lung infection
Synonyms in a broader sense
Medical: pneumonia
Synonyms in the broader sense:
- Lobar pneumonia
- atypical pneumonia
- interstitial pneumonia
English: pneumonia
Definition of pneumonia
Pneumonia are inflammations of the lungthat are either acute or chronic.
The alveoli and / or the tissue between them (interstitium) can be affected. The inflammation rarely affects the entire lungs, usually individual sections of the lungs, the lobes of the lungs, are affected.
There are different pathogens: mostly bacteria or Virusesbut also mushrooms.


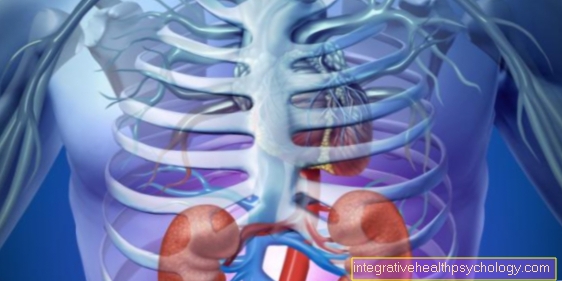
Anatomy and location of the lungs
- right lung
- Windpipe (trachea)
- Tracheal bifurcation (Carina)
- left lung
Frequency (epidemiology)
Occurrence in the population
Pneumonia is the most common fatal infectious disease.
Overall, it is the fifth most common cause of death. The official rate of new cases in Germany is around 140,000 to 200,000 annually, but a high number of unreported cases is assumed.
The probability of death in previously healthy lungs is around 5%. However, if pneumonia is acquired in hospital (so-called nosocomial pneumonia), the mortality rate is up to approx. 70%.
Classification
There are several forms of pneumonia:
- community-acquired pneumonia
- nosocomial pneumonia (acquired in hospital)
- Inflammation of the lungs (pneumonia) with a serious underlying disease (kidney or heart failure, diabetes)
- Aspiration pneumonia (aspiration means to "breathe in" the stomach contents; e.g. in the case of alcoholism or diseases of the esophagus)
- Inflammation of the lungs (pneumonia) in the case of immunosuppression (e.g. if the immune system is weakened by HIV)
Signs of pneumonia
The signs of pneumonia can be different because, strictly speaking, there are two forms of pneumonia:
- typical pneumonia
- atypical pneumonia
1. In the typical form, there is a sudden strong cough, combined with purulent expectoration, shortness of breath, difficult, labored breathing with pain, and high fever, as well as chills.
The temperatures rise quickly to over 38.5 degrees, breathing is accompanied by rattling noises. In the laboratory tests, the doctor will typically find increased inflammation parameters and an increased number of white blood cells in the blood.
2. The signs of atypical pneumonia are less fulminant: The classic is a subacute, insidious onset, with a fever below 38.5 degrees. Atypical pneumonia usually develops from a flu-like infection and marks a further worsening of the previous illness. Patients feel less sick and the cough is more dry than it is accompanied by sputum. Rattling noises are weak in the lungs, if at all not audible.
The gold standard in the examination of lung diseases is examination with a stethoscope. With its help, conclusions can be drawn about the nature of the disease, since changes in the sound patterns over the lungs when breathing always indicate the direction of the disease. For example, rattling noises during a lung examination indicate secretion deposits in the airways. The rattling noises can be fine, medium or coarse bubbles, and are further divided into wet and dry.
Coarse rattling noises are more likely to indicate a disease of large airway sections, and vice versa. So the signs of pneumonia depend on the type of inflammation. An increasing, slow worsening of an existing bronchitis, as well as a sudden, severe course, can speak for pneumonia.
In children, regardless of the type, the following symptoms are in the foreground: shortness of breath, with painful breathing up to cyanosis due to insufficient oxygen supply and subsequent circulatory collapse. Due to the shortness of breath also increased breathing rate, painful breathing, and nostril breathing.
