TMJ inflammation
General
Biting, chewing, speaking - everyday things for us that we are not consciously aware of. However, none of this would be possible without our TMJ, our TMJ is in constant use. But even at night, if we don't notice, we move our jaws.
But how is this multifunctional joint structured and what happens if it suddenly becomes infected?

Inflammation in the temporomandibular joint
In addition to the temporomandibular joint, humans have many other joints in the body, such as the shoulder joint, the hip joint or the finger joints, all of which have to deal with many tasks every day.
In general, inflammation in the joint is called arthritis. The most common type of arthritis is rheumatoid arthritis, or rheumatism for short.
Read more on the subject: Arthritis
The reasons for such inflammation can be different. The inflammation can be triggered by bacteria, by overloading the joint and wear and tear, by an autoimmune disease or by gout.
If only the joint capsule is inflamed, it is called capsulitis.
Read more on the topic: Temporomandibular joint
TMJ symptoms

A temporomandibular joint inflammation manifests itself primarily as pain. These can occur in phases, but they can also be permanent, especially if the inflammation is more advanced. Movement, such as yawning, speaking or eating, can make things worse.
The mouth opening can also be affected. In addition, the inflammation can also be expressed by a general feeling of illness with a slight fever.
In addition to the pain, inflammation in the temporomandibular joint is sometimes noticeable through noise. This is also the difference to "simple" pain in a joint (arthralgia). The noises arise during the movements and sound like a cracking or rubbing.
An MRI (magnetic resonance imaging), the diagnostic method of choice for temporomandibular joint problems, reveals erosions on bony structures. The bone begins to change.
Sclerotherapy can be seen on the condyle and the articular tuberosity. As the bone substance increases, the tissue becomes thicker. Furthermore, fluid collects (effusion). The structures in the vicinity of the joint surface are increasingly attacked and destroyed over time. The proteins that arise from damaged cartilage, connective tissue or bones attack the healthy structures (bones, capsules, etc.).
If the arthritis is left untreated and the improper exercise persists, the pain will get worse and the inflammation will spread. There is a risk of permanent damage such as osteoarthritis.
Read more on the topic: TMJ arthrosis
Causes of temporomandibular joint inflammation
The causes of a TMJ are wide-ranging and can also be traced back to the general factors just mentioned.
Arthritis can also develop, especially in the temporomandibular joint, if the temporomandibular joint is incorrectly loaded, especially if it is chronically overloaded.
Actually, the teeth of the upper and lower jaw only have about 30 minutes of contact within a day, so enough time for the individual parts to recover. In the event of damage, however, you may grind and press your teeth, which leads to overfunction
Read more on the topic: Grinding your teeth.
This happens particularly often at night, triggered by stress or mental illness. The muscles in particular are constantly under stress and can stiffen.
The temporomandibular joint can also become inflamed if there are faults in the teeth. These can either be natural, for example there is a gap between the teeth, causing other teeth to begin to migrate. However, the wrong load often arises from crowns that are too high, incorrect bridges, incorrectly fitting prostheses or general misaligned teeth.
Traumatic damage caused by an accident or surgery can also lead to inflammation.
Incorrect loads on the spine and crooked postures are also to blame for non-physiological loads on the joints.
Temporomandibular joint pain with earache
If there is TMJ inflammation, pain in the ears can also occur due to the anatomical proximity. The reason for this is the close anatomical proximity between the temporomandibular joint, the external auditory canal and the middle ear.
On the one hand, temporomandibular joint pain can also manifest as earache, but on the other hand, otitis media can also spread to the temporomandibular joint, since the bone that separates the two structures is quite permeable.
The symptoms often go beyond earache. It can lead to tinnitus, cracking noises when opening the jaw, pain in the teeth and headaches.
Read more on the topic: Tinnitus
If you experience ear pain, you should see a doctor to find out the exact cause. The doctor then examines whether it is, for example, an otitis media or a cranio-mandibular dysfunction (CMD), i.e. a misalignment of the temporomandibular joint that causes ear pain.
But not only misalignments or overloading of the temporomandibular joint can lead to earache. Toothache, tooth decay, wisdom teeth or root inflammation in the molar area can also trigger pain radiating to the ear.
Therapy of temporomandibular joint inflammation
The first step in an acute temporomandibular joint inflammation should always be pain relief and anti-inflammatory measures. Because in the inflammatory state, all other treatment options cannot be carried out.
