Bone density measurement
- Dual-Energy X-Ray Absoptiometry (DEXA)
- Quantitative computed tomography
- Statutory health insurance benefits for bone density measurements
Synonyms
Osteodensitometry
Engl .: Dual Photon X-Ray = DPX
definition
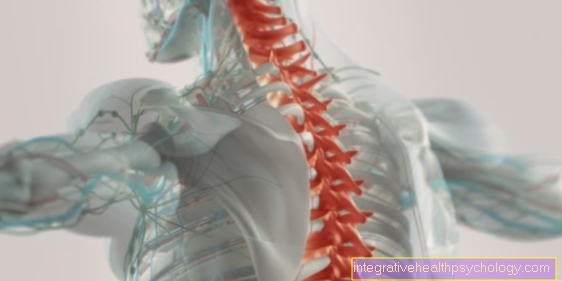
With a bone density measurement, a doctor uses a medical-technical procedure to determine the bone density, i.e. ultimately the calcium salt content of the bone and thus its quality. The result of the measurement provides information about how break-resistant a bone is and is primarily used to reduce the risk of a bone fracture (fracture risk) in the case of existing bone loss (osteoporosis) estimate.

Sequence of a bone density measurement
The Density or the calcium salt content of the bone can be determined using various methods. The following is a brief explanation of how the various procedures work.
- The DXA? Dual X-ray absorptiometry: This method measures bone density with the help of X-rays. These are two x-ray sources required. These differ slightly from each other. The Measurement of bone density occurs in two areas of the patient. These are by default Hip joint and lumbar spine. The measurement takes 15 to 30 minutes and is not painful or excessively uncomfortable for the patient.
- The quantitative computed tomography? QCT: This procedure is one specialized computed tomographyin which the physical density of the bone is determined very precisely. The process is similar to that of conventional computed tomography. During the examination, which mostly only takes a few minutes thanks to modern equipment, the patient lies on one height adjustable table. The recordings of the bone are also used here X-rays manufactured. No contrast agent is required for the display. Such recordings are called native recordings. Before the recordings are made, it is planned exactly which area one would like to display around the To keep radiation exposure as low as possible. In addition to quantitative computed tomography, the peripheral quantitative computed tomography (pQCT). It refers to more compact and cheaper devicesthat the bone density of the periphery, for example Arms or legs, measure up. Conventional QCT, on the other hand, scans the bone density of the entire body.

Dual-Energy X-Ray Absoptiometry (DEXA)
There are several different ways to measure bone density. The standard procedure, which is also used by the WHO (World Health Organization) and the governing body for osteology is recognized as the method of choice, the measurement is using X-raysthat one as Dual-Energy X-Ray Absorptiometry (DXA or DEXA) or Two-spectra X-ray absortiometry designated.
This method is ultimately based on the normal X-ray method, but in contrast to this, it does not use one, but two X-ray sources that differ slightly in terms of energy. The principle of an X-ray image is based on the fact that different materials with different densities (including different tissues within a human body) “weaken” the X-rays that pass through, ie absorb them to different degrees. This is why you can see different shades of gray on an X-ray: bones appear White, since these are usually very dense and strongly slow down the X-rays, while air-filled rooms hardly attenuate the X-rays at all and thus on the image black are. The absorption is not only from the tissue, but also from the energy the X-ray radiation dependent.
In the DEXA there are therefore two different values for each measurement point in the X-ray image (one for each X-ray tube) after the measurement has taken place. From the combination of these two results, one can finally go through the Calcium and hydroxyapatite content the bones draw a conclusion about their density.
It is important, however, that these values are not real density values in the physical sense (kg / m3), but a so-called area projected mass or Area density (kg / m2). Not all bones are equally suitable for this assessment, so usually either the Lumbar spine or the Thigh bone or that hip joint X-rayed, since the density measurements are most informative here.
This bone density measurement can be carried out either in the hospital or in the practice of an orthopedic surgeon or radiologist. To do this, the patient has to lie down on an X-ray table, where he is irradiated with the X-ray light. The whole procedure takes roughly 10 mins. The decisive advantages of this standard measurement are low radiation exposure, one quick implementation and a small risk For Measurement error.