Read more detailed information on this topic at:
- What are the signs of pneumonia?
- Pneumonia incubation period
- pain in the back
Typical complaints and symptoms
In terms of symptoms, one can differentiate between typical and atypical pneumonia. Here, these symptoms should be presented in a simplified manner using the list.
- Typical pneumonia
- Start: quickly
- Chills: +++
- Cough: +++
- Fever: over 39 ° C
- Rapid breathing: +++
- Pathologist Auscultation *: +++
- X-ray: segmental
- Atypical pneumonia
- Start: slowly
- Chills: +
- Cough: +
- Fever: below 38.5 ° C
- Rapid breathing: +
- Pathologist Auscultation *: -
- X-ray: diffuse, interstitial
*Pathological auscultation means that when listening with the stethoscope, instead of the normal breathing noise, one hears a so-called rattle or crackle.
Read more on the topic:
- Symptoms of pneumonia
- Pneumonia pain
- Pneumonia
Causes of Pneumonia
Pneumonia can be caused by either:
- bacteria
- Viruses
or - Mushrooms
to be triggered.
The causes include:
- an immunosuppression (e.g. from medication, HIV)
- after an operation
- from hypothermia
- from poor ventilation of the lungs
- from being bedridden
Read more detailed information on this topic at:
- Causes of Pneumonia
- Coronavirus- how dangerous is it?
Dry pneumonia without a cough
Both a typical and a atypical pneumonia usually goes with to cough hand in hand. It is either dry or productive and can suggest pneumonia. Sometimes pneumonia goes hand in hand without a cough.
This is especially the case in older patients, and makes diagnosis more difficult, since the absence of a cough is rather untypical. Atypical pneumonia in particular can take a mild course with a slight, unproductive cough. These may then be dismissed as a smoker's cough, or ignored entirely. Pneumonia remains potentially life-threatening even without a cough!
Diagnosis of pneumonia

Several areas are consulted to diagnose pneumonia.
When interviewing the patient (anamnese) For example, fever, chills, cough, discolored sputum and chest pain are noted.
The physical examination reveals an infiltrate. If the doctor taps the lungs, the knocking sound is muffled compared to healthy lung tissue.
The stethoscope can then be used to detect rattling noises when breathing in and so-called bronchial breathing. Bronchial breathing means breathing with a breathy character (sounds like "ch" when you inhale and exhale).
X-rays are particularly groundbreaking in the diagnosis of pneumonia. X-rays should always be carried out in two planes (i.e. from the front and from the side).
With the help of these radiological recordings, not only can the diagnosis of pneumonia be made, but above all the localization of the same can be recognized here.
Read more on the topic: Chest x-ray (chest x-ray)
Chest pressure- these are the causes
In order to be able to start the therapy in a targeted manner, the pathogen must be detected.
This can e.g. For example, using sputum (sputum) either under the microscope or by growing cultures. Usually, however, a broad spectrum antibiotic is used for therapy, which covers a large number of pathogens.
So-called serological diagnostics also play an important role. Here the antibodies formed by the body are detected after at least one week of illness.
Antibodies are formed against foreign substances, in this case bacteria, viruses or fungi, in order to "Intruders" to fight. The counterpart to the antibodies, i.e. what is reacted against, is called an antigen. Antigen and antibodies function according to the lock and key principle. This antigen can also be detected. In this way you can determine the genetic makeup of the pathogen.
The blood sample / laboratory values determine important inflammatory parameters in the blood.
These include the CRP value (C-reactive protein) and the white blood cells (leukocytes).
The higher the two values, the more severe the inflammation. The normal values of CRP are <5 mg / l, the normal values of leukocytes are 4-11 million / ml.
These reference values can fluctuate depending on the evaluating laboratory.