There are therefore pain relievers that are also anti-inflammatory. Only when the patient can move the lower jaw freely again and no longer feels any pain when touched can physiotherapy or splint fabrication take place.
In the case of temporomandibular joint inflammation, one first tries to be as invasive as possible in order to prevent an operation as far as possible.
This is done by means of specially made splints that are used for the patient and simulate the healthy bite position for a longer period of time. If this helps to relieve the pain, certain changes can be made to the teeth in order to maintain the healthy bite position without a splint. A prosthetic restoration may also be necessary.
Physiotherapy can also be prescribed. Muscular tension can be released and incorrect posture corrected. A few relaxation exercises can also help.
Avoiding too firm and difficult to chew food can also reduce suffering
Medications can be prescribed to reduce inflammation and make pain more tolerable. You can also actively contribute to healing yourself by perhaps changing your lifestyle and reducing stress.
Often there is nocturnal overload, which can have different causes. Treating mental illness can also help.
A correct sleeping posture should be adopted at night. Lie on your back with a slightly high pillow. You can also actively observe during the day to what extent you are straining your muscles and whether your teeth are tense.
It is also useful to wear a splint to protect your teeth at night.
See below: Crunch seemed
What drugs help with TMJ inflammation?
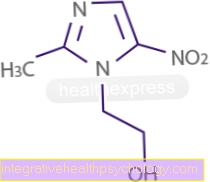
In the case of TMJ inflammation, anti-inflammatory and pain reliever drugs are most advisable. High-dose ibuprofen or diclofenac are suitable for this.
To reduce the frequency of side effects, COX-2 inhibitors can be used instead, which are also anti-inflammatory. These include celecoxib (1-2 x 200mg daily) and rofecoxib.
The drugs can either be taken in tablet form or injected by a doctor. It is preferable to take it in the form of tablets, since the spraying is associated with the risk of spreading germs.
Home remedies for TMJ
The temporomandibular joint can become inflamed if there is improper loading, e.g. due to prosthetic restorations or stress-related grinding of the teeth at night. As a measure to take at home, if your muscles are overactive you should try to reduce stress and possibly adapt your lifestyle a little.
Read more on the topic: Grinding teeth at night
Relaxation exercises can also help relax the muscles connected to the joint.You should avoid chewing gum or foods that are difficult to chew. As a home remedy, e.g. Quark compresses or heat from a red light lamp have proven successful in some patients.
However, these should be used in parallel to a splint made by the dentist if necessary. This can intercept any overfunction and relax the jaw joint somewhat.
Read more on the topic: Occlusion splint
When is an antibiotic necessary for TMJ inflammation?
Since antibiotics are principally only effective against bacteria, it should be clearly established that it is a bacterial inflammation before an antibiotic is used for treating temporomandibular joint inflammation.
It can rarely happen that bacteria spread from the middle ear or the maxillary sinuses to the jaw joint.
If the MRI image shows an accumulation of fluid within the temporomandibular joint, the fluid can be aspirated with a syringe and then examined. Antibiotic therapy can be used if bacteria are detected. Amoxycillin or clavulanic acid are particularly suitable as medicinal substances for drug treatment.
Read more on the topic: Amoxycillin
Much more often, however, temporomandibular joint inflammation is a reaction to persistent overload, without bacteria having contributed to the development. Then the use of antibiotics is prohibited.
Homeopathy for TMJ inflammation
One of the most common causes of TMJ inflammation or general TMJ problems is the overfunction of the muscles due to incorrect loading. These arise e.g. from severe grinding of teeth. The reason for this grinding of teeth at night is mostly due to mental stress, stress, nervousness or sleep disorders.
There are many homeopathic remedies that can have a supportive effect in this context:
- Echinacea
- Hamamelis virginica
- Potassium chloratum
- Myristica sebifera
- Schüsslersalz Magnesium phosphoricum
An inflammation caused by bacteria can only be combated by the administration of antibiotics.
Duration of a temporomandibular joint inflammation
The duration of a temporomandibular joint inflammation depends entirely on the individual situation of the patient. Depending on the cause and the existing duration of the pain, it may take some time for the inflammation to subside.
Since in most cases the muscles are overfunctioning, the patient is given a splint that absorbs the forces. It can take a few weeks for the joint position to improve.