Quantitative computed tomography
However, there are other methods that can be used. On the one hand there is the so-called Quantitative computed tomography (QCT) or the peripheral quantitative computed tomography (pQCT for peripheral body parts such as poor and legs), which is also on the X-ray technology build up and make sectional images of the body. In contrast to DEXA, QCT produces a three-dimensional Image, so you can actually calculate a physical density for each recorded volume element. This method also enables a more precise differentiation between the outer (Cortex) and the inner Area of bones (Trabeculae or. Trabeculae), which can sometimes play an important role in the diagnosis of osteoporosis. However, the QCT expands the patient a lot higher radiation exposure than DEXA, pQCT is not necessarily, but studies show that this procedure is not the same meaningful like the other two.
Quantitative ultrasound examination
The third and final option for measuring bone density is this quantitative ultrasound examination (QUS), in which instead of X-rays Ultrasonic waves be sent through the body. As a result, the radiation exposure with this method is zero. Ultrasonic waves are also attenuated to different degrees by tissue of different densities and can thus provide information about the density of bones. The best regions to conduct this research are Heel bone and the small finger bones. However, even for these areas it has not yet been proven that the QUS can be used meaningfully for the purpose of disease-relevant bone density measurement.
Evaluation of the bone density measurement:
The procedures presented differ in terms of the statements that can be made through them. The DEXA serves one Assessment of the body composition from bone, muscle and fat tissue. But it measures not the physical density of the bone, just as one cannot make a statement about the three-dimensional shape of the bone. But you get a planar representation of the bone, which can also be referred to as area density (kg / m2).
The quantitative computed tomography however, there is a lot more precise than the DEXA. However, QCT cannot capture the full body composition. She can only do this locally. With it, however, the exact physical density of the bone determine. With the help of the QCT, properties of the bone such as Flexural strength and bone strength judge very carefully. In addition, the Mineral salt content of the different bone layers can be assessed individually. With DEXA, the value is shown as the mean value of the entire bone. QCT is more sensitive to pathological changes in the bone and can indicate osteoporosis earlier than DEXA.
Please also read our page Diagnosis of osteoporosis.
Results
With all of the above methods, however, the measured values obtained cannot be compared with the results from other devices (and also not with each other). That is why it has established itself, as results no absolute density values but instead either to one T value or one Z-Value to fall back on. The most commonly used is the T value. This is a dimensionless Size that indicates the extent to which the measurements deviate from normal in multiples of a standard deviation.
The T-value of the bone density measurement indicates whether and, if so, to what extent the measured bone density of the determined average value for healthy men or women in the 30 years of age deviates. Ever lower this value is, the higher the risk of getting one Broken bone to suffer.
According to the definition (according to WHO), osteoporosis is present if the T value less than or equal to -2.5 is 2.5 or more standard deviations below the average. For values between -1 and -2.5 one speaks of Osteopenia and all values greater than -1 are considered Normal findings. A disadvantage in the practical handling of the T-value is that it only refers to healthy 30-year-olds. However, since the bone density naturally continues to decrease as people get older, a very high proportion in these age groups would at some point be regarded as "sick". For example, this would be almost half of the 70-year-old women!
For this reason, another value has been developed, the Z-Valuewho focus on healthy women or men im same age relates. This makes it possible to estimate whether the bone density corresponds to age (and gender). A z-score greater than -1 means the bone density age-typical is, values that are below are pathological.In people who have a T value that is too low but a Z value in the normal range, the reduced bone density is considered a normal symptom of old age and in these cases drug therapy is usually refrained from.
When is a bone density measurement performed?

In which cases does it make sense to have a bone density measurement carried out? The main field of application of these procedures is the diagnosis of osteoporosis. Osteoporosis is a disease also known as bone loss. Characteristic here are the decrease in bone density and the breakdown of bone substance, which leads to an increased risk of bone fractures. A distinction is made between primary osteoporoses (i.e. osteoporosis as an isolated disease; this form makes up around 95% of osteoporosis patients) and secondary osteoporoses, which arise as part of other underlying diseases. Since bone density naturally decreases with increasing age, osteoporosis is particularly a disease of older age, with hormonal influences mainly affecting women after menopause.
