Vaccination during pregnancy
introduction
Pregnancy represents a time in which the female body is in a state of emergency, which is why different rules apply to many drugs and medical interventions than usual.
Read about this: Medication during pregnancy
When it comes to vaccinations, there are some guidelines that should be followed in order not to endanger the health of the mother and the unborn baby.
vaccination
Complete vaccination protection is particularly important during pregnancy for two reasons:
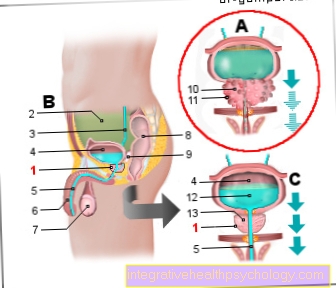
There are some infections that can be transmitted from a woman to her unborn child, as these pathogens enter the child via the blood placenta pass over and thus also infect the unborn child.
Antibodies can also be transferred in this way.
If the mother has protection against a certain disease in the form of antibodies against the pathogen, she can also transmit this to her child, who then has protection in the first three to six months of life.
This phenomenon is also called "nest protection". This slowly subsides while the child's own immune system develops accordingly.
It is best for a woman to see a doctor if she already wants to have children.
He can then use your vaccination card to determine whether all vaccinations are up to date or whether booster vaccinations may be necessary.
If the vaccination protection is incomplete, it is advisable to update it. If a live vaccine such as measles, mumps, and rubella is necessary, the woman should then wait at least three months to become pregnant.
The costs of all vaccinations carried out by the Standing Vaccination Commission (STIKO) of the Roland Koch Institute are recommended, also covered by the statutory health insurance companies.
If you take this precaution, you can avoid getting into the situation of having to worry about the vaccination status during pregnancy.
If you are already pregnant and there are gaps in the vaccination protection, the next steps should be discussed with a specialist. Together with the woman, he or she can weigh up the benefits and risks of any upcoming vaccinations and ultimately decide together with her which step makes sense next.
Most vaccinations are not given, unless there is an urgent need to do so, because the consequences of pregnancy are difficult to predict. One way or another, pregnant women are advised to stay away from people with infectious diseases or those with a fever in order to prevent infection.
In general, it is recommended not to have any vaccinations in the first trimester (i.e. in the first 3 months) of pregnancy, as there is a potential risk of endangering the embryo both through the vaccination itself and through the possible side effects. During this period one is particularly careful with the administration of any medication, as this is when the child's organs are formed.
Otherwise, a distinction is made between recommended, permitted and critical vaccinations during pregnancy.
There are many vaccinations that are completely harmless even during pregnancy.
These include vaccinations against flu, diphtheria, tetanus, whooping cough, hepatitis A and B, meningococci and polio (poliomyelitis).
Other vaccinations should be avoided if possible during pregnancy. In this group, mumps, measles, rubella and chickenpox (varicella) are particularly important.
These are so-called "live vaccines". This means that with these vaccinations, although weakened but still living organisms get into the body, they simulate a disease and cause the body to react with a defense reaction. However, these living viruses can enter the organism of the unborn child via the blood and thus infect it. This is extremely feared, especially with rubella. While the disease is usually mild in adults and the symptoms are often limited to slight respiratory problems and a skin rash, a fetus can be life-threatening from infection with rubella virus.
More than half of the children who were unborn with rubella develop what is known as "rubella embryopathy", which can be associated with severe brain damage, heart defects, eye damage and / or deafness. For these reasons, it is both important to ensure that a pregnant woman does not get infected with rubella and that she does not get vaccinated during pregnancy.
See also: Adult rubella
Other vaccinations, such as cholera, Japanese encephalitis or yellow fever, should not be given if you are pregnant. However, these are not part of the routine vaccinations in Germany and are actually only recommended in principle if a trip is made to an area in which the pathogens are even more common.
However, if such a vaccination was given during pregnancy when it was not yet known, it is not necessarily a cause for concern, as complications do not always occur.
(An exception here is a vaccination against rubella. If this was carried out by mistake during an existing pregnancy, it is advisable to carry out additional ultrasound checks on the baby during the course of the pregnancy.
Many of the recommendations made are not even based on sound medical knowledge, but are only based on assumptions.
This is because (for understandable reasons) it is extremely difficult to conduct studies with pregnant women that could provide more precise information on the influence of certain vaccinations.
The only vaccination that is expressly recommended during pregnancy is the flu vaccination (against the seasonal Influenza A Viruses).
This recommendation also applies to the period from the second trimester of pregnancy, in certain cases, for example in the case of some chronic underlying diseases of the pregnant woman, it is even recommended to vaccinate in the first trimester. With this vaccination, it has been proven that the benefits clearly outweigh the risks.
Learn more about the Flu vaccination during pregnancy.
Risks
Otherwise, of course, a pregnant woman is also at risk of the same side effects that other people can suffer from a vaccination.
These include, above all, fatigue and local symptoms such as redness, swelling and itching or tenderness of the area where the vaccine was injected.
Fever, swelling of the lymph nodes or disease-specific symptoms (for example, joint problems with rubella vaccination) may occur less frequently.
Contraindications
The usual contraindications for vaccination apply to pregnant women as well as to the general population (in case of doubt, however, these are seen a little more closely in pregnant women).
These include an allergy to chicken protein, an existing illness or immune deficiencies.