammation and the number of organs involved. In addition, there may be general symptoms such as chills, fatigue, fever and headache. A mumps infection primarily results in inflammation of the parotid gland and, a few days later, inflammation of the testicle. This process is so specific that it automatically suggests a mumps infection.
In viral infections, both testicles are affected in only 30 percent of cases.In general, sexual intercourse is relatively painful during the infection and should be avoided: In addition to a loss of function of the testicles, there is also the risk of infecting the partner, so that he then also has to struggle with a urinary tract infection or inflammation of the urogenital tract.
You can find out more about this topic here: Symptoms of inflammation of the testicles.
Pain
Pain is the defining symptom of testicular inflammation. Inflammation is typically associated with symptoms of redness, overheating, swelling, and pain. So there is a pain per se from the inflammation.
However, the swelling is also a strong pain trigger, especially on the testicles. The testicle is packed in a tight capsule. If the testicle swells due to the inflammation, this capsule is stretched very quickly, which in turn is a very painful rice.
In addition to adequate cooling and elevation of the affected testicle, the pain can also be treated with painkillers. Preparations such as ibuprofen and paracetamol are particularly suitable because they not only relieve pain, but also have an anti-inflammatory effect.
How contagious is testicular infection?
Inflammation of the testicles can be contagious in many cases. The pathogens are transmitted in different ways.
For example, if you get testicular inflammation due to a mumps infection, the mumps virus can be passed on through the saliva. A droplet infection, for example from coughing, is often sufficient for this. Those who are infected with the mumps virus usually also get an inflammation of their salivary glands. However, the infection does not necessarily lead to an inflammation of the testicles. Here, too, it applies that especially men after puberty are prone to testicular inflammation from mumps, so that a third to a fifth of infected men also suffer from testicular inflammation.
Testicular inflammation caused by sexually transmitted diseases such as gonorrhea or chlamydia is also contagious. However, normally only sexual partners in the person concerned become infected. In heterosexual couples, a man can transfer the bacteria to his partner, which can also cause inflammation of the female genital organs. Conversely, the woman can infect her male partner with the bacteria, whereupon he can develop testicular inflammation. Direct infection with testicular inflammation can occur during homosexual intercourse between two men.
In principle, however, only the pathogen is transmitted from one person to the other. It is not always certain whether the infected man will then also suffer from testicular inflammation, but it does occur frequently. With adequate genital hygiene, infection with chlamydia and gonorrhea should not occur without sexual contact.
diagnosis
Various means are available for diagnosing testicular inflammation: First of all, a doctor-patient conversation - also called anamesis - is important in order to determine the exact symptoms and what happened. A relatively clear diagnosis often results from this conversation. The conversation is usually followed by an assessment of the testicles and a palpation. If the patient reacts excessively painfully to pressure, or if the testicle is already visibly swollen and reddened, these can be indicators of testicular inflammation.
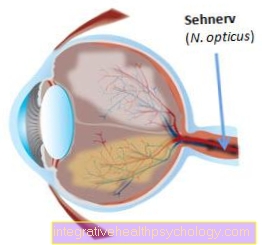
In addition, the doctor is available to diagnose the testicle by means of ultrasound (Sonography) to disposal. The ultrasound can show accumulations of fluid, i.e. edema, as well as swellings, or torsions. Ultrasound is a very cheap, fast and, above all, safe way of examining the patient. If the suspicion of a bacterial infection is confirmed, it is important to determine the exact pathogen.
Antibiotic therapy should always be targeted against a pathogen, and not as a "sweeping blow" with a broad spectrum antibiotic. In some cases this is not possible otherwise or makes sense, but one always tries to target the pathogen in order to keep broader acting antibiotics in hand for possible later diseases. Over time, bacteria develop a resistance to frequently used antibiotics, which is why the pharmaceutical industry has brought several different generations of antibiotics with different mechanisms of action onto the market since the invention of the antibiotic.
The urine is collected for precise pathogen diagnosis and a culture is grown from it in the laboratory. Under optimal conditions, the pathogens then multiply suddenly in the laboratory and can usually be identified after a few days using various tests. In the case of a mumps infection, there is no classic pathogen detection by means of culture, but an immunological test that detects certain substances in body fluids (such as blood, sperm, urine). One of these tests is called an ELISA and is also used to detect HIV, for example. An ELISA test usually costs around € 20, with the costs being borne by the health insurance company.
Read more on the subject at: Urinalysis
therapy
The treatment of testicular inflammation depends on the exact cause. Viral infections are treated differently from bacterial ones. Antibiotics are available for bacterial infections. However, these should only be used after the pathogen has been precisely identified. A broad spectrum antibiotic often helps just as well as an antibiotic specially tailored to the pathogen. However, one reserves the option of using a broad spectrum antibiotic for those cases in which the pathogen cannot be found at all. Antibiosis without prior identification of the pathogen is not necessarily considered a malpractice, but is considered “clumsy”, provided the patient is not in acute danger (for example, if the testicle is threatened).