Read more on this topic at: Transient osteoporosis
Bone density measurement is used both in the case of known osteoporosis that has already been diagnosed in order to be able to assess the existing risk of fractures and, on the other hand, for people who are suspected of having osteoporosis. If a previously healthy person develops symptoms that clearly indicate osteoporosis, for example frequent bone fractures (especially if these cannot be explained by a previous accident), bone pain or a hunched back, a bone density measurement can be useful .
People who abuse nicotine or alcohol are at increased risk of developing osteoporosis. Even if there is a vitamin deficiency (e.g. either in states of malnutrition such as anorexia (Anorexia nervosa) or diseases of the gastrointestinal tract that are associated with a reduced intake of food components such as inflammatory bowel disease, the calcium salt content of the bones is often reduced. Since the build-up and breakdown of bone substance is also controlled by hormones, some hormonal disorders also have an effect on bone density. For example, an overactive thyroid (Hyperthyroidism) favor osteoporosis and in general women going through menopause (menopause) affected by this clinical picture, as the estrogen production of the female body decreases considerably here. Even if several cases of osteoporosis are known in the family or if there is an underlying disease such as diabetes mellitus, this predisposes to the development of osteoporosis. One of the most common reasons for secondary osteoporosis to develop is long-term treatment with glucocorticoids (Steroids) like cortisol. Bone density measurement also plays an important role in the treatment of osteoporosis in the sense of a follow-up in order to be able to assess whether the treatment is working and whether or how the disease is progressing.
Read more on the topic: What kind of pain occurs with osteoporosis?
Cost of the bone density measurement
Since the year 2000, bone density measurements have only been carried out by the Statutory health insurance paid if there is already at least one on one osteoporosis attributable Broken bone is present or a urgent suspicion insists on osteoporosis.
The early detection osteoporosis with the help of bone density measurement is, however no cash benefit.
The costs Bone density measurements vary depending on the measurement system used and the complexity of the examination.
Usually the cost of the measurement is between 40 and 80 € for those with statutory health insurance who have to pay for the benefits themselves.
In the area of private insurance, costs of € 80-100 are usually applied.
Statutory health insurance benefits for bone density measurements
Bone density measurements are different methods in which the density or the calcium salt content of the bone is determined. One uses, for example, the Computed tomography or the Dual X-ray absorptiometry. Bone density measurements are most common in the diagnosis of osteoporosis instead of. These procedures go in the case of Computed tomography and the DXA also associated with a certain radiation exposure for the patient. Therefore, the question when financing the bone density measurement is whether the diagnosis is useful and necessary.
Before 2013 the costs for a bone density measurement were only covered by the statutory health insurance if the patient had already suffered a fracture. Furthermore, the fracture must have been sustained without a special event, such as a high level of violence or a violent fall. In addition, before 2013 the health insurance companies covered the costs for patients with a strong suspicion of osteoporosis. But in this case too, patients had to pay for the bone density measurement as an individual health service (IGeL) themselves.
Since May 11, 2013 However, something has changed in the financing of bone density measurements. The joint federal committee (G-BA) relaxed the requirements for assumption of costs again. Bone density measurement using DXA is now also available for Patients with osteoporosis or an increased suspicion of osteoporosis without a fracture already occurred covered by the statutory health insurance.
An important prerequisite for the assumption of costs is that based on specific findings, the intention to specific drug therapy consists. The patients benefit effectively from such a bone density measurement in that the therapy can then be adapted accordingly and also patients who would not need drug therapy are protected from it. The measurement can be repeated after 5 years, or earlier if necessary based on clinical or anamnestic findings. The relaxation of the assumption of costs is especially important for patients who, due to certain factors such as previous illnesses or the Long-term therapy with cortisone are at risk of developing osteoporosis. These patients are now also covered.
Risk of broken bones
The Bone density measurement is very important in the diagnosis of osteoporosis, but not the only aspect that plays a role in the risk of a fracture.
Therefore, the WHO has developed a model which, in addition to the Bone density eleven more Risk factors (including, among other things, age and gender) in an algorithm that ultimately makes it possible to estimate the probability with which the person affected will: within the next ten years:
- one Hip fracture
- one Femoral neck fracture
- Vertebral fracture
- Broken spoke
will come.
Please also read our page Vertebral fracture in osteoporosis.