Physiotherapy for a herniated disc
Synonyms
- Disc prolapse
- Protrusio
- NPP
- Disc prolapse
- lumbar disc prolapse
- Disc protrusion
introduction
Be on this side Help for self-help for patients with one in the Lumbar spine localized (lumbar) disc prolapse given. An overview is given of what those affected can do in addition to medical conservative (non-surgical) therapy to improve your health and to prevent recurrence (preventing recurrence of symptoms).

The herniated disc is a common disease of the spine. It can occur in any part of the spine. Disc material escapes and the surrounding tissue may be irritated. A herniated disc can cause muscle weakness, pain, and paralysis.
In most cases, the herniated disc can be treated conservatively, through physiotherapy, physical therapy, pain therapy, etc. An operation may be necessary in case of therapy resistance or serious incidents.
What is a herniated disc?
Of the disc prolapse is a degenerative disease, that means it is a Wear and tear. This can be unilateral long-term misuse (heavy work e.g. in a bent position) but also through genetic predisposition or previous Trauma arise. Bad posture and congenital axial misalignments (e.g. Scoliosis) can promote this incorrect load.
It comes to one Disc wear and tearbetween the Vertebral bodies takes on a shock absorber function. In the case of a herniated disc, disc material (a distinction is made between the fibrous solid outer portion, the Annulus fibrosus, from the gallery-like inner Nucleus pulposus) shifted from the intervertebral disc.
One distinguishes three stages, which are often in everyday use all under the term disc prolapse be summarized. The first stage is that Intervertebral disc bulge (Protrusion), no tissue has detached itself, only a displacement occurred.
It follows as second step the herniated disc (Prolapse), the outer Annulus fibrosus has torn, disc material has shifted.
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
In the third stage (Sequester) the leaked material no longer has contact with the intervertebral disc. Depending on the location of the displacement, different symptoms can occur. Of the disc prolapse can also be complete asymptomatic run away.
A herniated disc can occur in any section of the spine. In the Thoracic spine (BWS) he only comes a lot Rare in front.
At the most common the herniated disc is localized in the Lumbar spine (LWS), also in the cervical spine (Cervical spine), it occurs frequently, depending on the previous incorrect load.
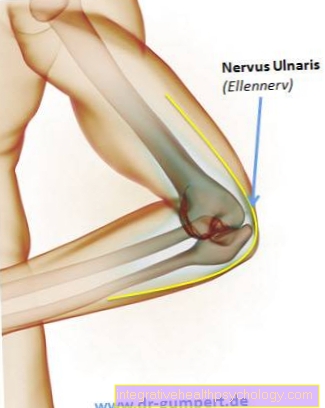
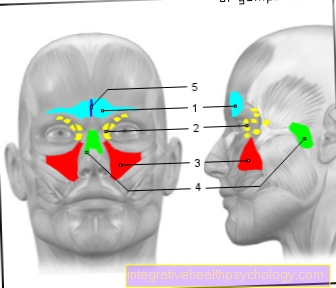
If the disc material irritates surrounding structures, it can Pain or Functional failure of muscles and nerves come. One speaks of one segmental disorderwhen disc material presses on the nerves emerging from the spinal canal and as a result the structures that are supplied by these nerves can no longer be properly supplied.
It can too Paresthesia, Muscle weakness and paralysis or Pain come in the supply area, reflexes (e.g. patellar tendon reflex) can also fail.
In severe cases you can too Malfunctions on bladder and Intestines occur immediately (not) medical to be clarified!
Of the disc prolapse can in most cases conservativei.e. treated without surgery.
Read a lot more information on this topic at: What is a herniated disc?
Physiotherapy for a herniated disc
A patient comes with the diagnosis disc prolapse For physiotherapy, a new diagnosis is first made by the therapist in order to be able to respond to the individual situation of the patient. In a anamnese an attempt is made to find out the causes of the incorrect loading, possible previous illnesses are clarified that have an influence on the development of the herniated disc or that could influence recovery. There will also be another one physical examination made to find out exactly what the patient's problems are.
