Hysterectomy - the removal of the uterus
synonym
Synonym: hysterectomy (from the Greek "hyster" = uterus and "ectomy" = excision)
definition
During a hysterectomy, which is technically known as a hysterectomy, the woman's uterus is removed based on various clinical situations. A common reason for a uterus to be removed is benign growths of the uterus called myomas. However, malignant diseases such as cervical cancer or endometrial cancer, which are also cancer of the uterus, can also be reasons for having the uterus removed.
The doctor has three different removal options available (abdominal, vaginal, laparoscopic). This procedure is one of the most common in gynecology.

Indications
A distinction is made between the indications for a hysterectomy absolute Indications, i.e. cases in which the hysterectomy must be performed in any case, and relative Indications in which removal of the uterus is recommended but not absolutely necessary.
The absolute indications include:
- Ovarian and Uterine cancer,
- severe Inflammation the inner genitals (if these cannot be controlled by conventional measures) and
- threatening Bleeding from the uterus, as they can occur, for example, during childbirth (also only if this cannot be controlled otherwise).
Relative indications are:
- Muscle tumors (Fibroids) or others benign tumors in the womb,
- a Prolapse of the uterus (Prolapse / subsidence of the uterus) or Uterus subsidence after birth
- Adhesions in the lower abdomen,
- a Endometriosis,
- Bleeding disorders (frequent, heavy or painful menstrual periods) or
- one strong enlarged uterus
- A Pelvic floor depression
Ultimately, however, a woman always has to decide for herself whether she would rather live with certain pains or risks than have the uterus removed and thereby give up the possibility of pregnancy. The gynecologist can only take on an advisory role.
execution
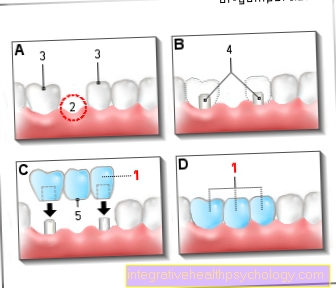
They are now a gynecologist three Procedures are available to help remove a uterus. Which of these is best suited for a particular patient must be decided individually for each case. This decision is mainly based on the disease, how old the patient is or what physical condition she is in and what difficulties or complications can be expected during an operation (e.g. due to Comorbidities, Inflammation or preceded Operations), how big and flexible the uterus is and, above all, what the patient's wishes are.
The three procedures differ according to their access to the uterus: There are abdominal, the vaginal and the laparoscopic hysterectomy. With all three options, it is important that the bladder with help of a Urinary catheter is completely emptied. This is removed again after the uterus has been removed, sometimes it has to remain in place for a few days.
The oldest method is that abdominal hysterectomy (Laparohysterectomy), in which the entire uterus is Lower abdomen Will get removed. Not so long ago it was the only variant. The decisive advantages of this access route are that there is a large overview for the surgeon, that the operation can be carried out if necessary (for example on the Ovaries) can be expanded and that adhesions are easily detachable. That is why this method is always chosen for malignant diseases. This procedure is also useful if the uterus is significantly enlarged. The disadvantage of abdominal hysterectomy, however, is the large skin incision that is made with a big scar, one higher risk of infection, one long hospital stay and one longer Recovery time goes hand in hand.
In the vaginal hysterectomy (Colphysterectomy) the uterus can pass through the Scabbard removed through it. This method is beneficial because the procedure can be performed without scarring. In addition, compared to abdominal hysterectomy, the recovery time is shortened and the pain caused is usually reduced. However, this procedure can only be done if the uterus is not too large.
The newest method is that laparoscopic hysterectomy. This is a minimally invasive procedure. The abdominal wall is not really opened, but special instruments are used Laparoscopy introduced into the abdomen through tiny incisions in the skin. On the one hand, a laparoscope is required, which contains a small camera, a magnification system and a light source, and on the other hand, of course, you need the instruments to perform the detachment of the uterus. Once this has happened, the uterus can then be removed through the vagina (laparoscopically assisted hysterectomy). Laparoscopically assisted is even more modern supracervical hysterectomyat which the cervix (Cervix) remains in the body. The body of the womb (Corpus) is cut into small pieces and then removed through the incisions in the abdominal wall.
In addition, you can also choose between one complete (total) uterine removal, in which the entire uterus including the cervix is removed, and one partial (subtotal) uterine removal differentiate in which the cervix remains in the body. In the radical hysterectomy (which occurs with cancer), not only the uterus, but also part of the holding apparatus, the upper part of the vagina, the pelvic lymph nodes and, if necessary, the ovaries are removed.
After the uterus has been removed, you should take it easy for a while. Sports activities should be avoided for the first four weeks - walks, etc. are okay if you are feeling good to keep your circulation going. Depending on the surgical method, you can start exercising again 2-3 months after the uterus has been removed.