In rare cases, an MRI scan of the lungs can also provide further information. The MRI shows soft tissue processes particularly well, significantly better than the classic x-ray images of the lungs. The problem with an MRI of the lungs is how the air in the lungs shows tissue. Thanks to the helium gas, which is harmless to humans, the display has been significantly improved in recent years:
Read more on this topic under: MRI of the lungs
Find out all about the topic here: Diagnosis of pneumonia.
Therapy pneumonia
If the pneumonia is severe, hospitalization is indicated.
In this case, a severe course is understood to mean a breathing rate below 30 per minute, which means little oxygen in the blood and low blood pressure. If the course is mild, outpatient treatment may be sufficient.
The administration of antibiotics is a major pillar of pneumonia therapy.
The antibiotics are administered depending on the pathogen.
For pneumococci and staphylococci, which are among the most common pathogens, penicillin or derivatives are often prescribed, for example.
In the case of atypical pneumonia, so-called macrolide antibiotics are administered due to the fact that it is mostly chlamydia and mycoplasma that are the cause. Since the spectrum of pathogens is often not immediately available, broad-spectrum antibiotics are used, since pneumonia requires immediate treatment.
Broad spectrum antibiotics are antibiotics that are effective against as many pathogens as possible.
In the case of viruses and fungi, however, antibiotics are ineffective.
The course of viral pneumonia cannot be influenced by medication.
As a support, breathing can be made easier for the patient by administering oxygen. If there is pain, painkillers are given and you have to drink a lot (or give fluids by infusion).
For more information, read on here: The therapy of pneumonia.
How contagious is pneumonia?
Pneumonia are usually through bacteria caused. The bacteria lead the list of pathogens Streptococcus Pneumoniae, Haemophilus influenzae, and Staphylococcus aureus on.
These are very widespread pathogens that we encounter every day. Still, we don't get pneumonia all the time. How can that be?
All of the above-mentioned pathogens are contagious and therefore potentially dangerous for the body. However, our body usually has a well-functioning one immune systemwhich successfully fights these bacteria as soon as they enter the body. Only for very old or very young people (so toddlers, or babies) there is an increased risk of infection. After all, their immune system is not yet - or no longer - so well developed. For a healthy person between the ages of 10 and 60, pneumonia should generally not be contagious.
However, a certain distance and basic hygienic dimensions are of course still required so as not to give the pathogens a chance. Staying in the same room or fleeting body contact should be possible without any problems.
Relatives can also come with you during this time Vitamin supplements and Cold teas take precautions. Brief ventilation is also recommended in order to reduce the bacterial load in the air and the risk of infection.
Complications
Severe pneumonia can lead to septic shock (sepsis = blood poisoning) and respiratory failure (respiratory failure), which requires intensive medical care.
Abscesses (collections of pus) can form in the area of the lungs and empyema (pus) in the area of the lung membrane.
An abscess is a collection of pus in unformed cavities, e.g. E.g. within the lungs. An empyema, on the other hand, is an accumulation of pus in existing cavities, for example in the lung membrane.
Read more about this on our website Pus in the lungs
Also a possible pleural effusion (liquid in the gap between the leaves of the lung membrane), i.e. water between the lung membrane, which heaped as a layman "Water in the lungs" can arise as a result of pneumonia.
As a result of bed rest, which is usually appropriate in the case of pneumonia, there is a risk of thrombosis.
In hospitals, however, this is counteracted by thrombosis injections (e.g. Clexane®, Fraxiparin®, etc.).
You can find out more about this topic at: thrombosis
Pneumonia is often associated with pleural empyema. At this point it is recommended to deal with the topic of "pleural empyema": Pleural Empyema - What's Behind It?
prophylaxis
There is prophylaxis for pneumonia insofar as the STIKO (Standing Vaccination Commission) of the Robert Koch Institute has recommended vaccination against pneumococci as a basic vaccination for all children since July 2006.
This doesn't just apply to children. If you were not vaccinated as a child, you should do so as soon as you are older than 65 and have more frequent upper respiratory infections.