A disc prolapse can do many various symptoms show, depending on the direction in which the disc material emerged and which structures are being irritated.
In the physical therapy becomes a more targeted Treatment plan individually tailored to the patient and treatment goals agreed with him.
This is independent of the location of the herniated disc Goal of physiotherapy one possible full function recovery to reach and a Pain reduction to achieve. Depending on the severity of the herniated disc, functional maintenance and compensation strategies can also be developed.
In the course of the disease, it is important to give the back the right stimuli to heal and to minimize the incorrect strain. No movement is not a solution. A posture correction should be worked out during therapy. A healthy back is a flexible back.
Of the disc prolapse (whether operated or treated conservatively) heals over time more and more off. Depending on the course is one full recovery possible, structures are irreversibly damaged, can Compensation mechanisms be worked out. During physiotherapy, posture at work or in everyday life can also be analyzed and suggestions for improvement found. The patient should be made in therapy Doing exercises at home independently and an awareness of one healthy posture develop. Relief postures should as much as possible be avoided, a conscious posture and behavior prevent the herniated disc from recurring or worsening.
When should physiotherapy be started?
The herniated disc is an injury and is associated with a natural inflammatory reaction. If the patient has been operated on, the operation will also trigger an inflammatory reaction. This is initially expressed among other things through pain and is supposed to protect the body from overload.
In this phase, the injured structures should be given rest so that they can regenerate themselves. In the pain-free area, movement can be carried out as part of physiotherapy. In therapy, soft tissue treatments (e.g. gentle massage) can improve the care of the affected area or reduce pain. If necessary, techniques from manual lymphatic drainage can be used to provide support. A gentle therapy is in the foreground.
After an operation, it is essential to follow the surgeon's instructions. Certain movements can be restricted or certain forms of exercise prohibited.
You might also be interested in this topic: Exercise after and after a herniated disc
Exercises and techniques
Together with the therapist, strategies are worked out how the patient can protect his back in everyday life (workplace design, back-friendly lifting ...). Proper handling of the back is made in the Back school Developed. This can possibly also be done in Group therapy occur.
The Mobility of the back should be restored as best possible in all directions. Come to this Mobilization techniques (Stretching, manual therapy, gymnastic exercises).
The same is true of protecting the back from further improper strain stability important. A targeted one Strengthening program is part of the physiotherapeutic treatment for a herniated disc. Depending on the status of the patient are targeted Muscle groups strengthened. The Abdominal muscles stabilizes the back from the front and can counteract a hollow back. The Back muscles stabilizes the back from behind. The Cervical spine can also be mobilized through targeted movements, here too there are strengthening exercises that improve posture. Shortened muscles (e.g. shoulder and neck muscles) can be stretched.
The so-called autochthonous Back muscles goes from vortex to vortex and plays an important role in the Stabilization of the spine. It cannot be controlled arbitrarily or only with great difficulty. Through targeted coordinative training, the Back muscles however strengthened become.
It is important to build a strengthen functional Core muscles, or also core muscles. The choice of exercises is varied, but should match the Therapist agreed because damaged structures can quickly become overloaded again if incorrectly executed.

Our Spine makes it possible for us to keep ourselves in an upright posture all day and to bend, stretch and turn in countless everyday activities. Our Band washersthat turn out to be Buffer between the individual vertebral bodies and move passively with every movement are a weak point in this system. At repeated unilateral movements and long-term static loads, such as. when sitting for a long time the gelatinous one gives way Disc nucleus single-sided printing from and moves in the opposite direction. Even bent over activities such as gardening or “incorrect lifting” over a long period of time lead to pressure on the posterior fibrous ring in which the core of the intervertebral disc is embedded. Constant Obesity, one weak core muscles and weak connective and supporting tissue can as Risk factor to be added.