Read more about the topic here: Abdominal muscle training after the removal of the uterus
Duration of the operation
The uterus can be removed using various surgical techniques. The method used is adapted to the underlying disease, so that not every method can be used for every disease. The duration of the operation can therefore also vary. As mentioned above, a distinction is made between vaginal hysterectomy, in which the uterus is removed through the vagina, abdominal hysterectomy, in which the removal is carried out via an abdominal incision, and laparoscopic hysterectomy, in which treatment instruments are inserted through small incisions. The latter is often referred to as a keyhole technology. The duration of the operation can vary depending on the procedure used and the underlying disease 1 to 3 hours last.
LASH procedure
In the LASH it is about the laparoscopic supracervical hysterectomy. This procedure represents a modified form of the removal of the uterus. The LASH takes place exclusively in benign diseases the uterus and is not suitable for treating cancer or precancerous diseases. Typical diseases in which the procedure is used are myomas and endometriosis of the muscle layer of the uterus (Adenomyosis uteri).
With LASH, the uterus is removed using the smallest surgical access points that are a few millimeters in size. Therefore, only very small surgical wounds arise. This procedure is known as minimally invasive surgery. Part of the cervix is left in place. Some of the advantages and disadvantages of LASH are discussed below.
Advantages: The advantages and disadvantages of LASH are currently still the subject of various studies in the context of studies. However, there already seem to be some advantages for the patients, so that LASH is definitely justified as a modern procedure. The small surgical entrances result in only small wounds that can heal very well. The patient's recovery is faster. By preserving the pelvic floor, sequelae such as incontinence or deterioration in sexuality seem to be rare. The extent to which these are rarer than with other procedures has not yet been conclusively clarified. The risk of comorbidities (morbidity) is lower than with other methods. Intraoperative complications are also less common. The inpatient stay is shorter and the recovery phase is faster. However, LASH cannot be performed on an outpatient basis. This is often mistakenly assumed, but it is not.
Disadvantages: The LASH also has some disadvantages that should be briefly discussed at this point. Since part of the cervix is left in place, the patient still has to take care of cancer screening after the uterus has been removed. Slight postoperative menstrual bleeding is also still possible. This is the case in around 10 to 17% of patients who have had LASH performed.
Removal of the uterus during menopause
Many women hope that the hysterectomy will prevent them Menopause get.
However, this is not the case. On the contrary: The distance of the uterus can to premature onset of menopause lead, especially if the Ovaries removed as well become. This is also called the surgical postmenopause because in this case the onset of menopause is triggered by the surgical removal of the ovaries.
The ovaries are instrumental to that production of the Sex hormones responsible and thus control the female control cycle. With Omission of the Hormone production put the typical menopausal symptoms, such as Hot flashes, Mood swings and Trouble sleeping a.
Even if the ovaries are left in the body when the uterus is removed, their function often fails prematurely, so that in this case, too, women enter the menopause earlier (on average four years earlier than women without a hysterectomy).
The resulting menopausal symptoms can, for example, with a Hormone therapy be treated. The the body's own female sex hormones (Estrogens) replaced. Postmenopausal hormone therapy, however, is not free of risk.
In addition to the positive influence on menopausal symptoms and the protective effect against osteoporosis, for example Risk of developing malignant diseases (in particular Breast cancer) greatly increased. Also the appearance of Leg vein thrombosis and Pulmonary embolism is thereby increased significantly. The decision to use hormonal therapy should therefore only be made after careful consideration detailed advice to be taken by a doctor.
Risks of hysterectomy

Removal of the uterus is a nowadays frequently performed procedurethat most gynecologists are familiar with. Still, it can happen during surgery too Complications come. The removal of the uterus, like any other operation, is general Operational risks.
This includes Bleeding during and after the operation, Wound healing disorders, Infections the surgical wound, as well as one Injury to neighboring organs, annoy and Blood vessels. After the operation, it is normal to have moderate bleeding for a few days.
Bleeds it however strong or if other symptoms such as fever are added, an infection must be assumed. It can also lead to the formation of a after the operation Blood clot come (thrombosis), which loosen and shoot in the lungs can (Pulmonary embolism). This is a potential life-threatening condition.
However, to prevent this from happening, every patient admitted to the hospital receives one Thrombosis prophylaxis in the form of Heparin syringes, such as Thrombosis stockings.
Generally speaking, the risks of hysterectomy are also from the Type of hysterectomy dependent. Will the uterus through the Scabbard removed, possible risks are postoperative narrowing of the vagina and / or ureter, or the development of secondary bleeding Bruising (Hematomas), such as Painful intercourse in the foreground.
When the uterus is removed by the Abdominal wall On the other hand, it can more likely lead to an injury to the bladder or the intestines, infections of the surgical wound and Adhesions come. Also Hernias will be described.
With both procedures, the blindly closed vaginal stump can sink over time, so that sexual intercourse can be painful. That too sexual desires and the sexual excitability can decrease by removing the uterus, but the opposite cases have also been described.
