Complications of epidural anesthesia
introduction
The application of an epidural anesthesia is considered a very safe procedure in medicine. The likelihood that the catheter will not be in the right place and that this will result in pain (so-called failure rate) is around 1%.
The side effects and complications also include:
- Drop in blood pressure - getting up slowly and slowly (initially sitting on the edge of the bed) is advisable in the days after the operation
- Infection of the catheter injection site
- Headaches - these arise when the hard membrane of the brain was injured when the PDA was applied and cerebral fluid could escape (so-called post-puncture headache)
You can find even more information about epidural anesthesia at: Epidural Anesthesia - Procedure and Complications
Allergic reaction to the anesthetic
The human body can react allergic to any medication that is administered. Allergic reactions, both to the local anesthetic and to the pain reliever (Opioid) are possible. As a rule, the preparations used are well tolerated and these are medicines that have absolutely proven themselves in practice.
It is important that the patient informs the doctor of any previously known allergies or intolerances, ideally by presenting the allergy pass. This can prevent avoidable complications.
If no allergies are known or if the drug is being given for the first time, in the worst case scenario it can lead to "allergic shock" (Anaphylactic shock) come.
However, for every epidural or epidural anesthesia, an anesthetist (anesthetist) and other specialists present. These permanently monitor all patients and can immediately treat such complications adequately.
If you are more interested in the subject of "allergic shock", read the next article under: Anaphylactic shock
Headache as a possible complication?
With epidural or epidural anesthesia as well as with spinal anesthesia, so-called "post-puncture headaches" can occur over time.
Since in spinal anesthesia, in contrast to epidural anesthesia, the hard meninges (Dura mater) is punctured, the risk is slightly higher with this procedure. This is because a small leak can arise in the hard meninges through which small amounts of nerve fluid can escape. The resulting negative pressure leads to headaches, which can be treated well.
Is there an increased risk of a caesarean section?
Performing epidural or epidural anesthesia alone does not increase the risk of a caesarean section (Caesarean section) becomes necessary.
An increased risk of a caesarean section arises from other risk factors, such as the position of the child in the womb or complications that arise in the mother or child.
What complications can epidural anesthesia cause during the birth process?? Read more about this under: Epidural anesthesia at birth
Can this prolong the birth process?
It has been observed through studies that women who gave birth naturally with epidural anesthesia had a longer birth compared to women without epidural anesthesia.
However, it has not been proven whether the epidural anesthesia is responsible. It is assumed that the reduced pain during labor and the less pressing may be responsible for this.
Rare problems with epidural anesthesia
The following complications are mentioned for the sake of completeness, but they are extremely rare:
- Injection into the spinal space:
As explained at the beginning, the drug unfolds its effect in the epidural space. If the anesthetist accidentally injects the medication into the spinal space immediately behind it, this can slow the heartbeat, drop blood pressure and paralyze breathing.
However, these complications can be treated well by the experienced anesthetist.
- Direct damage to the spinal cord when inserting the puncture needle
- Allergic reactions to any of the drugs used
- Piercing a larger vein in the epidural space:
The blood escaping from the vein can press on the spinal cord and - if this process goes unnoticed - lead to permanent damage.The risk of this complication can be considerably minimized by checking the blood for intact clotting beforehand (=> see next paragraph!)
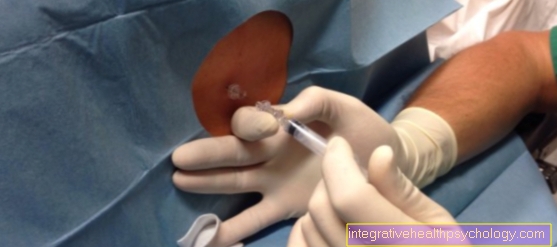
Blood clotting must also be monitored and investigated
The blood must be examined to see whether the clotting is intact. In a preliminary discussion with the anesthetist, it is necessary to clarify when drugs that inhibit blood coagulation may no longer be taken. This mainly relates to ASS 100 Heparin and Marcumar.
The following guide values for discontinuing medication can be used as a rough guide:
- 4 hours after normal (unfractionated) Heparin
- 12 hours after low molecular weight heparin
- 1 day after taking non-steroidal anti-inflammatory drugs (NSAIDs): ibuprofen, diclofenac, etc.
- 3 days after acetylsalicylic acid (e.g. Aspirin®) for single doses of more than 100mg per day
- 10 days after taking clopidogrel (e.g. Plavix®)
- Marcumar or warfarin must be switched to heparin in good time
Of course, this information does not only apply to long-term medication prescribed by a doctor: caution is also advised when taking painkillers on your own responsibility in the days before the operation.
Epidural bruise?
In the epidural space there are also veins that can be injured by the puncture. When this happens, it can bleed into this anatomical space. Usually this is small bleeding that can be reabsorbed over time.
However, if there is excessive bleeding, which is a very rare complication, the spinal cord may compress (pulled the trigger) become. Then an operation to remove this bruise is necessary. However, such an incident is very rare.
Recommendations from the editorial team
For more information on epidural complications, visit:
- Peridual anesthesia
- General anesthetic side effects
- Pain therapy
- birth
- How can you relieve birth pains?













.jpg)