At some point it will stop Fiber ring the pressure load no longer stood, it comes to small tears, until mostly one sudden movement or a lifting operation acutely painful herniated disc arises. This acutely painful event is preceded by a long process, which is usually already recurring Back pain attacks made noticeable.
However, a herniated disc can also be considered Incidental finding at a Nuclear spin (MRI) can be determined without the person suffering from or in the past. The pain picture is thus i.a. depends on the location of the herniated disc.
More than 100,000 people are annually in Germany at one Herniated disc operated on, unfortunately many of them continue to complain of pain even after surgery. The decision to operate should therefore only be made after targeted conservative therapy and careful consideration of all factors, unless there are acute symptoms of paralysis or bladder and rectal weakness.
In any case, regardless of whether the herniated disc has to be treated conservatively or surgically, patients need one immediately targeted and consistent medical pain therapyto eliminate acute pain and one To prevent chronification. A physiotherapy treatment be introduced so that the patient is actively involved in the healing success and can prevent long-term damage and relapses (relapse).
Please also read our topic: Exercises for a herniated disc
Here you can go directly to ...
- Functional tests for a herniated disc
- Treatment plan for a herniated disc
- Treatment plan for a herniated disc in the subacute state
- Exercises for a herniated disc
Optimal behavior in the event of an acute herniated disc

- Exact diagnostics and consistent pain therapy by the doctor
- Temporary relief - here the emphasis is on temporarily for a few days - lying down in the most comfortable position possible. It is not decisive whether the supine position in a step bed, side position or even prone position, which depending on the location of the herniated disc can also bring relief. Experience has shown that it makes the most sense to change the positions taken frequently depending on the perceived relief and to start with light movement exercises as soon as possible while lying down.
- Heat applications in the form of hot water bottles, grain bags or single-use mud packs are often perceived as pleasant and pain-relieving due to the increased blood flow and muscle relaxation achieved.
- Walking, usually you can get out of bed after a few days and the lying phases can be interrupted by walking. Moving forward in a more or less upright gait caused by the pain initiates a slight mobilization of the pelvic joints and the lumbar and thoracic spine. The movement sensors in the joints and muscles that are activated when moving are superimposed on pain-firing nerve receptors and there is pain relief in the back. If possible, climbing stairs and walking should also be done outdoors.
- Taping the lumbar spine
From the beginning it makes sense to put a tape in the lumbar spine.
This mainly serves to relax the muscles and improve the metabolism.
The so-called kinesio tapes do not have the task of supporting the spine. Since the kinesio tapes constantly trigger a stimulus through the skin through movement, pain relief without side effects and easier movement is achieved.
Read more on this topic at: Taping the herniated disc
The "right lying"
Starting position: supine position / side position in bed
Execution: Basically, the patient must be able to relax as well as possible in his chosen position, regardless of what the doctor or therapist recommends.
Experience shows that most intervertebral disc patients prefer a flexible, point-relieving mattress that hugs the surface of the body. A hard mattress has been recommended in specialist circles for years and has fortunately disappeared from the minds of manufacturers, orthopedists and physiotherapists. The hard, unyielding support, especially in the side position, is often a torture method for the pain-afflicted disc patient due to the increased pressure on the shoulder and pelvic girdle.
In addition to the point-elastic mattress, a soft neck support pillow adapted to the shape of the cervical spine and possibly a foam cube, a blanket under the lower legs or a knee roll can be used as a relief aid (so-called step storage.) A suitably high case can be upholstered with a blanket and place it under the lower legs. Inflatable, inexpensive storage cubes are also available from specialist retailers.
Some patients prefer to be in the lumbar lordosis, i.e. you need a small pillow or a rolled towel under your back to support your lumbar spine.
In the side position, a small pillow in the lumbar spine or a pillow between the knees can provide additional relief, as the lumbar spine is not brought so far forward in the rotary motion.
Getting out of bed with little pain

Starting position: Lie on your back in bed
Execution: Basically, when getting out of bed, the torso should be stabilized by tensioning the stomach, pelvic floor and back muscles and then moving “en bloc”.