To date, viral infections cannot be treated causally. Although there are also antivirals as counterparts to antibiotics, these currently have no proven effect on testicular inflammation. Therapy is therefore symptomatic with bed rest, cooling, and elevation of the testicle in order to encourage fluid drainage. In any case, pain relievers such as ibuprofen or paracetamol can be taken as they have anti-inflammatory and analgesic effects. With long-term ingestion and high dosage, however, it should also be taken into account that the above painkillers can hit the stomach and cause gastrointestinal complaints.
Which antibiotics are used?
Depending on the underlying pathogen, testicular inflammation can be treated with various antibiotics. If gonococci are the cause of the disease, fluoroquinolones such as levofloxacin are used. Doxycycline can also be used for gonorrhea. For more severe courses, a combination therapy consisting of cephalosporins (e.g. ceftriaxone), azithromycin and doxycycline can be chosen.
A chlamydial infection can also be treated with doxycycline. As an alternative, ofloxacin is often used against chlamydia. Treatment with glucocorticoids (cortisone) can be initiated in combination with antibiotics, especially in young men with severe testicular inflammation.
Read more on the subject at: Antibiotic therapy for chlamydial infection
In the case of a mumps infection with testicular inflammation, on the other hand, antibiotic therapy makes no sense, as the pathogen is a virus and not a bacterium.
Which home remedies can help?
Home remedies that can be used for testicular inflammation are primarily aimed at elevating and cooling the affected testicle.
Raising the testicle helps prevent the inflamed testicle from pulling on the surrounding tissue as much. Raising the testicle takes some tension off the affected structures, which can alleviate the symptoms. A so-called testicular bench can be used to raise it. A simple little pillow that can be placed between the legs and supports the inflamed testicles is sufficient as a home remedy.
Cooling is also particularly important with testicular inflammation. For example, ice packs can be used for this. If these come straight from the freezer, they should never be placed directly on the skin, as this can cause freezing. Instead, you should wrap the cold pack in a towel and then place it on the inflamed testicle. The cooling should take about ten to fifteen minutes, then you can take a break of about half an hour.
Other cooling options are curd cheese wraps or cabbage leaves. To do this, either quark or cabbage is placed on a cloth or paper towel. The quark can soak the cloth directly, the cabbage must first be kneaded a little in the cloth so that it gives off its moisture. If the compresses are not cold enough, they can be placed in the refrigerator for 30 to 60 minutes. The cooling compress can then be applied directly to the testicles.
If the testicle is infected by germs, hygiene should not be neglected. Therefore, despite pain in the inflamed testicle, the genital area should be showered and washed regularly.
Cooling the testicle
With testicular inflammation, the cooling of the testicles plays an important role. In addition to elevation, cooling can significantly improve symptoms. On the one hand, the cooling is pain-relieving, it can also downregulate the blood flow and thus lead to a reduction in testicular swelling.
homeopathy
Homeopathic remedies can also be taken against testicular inflammation. Above all, various Aurum preparations play an important role: Aurum chloratum natronatum, Aurum colloidale, Aurum iodatum and Aurum metallicum can be taken in case of testicular inflammation.
The dosage should be D6 or D12. For very minor complaints, D1 or D4 are also sufficient. Homeopathic remedies are particularly suitable when the inflammation is low. Even more pronounced testicular inflammation can be treated with homeopathy, but the effect of antibiotic therapy in bacterial inflammation should not be ignored.
Duration of testicular inflammation
The duration of testicular inflammation varies greatly depending on the pathogen and how quickly it is recognized. In most cases, the inflammation of the testicles lasts for a few weeks before it completely heals. However, with adequate therapy, the symptoms can improve significantly after a few days.
The duration of the testicular inflammation can determine whether one speaks of acute or chronic testicular inflammation. If the inflammation of the testicle lasts for less than six weeks, it is called acute testicular inflammation. If it lasts more than six weeks, however, it is called chronic orchitis.
Basically, the duration of the testicular inflammation depends primarily on how quickly the cause of the disease can be eliminated. If there is an underlying bacterial infection, effective antibiotic therapy can completely eliminate the disease after a few weeks. Viral diseases, on the other hand, are more difficult to treat because many viruses have no direct antidotes. Therefore, testicular inflammation caused by viruses can often only be treated symptomatically and therefore usually takes a little longer.
Read more on the subject at: How long does testicular inflammation last?
forecast
In the best case, the testicular inflammation heals completely within a few weeks. In this case, there are no long-term consequences to be feared. However, if the course is severe, there is a risk of testicular atrophy. This is the term used to describe a decline in testicular tissue. Testicular atrophy is always accompanied by a more or less severe loss of function of the testicle, and can be felt externally as a reduction in the size of the corresponding testicle.
Fertility does not necessarily have to be restricted, as sperm can still be produced via the second testicle. However, if both testicles are affected, infertility can occur. This is the case in around 10% of testicular infections. Since the sperm only makes up 0.5% of the ejaculate, while the remaining 99.5% contain pure seminal fluid, any infertility (infertility) cannot be externally determined. In any case, the amount of ejaculate varies from man to man between 2 and 6 milliliters.