The vaccination is also recommended if you have a known immune deficiency or suffer from a chronic illness (e.g. chronic bronchitis, diabetes).
In the event of a flu epidemic, flu vaccination should be considered.
The flu can also trigger pneumonia.
For more information, see:
- Vaccination against pneumococci
- Vaccination against pneumonia
Duration and prognosis of pneumonia
Typical pneumonia does not go beyond 2-3 weeks with proper treatment. In individual cases, courses of up to 12 weeks are possible, from 8 weeks onwards one speaks of a chronic illness.
Atypical pneumonias are usually less fulminant and milder. Often the patients do not even perceive an atypical pneumonia as such and assume a severe cold.
As a rule, this should also have subsided within 2 weeks. With typical pneumonia, the condition worsens within the first week. Then the healing phase begins.
Complications can occur in immunocompromised or elderly patients: Although the average mortality rate is (Fatality of the disease) at low 0.5%. However, unfavorable factors can negatively affect this value. The CRB-65 score provides information about the possible progression of pneumonia.
C stands for confusion, R for respiratory rate, i.e. breathing frequency, if this is more than 30 breaths per minute, and B for blood pressure values that are below 90 to 60. The 65 ultimately stands for an age of 65 years or older. One point is awarded for each relevant element of the CRB65 score. While at 0-1nem point the lethality is still estimated at 1-2% percent, if all four points apply it is a high 31.2%. Therefore, patients to whom all four points apply are always treated in the intensive care unit.
Read more on the topic:
- Duration of pneumonia
- dragging of pneumonia
- Pneumonia in old age
Pneumonia developed in certain situations
Pneumonia in the baby

Special precautionary measures apply to babies, both in the event that they are sick themselves and in the event that their parents or siblings are sick.
The immune system of children is not fully developed until the age of 10, it is still learning. As a result, babies cannot defend themselves against the pathogens as effectively as adults. This means, on the one hand, that they get sick more quickly and more frequently, but also that the diseases are more severe because their bodies have not yet had that much practice in eliminating the bacteria.
This is why pneumonia in toddlers is particularly critical and should always be presented to a doctor. Symptoms are similar to those of adults, but they differ in some places:
Babies and children naturally have an increased breathing rate. However, this is increased again, so-called nostrils and shortness of breath occur. Rapid breathing causes a lot of moisture to be exhaled from the body, causing water to be lost and the skin to retract, especially in the chest area. While older children can still cough up the cough, babies often swallow it and vomit as a result. High fever and chills are also typical. Because this is a life-threatening situation, babies and toddlers are usually admitted to the hospital as an inpatient.
A vaccination against the most common pathogens can be carried out from the 2nd month of life.
Read more on this topic at: Pneumonia in the baby
Pneumonia in the child
Pneumonia in children is a common infectious disease. The pathogens are usually bacteria such as pneumococci or viruses such as RS viruses or mycoplasmas. The symptoms are often unspecific, which is why pneumonia can unfortunately go undetected under certain circumstances. Common symptoms are fever, cough with or without sputum, and feeling very sick. If pneumonia is suspected, a doctor should be consulted immediately so that therapy (antibiotics) can be started at an early stage.
For more information, see: Pneumonia in the child
Differences from pneumonia in an adult
Pneumonia in children is by no means uncommon. Basically it is the same clinical picture as in adults: Pneumonia is an infectious inflammation of the lungs that can be caused by viruses, bacteria or fungi. In children, pneumonia is still one of the leading causes of death, especially in developing countries.
In the industrialized nations, however, there are good treatment options available, so that pneumonia only occurs in very rare cases ends fatally. The pathogens are usually transmitted through sneezing or coughing. A particularly high risk of transmission between children is in the Community facilitiesin which children spend most of their time.