However, painkillers should not be used long-term in order to avoid the side effects and possible addiction (with opiates). At the beginning of treatment, they are used to initiate measures that affect the cause of the jaw joint inflammation.
Summary information
A TMJ is a very painful and uncomfortable condition.
Movements such as chewing, yawning or speaking, which are otherwise normal and not noticed, suddenly cause great pain and unpleasant noises.
The temporomandibular joint begins to inflame, movements are only possible to a limited extent.
The many different causes allow a wide range of treatment that should be initiated as early as possible in order to stop any protracted damage early. A visit to a dentist is the first point of contact who will examine the temporomandibular joint and assess its functional condition.
In the case of temporomandibular joint problems, it is often necessary to work with other doctors from different fields (such as ENT) in order to treat arthritis well and in good time.
Structure of the temporomandibular joint
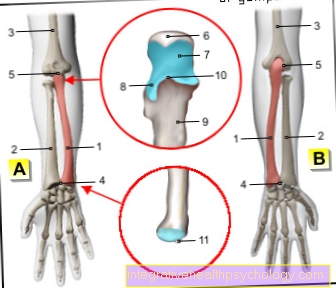
The exact name of the temporomandibular joint is articulatio temporomandibularis. The joint is a split joint.
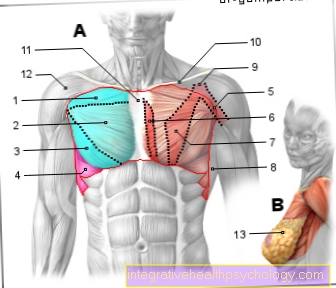
The temporomandibular joint is located just in front of the external auditory canal and consists of parts of the temporal bone, the condyles (appendages) of the lower jaw, an articular disc, as well as a joint capsule and ligaments.
The articular tuberosity (tuberculum articulare) lies further in front of the temporal bone.
Viewed from the side, the joint surface and the articular tuberosity form an S-shape. This joint is a real joint, which has cartilage-covered joint surfaces that are separated by a gap.
A liquid is created in the joint cavity, which forms a kind of grease, so that an optimal gliding on one another is made possible.
The joint pit is formed by the temporal bone, the temporal bone. The pit itself is divided into a front and a rear part by fissures (crevices).
Only the front area is the one that forms the joint surface. So this is where the condyle, the articular head, moves within the pit.
The rear part is also included in the joint, but it does not form the movement area. The so-called retro-articular cushion lies in the posterior surface. This consists of nerves, fat, veins and connective tissue.
The articular disc, already mentioned above, lies between the joint surface and the joint head. It is like a cushion and divides the joint into two separate joint chambers. Above the disc is the discotemporal chamber, below it the discomandibular chamber. Different temporomandibular joint movements take place in the two chambers. The rotational movement takes place in the discomandibular chamber and the sliding movement (translation) in the discotemporal chamber. The mouth opening is a combination of both movements.
The articular disc itself can be subdivided into a vascular-poor anterior and a vascular-rich posterior section. It is important that the rear part is divided into two leaves and thus forms the bilaminar zone. The top sheet has elastic fibers, the bottom one with friendly fibers. The retro-articular cushion lies between the two leaves, which was explained earlier in the text. The joint is surrounded by a capsule, the articular capsule.
In addition to this capsule, there are also different ligaments that are more or less involved in securing the joint. These would be, for example, the lateral ligament, the stylomandibular ligament or the sphenomandibular ligament.
In addition to securing the joint, they are primarily responsible for limiting certain movements. So it is not possible for us to push the jaw forward indefinitely, which is partly caused by the ligaments.
You may also be interested in this topic: Inflammation of the jaw
Position of the healthy temporomandibular joint
If the temporomandibular joint is healthy and does not show any inflammation, the articular disc should ideally rest on the condyle like a cap during normal clenching.
So the Discus can also be a little further ahead. If you now move the lower jaw forward, or if you open or close the mouth, the condyle and the disc move forward or backward together, so that the cap remains on the condyle. The condyle moves just a tiny bit further forward.
Of course, there can also be deviations there that are without complications and do not require any treatment.
Recommendations from the editorial team
You might also be interested in these topics
- Temporomandibular joint
- Broken jaw
- Lock jaw
- Jaw clamp
- Temporomandibular joint pain
- Cranio-mandibular dysfunction


.jpg)



.jpg)