First, the legs are set at a 90 ° angle, the lower arm is stretched out forwards and then turned into the side position while the muscles are tense. At the same time, the legs are brought out of bed by propping up the upper arm. The weight of the legs makes it easier to get up to sit.
When turning "en bloc", the muscularly stabilized spine is rotated little and any pain that may arise is prevented.
The way back to the supine position takes place in reverse.
When the pain has subsided enough that it is possible to leave the house again, physiotherapeutic treatment is indicated in addition to medical and physical therapy.
The physiotherapeutic findings
Taking the anamnesis = Pain history: there is often a long-term "back career"
Collection of visual findings: A clear pain relief can often be observed here
Palpable finding: Here one often feels a strong, often one-sided, protective tension in the muscles
In the case of the physiotherapeutic assessment, first Anamnesis, visual and tactile findings carried out. Then follow Function, provocation and nerve tests, which are checked at regular intervals during the series of treatments in order to establish a follow-up and possible Improvements to document. This makes the patient stronger motivated, his treatment and be active Exercise program to continue intensively.
Therapy on the device
Can also be used for therapy equipment (e.g. leg press to Theraband) can be used, among other things by the disc prolapse caused muscular deficits e.g. to train in the leg or arm muscles or to strengthen the back / stomach itself.
The patient should always an exact Instruction in the devices, the performance and the intensity of the exercises. In the case of surgical treatment, the Information provided by the surgeon regarding mobility and stress get noticed.
Therapy can also go through at this stage Soft tissue techniques (passive stretching techniques, massage, trigger point therapy, fascia techniques) can be added to treat changed structures, improve the nutritional situation of the tissue or relieve pain. Also techniques of manual therapy can be part of the therapy to reduce functional disorders of the structures and to restore mobility in certain sections of the spine.
Other therapeutic procedures
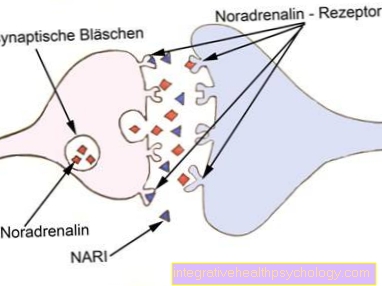
To support the therapy of the herniated disc, the Electrotherapy in question by certain Types of currents can specifically stimulate damaged nerves or weak muscles or relieve pain. Pain reduction can be achieved with the help of Painkillers can be achieved.
There are various health insurance offers in the area Rehabilitation and preventionthat can be used in addition to the therapy of the herniated disc. Relief through aids in everyday life, a redesign of the workplace to improve the ergometry can still be helpful.
Read more about this topic at: Rehabilitation after a herniated disc
Physiotherapy pain
It may be that during the physiotherapy exercises Pain occur. This is not a mandatory reason to stop therapy. Before repeating the exercises with the Discussed by therapist become. The pain can be sore muscles or shortened structures that cause pain due to the stretching. Also one Incorrect or overloading may be the cause of the pain.
Summary
The herniated disc is a diverse and very individual clinical picture which can be treated in physiotherapy through pain-reducing measures such as massage techniques, soft tissue treatment, trigger points, mobilization techniques such as manual therapy, stretching and strengthening exercises.
The treatment is strongly dependent on the findings and includes the patient's everyday life (posture at work, back-friendly behavior in everyday life). Of the Treatment success is from the localization and Severity of the herniated disc and from the consistent Cooperation of the patient dependent.
Already in the acute state of the lumbar Herniated disc Targeted behaviors and exercises accompanying medical pain therapy can bring relief. With decrease in pain and increase in strength through targeted Strength training Depending on the intensity of the training and the pain symptoms, the physical performance for everyday life and work improves within a few weeks and months. The increase in stability and back-friendly behavior in everyday life and at work can significantly increase the chance of remaining symptom-free for a long time. Growing trust in one's own body, a decrease in fears and the increasing suppression of acute pain events from the mind allow normality to return to life.