These are, for example, schools, kindergartens, sports clubs or even children's homes. The risk of transmission is particularly high due to the close contact. In infants and young children, the immune system is not as mature as it is in adults, which is why transmission can easily take place. Pre-existing conditions such as cystic fibrosis or asthma increase the risk for children of developing pneumonia.
The symptoms of pneumonia are not always immediately apparent, especially in young children and infants, unlike adults. Infants and young children can get through Unwillingness to drink and one bloated stomach become conspicuous.
Apathetic behavior, a high fever, and rapid and shallow breathing can also indicate pneumonia. Coughing and erecting the nostrils while breathing are typical. This is known as Nostrils. In older children, the symptoms are similar to pneumonia in an adult.
Pneumonia after an operation
After operations (OP) the immune system is weakened because the body has to use energy to regenerate the operated area. This is a natural process and unfortunately it cannot be avoided. The more “construction sites” the body has to take care of, the more susceptible it is to external attacks.
In addition, after certain operations, such as transplants, it may be necessary anyway to slow down the immune system so that the transplant is not rejected immediately.
If there is also postoperative artificial ventilation or large-lumen accesses such as a central venous catheter, there is also the risk of the plastic tubes and needles used becoming colonized with pseudomonads. Pseudomonas aeruginosa is one of the most common pathogens of nosocomial (acquired in hospitalPneumonia.
Unfortunately, this circumstance cannot always be prevented even by the strictest hygiene measures, so that many patients fall ill with a subsequent infection after surgery. This is particularly favored by a long hospital stay. Unfortunately, according to the name, the greatest number of pathogens is still found in the “hospital”.
Read more on this topic at: Pneumonia after an operation
forecast
The forecast for outpatient pneumonia is quite good, because the mortality rate is well below 5%.
In comparison, the death rate from pneumonia acquired in hospital is 70%. On the one hand, this is due to the different spectrum of pathogens: hospital germs are usually more resistant.
You can find more information on the topic here: multi-resistant hospital germs
On the other hand, it is due to the fact that pneumonia usually occurs as a superinfection in hospitals; it is acquired in addition to an already existing disease because the immune system is already weakened.
Vaccination against pneumonia
There is no vaccination against pneumonia, only against one certain bacteriawhich can cause pneumonia. These bacteria are called pneumococci.
According to the Standing Vaccination Commission (STIKO), vaccination is carried out as part of the Basic immunization recommended for all infants and young children. It consists of a dead vaccine (PCV13), which is contained in three partial vaccinations is administered and against 13 different bacterial strains of the Pneumococci should protect.
The first dose is given at 2 months of age, the second at 4 months of age, and the third at 11 to 14 months of age. At Premature babies a fourth vaccination is added. Vaccinations against varicella, measles, HiB and influenza can also protect against pneumonia.
history
The so-called Legionella pneumonia takes its name from its first appearance at a gathering of former legionaries.
One after the other was coughing and fever ill. They got infected in the shower because the shower water had not been heated to high enough and so the pathogens, the so-called legionella, were not killed.
Inhaling these pathogens into the lungs caused inflammation.
Anatomy of air ducts

- Right lung - Pulmodexter
- Left lung - Pulmo sinister
- Nasal cavity - Cavitas nasi
- Oral cavity - Cavitas oris
- Throat - Pharynx
- Larynx - larynx
- Windpipe (approx. 20 cm) - Trachea
- Bifurcation of the windpipe -
Bifurcatio tracheae - Right main bronchus -
Bronchus principalis dexter - Left main bronchus -
Bronchus principalis sinister - Lung tip - Apex pulmonis
- Upper lobe - Superior lobe
- Inclined lung cleft -
Fissura obliqua - Lower lobe - Inferior lobe
- Lower edge of the lung - Margo inferior
- Middle lobe (right lung only) - Lobe medius
- Horizontal lung cleft (between upper and middle lobes on the right) - Horizontal fissure
All medical illustrations





.jpg)