The complications occur altogether more often in the Removal of the uterus through the abdominal wall than with vaginal hysterectomy.
Following the hysterectomy, women often feel a few weeks of pain, but with an adequate Pain medication are easy to get under control. Some women also report a longer lasting one inertia, fatigue and weakness. However, this is controversial as many women tend to be one positive influence on their general condition after the removal of the uterus.
Having a hysterectomy increases the risk of having Urinary incontinence (Bladder weakness with inability to hold urine). This is expressed through spontaneous urination when laughing, coughing, or lifting heavy objects.
In women who have their uterus removed before menopause, the ovaries are usually left in the body. However, there is some evidence that the removal of the uterus causes the ovaries to stop functioning earlier, so that menopause may occur prematurely (up to 4 years earlier). Of course, these women will no longer have menstrual periods after the operation and will no longer be able to get pregnant.
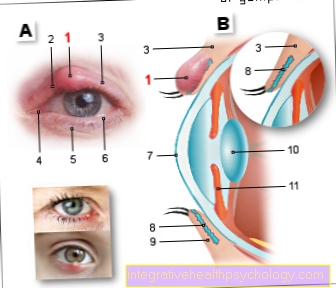
Illustration of a uterus
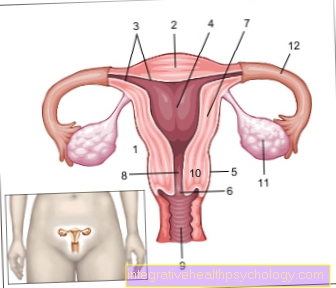
- Uterus -
uterus - Uterine tip -
Fundus uteri - Uterine lining -
Tunica mucosa - Uterine cavity -
Cavitas uteri - Peritoneum cover -
Tunica serosa - Cervix -
Ostium uteri - Uterine body -
Corpus uteri - Uterine constriction -
Isthmus uteri - Sheath - vagina
- Cervix - Cervix uteri
- Ovary - Ovary
- Fallopian tubes - Tuba uterina
You can find an overview of all Dr-Gumpert images at: medical illustrations
- Uterus - uterus
- Uterine tip - Fundus uteri
- Uterine lining -
Tunica mucosa - Uterine cavity - Cavitas uteri
- Peritoneum cover - Tunica serosa
- Cervix - Ostium uteri
- Uterine body - Corpus uteri
- Uterine constriction - Isthmus uteri
- Sheath - vagina
- Pubic symphysis -
Pubic symphysis - Urinary bladder - Vesica urinaria
- Rectum - Rectum
Complications
As with all operations, the removal of the uterus carries the risk of some complications. On the one hand, there are the usual ones Risks of anesthesia and the possibility of one infection. In addition, neighboring organs of the uterus, nerves, soft tissues and the adjacent skin can be injured during the operation. Even stronger ones Bleeding it can happen in some cases. After the procedure you can also Secondary bleeding, overshooting Scarring, Adhesions in the operated area, impaired bladder function and rarely Urinary and fecal incontinence (but only in the case of congenital connective tissue weakness and only after several years after the operation). Sexual sensation usually remains unaffected after a hysterectomy.
consequences
Probably the most important consequence of the removal of the uterus is the permanent loss of the possibility of a pregnancy. Also one Menstrual period no longer occurs (unless the cervix has not been removed). Hormonal deficiency symptoms (which are related to the symptoms of the Menopause resemble, so among other things Hot flashes and dizziness) only come about when both ovaries and the uterus have to be removed. However, these symptoms can be avoided by taking Hormones counteract.
Cost of a hysterectomy
The removal of the uterus takes place under inpatient conditions. The cost of the procedure is around 3000 euros. As a rule, the costs are covered by the health insurance.
Length of hospital stay
A hysterectomy is a inpatient stay necessary, especially in the first few days after the operation Control of the wound as well as the general condition of the patient is very important. A Hospitalization from approx 5 to 7 days is normal. Longer stays may also be necessary in the case of complicated procedures, a poor general condition of the patient or serious previous illnesses.
Length of sick leave
Patients who have had a hysterectomy are admitted to the hospital for approximately 5 to 7 days. During this time they are of course on sick leave and unable to work. Usually one is done after the operation Sick leave for about 2 to 3 weeksto ensure good healing. If there are complications or difficulties in the healing phase, a longer sick leave may be necessary. It is therefore important that patients report symptoms to the treating doctor during their follow-up examinations.
Resumption of sport
A complete healing after surgery should circa after 4 weeks be achieved. However, this depends on the course of the operation, the age and general condition of the patient and the course of the healing phase, so that no general statement can be made. In the follow-up care of the operation, gynecological examinations are carried out in which the healing process is followed, so that patients should discuss with the treating doctor individually when they can resume sporting activities. If the course is uncomplicated and has healed well, you can usually do sports again after 4 weeks. However, there are also differences in the type and intensity of physical activity. In particular, lifting heavy weights should be avoided until definitive healing.