Also read the article: How long does testicular inflammation last?
What are the long-term consequences of testicular inflammation?
The long-term consequences of testicular inflammation are rare when the condition is adequately treated, but are often severe when the complication is complete. If the testicular inflammation is not detected in time or if the pathogen is not detected, so that the wrong antibiotics are used, the testicular inflammation can be significantly prolonged.
There is also the possibility that the bacteria will settle in the testes or the surrounding tissue and form an encapsulated cavity there. Often pus develops in this cavity, in this case one speaks of an abscess formation.
An infection of the urinary tract from the inflammation of the testicles is also possible. It can lead to a urinary tract infection or a bladder infection. Chronic bladder infections can be a risk factor for developing bladder cancer, but testicular inflammation is rarely seen as a chronic trigger. In contrast, what can be caused by an inflammation of the testicles, especially in older men or people with a poor immune system, is a urinary tract infection that rises up to the kidneys. One speaks of an inflammation of the kidney pelvis (Pyelonephritis), which in the worst case scenario can develop into blood poisoning.
An inflammation of the testicles can also cause an infection of the surrounding skin. If this is not treated in time, the infection can spread unhindered and extensive skin death occurs (necrosis, gangrene). Under certain circumstances, this can lead to a life-threatening soft tissue infection and is therefore one of the most dreaded consequences of testicular inflammation.
Only in rare cases does testicular inflammation lead to sterility. It should also be noted that sterility can only occur on the affected testicle. Usually the other testicle is not inflamed, so that complete sterility cannot result. Occasionally, testicular atrophy (shrinkage of the testicle) occurs as a result of testicular inflammation caused by mumps. However, this does not affect the function.
Can testicular inflammation make you sterile?
In principle, testicular inflammation can also lead to the affected person becoming infertile (sterility). Most acute testicular inflammation affects only one testicle, and in most cases it is not sterile after the inflammation. If the affected testicle becomes infertile, the person has a second testicle that can replace the other's function. On the other hand, chronic or recurring inflammation of the testicles can definitely lead to infertility, as tissue damage can occur in the long term.
Read more on the subject at: Infertility in men
Can you get testicular infection from cold?
Cold is not one of the typical triggers of testicular inflammation. However, the cold can generally lead to a urinary tract infection in the affected person. If the pathogens spread from the urethra to the testicles, testicular inflammation is also possible. However, such a development of testicular inflammation rarely takes place.
Inflammation of the testicles as a complication of inguinal hernia surgery
If a testicular inflammation occurs as a complication of an inguinal hernia operation, a slightly different spectrum of germs must be considered than with the "classic" testicular inflammation. With an inguinal hernia, bacteria from the abdomen can spread to the skin. From there, the infection can spread to the testicles. Antibiotic therapy is also useful here. You should also check regularly whether the surrounding soft tissue is infected.
Read more on the subject at: Inguinal hernia surgery
Testicular cancer
An important differential diagnosis in addition to testicular inflammation is testicular cancer, or testicular carcinoma.While with testicular inflammation the swelling usually increases sharply within a few days and is painful, this process takes several months to years in testicular cancer. In testicular cancer, the swelling usually appears as a small, nodular change in the scrotum.
Unlike other types of cancer, testicular cancer peaks between the ages of 20 and 45. Young men are particularly affected, the incidence is 1 in 10,000. Testicular cancer is very treatable in the early stages with a cure chance of over 90%. Interestingly, the nodular changes in the testicles are usually not noticed by the affected men themselves, but very often by their partners. Therapeutically, chemotherapy or radiation follows the diagnosis.
Read more on the subject at: Treat testicular cancer
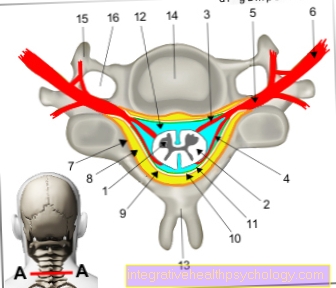
Anatomy of the testes
The testicles are located on both sides in close proximity to the limb in the so-called scrotum, or scrotum. The epididymis, in which the sperm mature, are superimposed on them and are stored. The testicles, however, have two important tasks for the male body: On the one hand, they produce semen and, on the other hand, testosterone, a hormone also known as the "masculinity hormone". Testosterone is responsible for male muscle growth, hair, and libido, as well as potency.
A testicle weighs about 15-20 grams and is about 20 ml. It is very sensitive to pressure and pain, which is why it is protected separately in many sports by a testicle protection. It is surrounded by a large number of layers of skin and connective tissue, and is also very well supplied with blood.
Since sperm cannot survive from a temperature of over 35 degrees, the temperature level in the testicles must always be kept below the actual body temperature of 37 degrees. The testes use various mechanisms for this purpose. On the one hand, it can relax the muscles in the scrotum so that it slides further away from the body together with the testicles and is less warmed by the body. On the other hand, due to the strong blood flow, the testicle can be heated or cooled, just like heating.
Read more on the topic: Sperm