Pulmonary function test
General
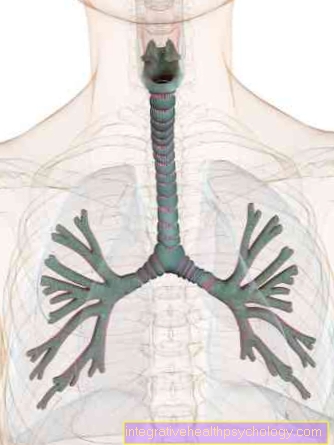
With the lung function test, the doctor can determine whether the lungs are working properly. Depending on the type of examination, it is measured how much air is moved through the lungs, at what speed and pressure this happens and in what ratio the breathing gases oxygen (O2) and carbon dioxide (CO2) be replaced. In this way, serious lung diseases can be recognized at an early stage, sometimes before the patient notices his breathing problems himself.
Indications
The typical symptoms for which a pulmonary function test is ordered are Shortness of breath, to cough and Expectoration. Of course, the signs of illness have to persist for a long time to give rise to a pulmonary function test. Besides, this is Investigation makes sense for smokersas they have a greatly increased risk of various lung diseases. Some patients are also sent to a pulmonologist if a X-ray shows abnormal lung findings showed or abnormally high red blood cells in one blood sample were found. Since the so-called erythrocytes transport oxygen through the blood, their increased occurrence suggests that the lungs cannot otherwise absorb enough vital oxygen. In some cases, however, the lung function test is also carried out as a routine measure. For example, asthmatics should have regular exams. For Competitive athlete and for some professional groups, a control of the lung function is also useful.
Diseases
In classic spirometry, it is checked whether the lungs are adequately ventilated, i.e. inhales and exhales sufficient air. If this is not the case, it is called a ventilation disorder. There are different types of ventilation disorders.
Obstructive ventilation disorder: If the airways are narrowed, the patient must always exhale against a certain resistance. The air can no longer easily escape from the lungs. This is the case with bronchial asthma and chronic obstructive pulmonary disease (COPD) the case.
Restrictive ventilation disorder: In some patients the problem is that the lungs or the chest (thorax) are not stretchable enough. That suggests hardening of the lungs (Pulmonary fibrosis), a pleural effusion, scarring after a lung operation or a diaphragmatic palsy (the diaphragm is too high).
- Neuromuscular ventilation disorder: The transmission of signals from the brain to the respiratory muscles is disturbed or interrupted. Mostly this is due to an injury to the responsible nerves, such as paraplegia.
values
In order to understand what knowledge the doctor receives from a lung function test, one should look at the values determined.
Tidal volume (AZV): The amount of air that the patient moves during normal, calm breathing (approx. 0.5 l).
Inspiratory capacity (IC): The maximum volume of air the patient can inhale after exhaling normally (approx. 3.5 l).
Inspiratory reserve volume (IRV): After a normal inhalation, everyone can breathe in a little extra air. This is the so-called "inhalation reserve" (approx. 3 l).
Expiratory reserve volume (ERV): Even after exhaling normally, you can still exhale additional air with a little tension (approx. 1.7 l).
Vital capacity (VC): The amount of air that you can exhale again with maximum effort after a maximum inhalation (depending on size, etc. approx. 3.3-4.9 l).
One second capacity (FEV1, Tiffeneau test): The volume of air that can be exhaled again within one second after maximum inhalation (at least 70% of vital capacity).
- Peak flow (PEF): Here you measure the strongest air flow that leaves the lungs when you exhale quickly (max. 600 l / min).
Spirometry
The Spirometry is also called the "small lung function test". The doctor can use spirometry to determine the Vital capacity (i.e. the amount of air that a person can breathe in and out maximally) and the One second capacity (How many liters of air are moved in one second when you exhale strongly).
The measuring device that Spirometer consists of a hose system with a mouthpiece and is connected to a recorder. This shows the amount of air breathed as a curve, similar to the Cardiac currents during an EKG to be recorded. The patient encloses the mouthpiece with his lips and is also given a nose clip. This is to prevent air from escaping through the nose and thus not being registered during the measurement. Then the patient is told how to breathe during the exam.
Usually the normal inhalation and exhalation measured (i.e. that Tidal volume). Then the patient should breathe out as deeply as possible, then breathe in as deeply as possible immediately afterwards and then exhale again hard and quickly. Normal breathing is then recorded again. As a rule, the procedure is repeated several times in order to obtain several meaningful curves.
In this pulmonary function test, it is extremely important that the Patient cooperates well and understands the instructions for breathing. The examiner should motivate him to really do the exercises with full force. This is certainly particularly difficult with children, because they are not easily inspired to take the test in the somewhat frightening environment and with the uncomfortable nose clip.
The pulmonary function test is risk free and also not painful. In some patients, however, the heavy breathing can cause one brief dizziness to lead.
Full body plethysmography
This investigation lead above all specialized internists, so Pulmonologists, by. The patient is in a airtight cabin, similar to a telephone booth. He gets a Mouthpiece and breathes through the so-called pneumotachographs initially normal and then possibly accelerated or particularly deep in and out. The resulting pressure differences in the chamber are then measured.
Most of the time the doctor also runs one Closure pressure measurement by. The mouthpiece is blocked and the patient breathes briefly against the resistance out. With whole-body plethysmography or body plethysmography, the lung volume and also the Bronchial resistance be measured. The advantage of this Pulmonary function test lies mainly in the fact that the patient do not actively participate got to. Normal breaths are enough to get meaningful values.
The plethysmography is absolutely harmless. There is neither pressure nor radiation exposure and the door of the chamber can of course be opened open anytime. Only for Claustrophobia patients the investigation could be a problem as the chamber is relatively small and for a successful measurement absolutely must be closed.
Peak flow
The lung function test by Peak flow is less informative, but has the advantage that it can be carried out by the patient himself is. He just needs the peak flow device with the Lips enclose, inhale and exhale as hard as you can. The determined value is then read off in l / min either digitally or with a pointer. He is depending on the age, sex and size of the patient.
The peak flow is used to determine the force with which the Exhale patient can. It is very useful for people with chronic lung disease such as asthmatics because it works quickly Changes in your lung function Can be detected. For many, one is recommended diary, in which the peak flow value is entered once or several times a day.
Spiroergometry

Spiroergometry is the most complex lung function test. It doesn't just make statements about that mechanical breathingbut also about the Cardiac function, the blood circulation, the Gas exchange in the lungs and the Muscle metabolism.
While normal spirometry only measures the breathed volume of the lungs, the doctor also records the concentration of the two breathing gases oxygen (O2) and carbon dioxide (CO2). This investigation is on a Treadmill or one Exercise bike carried out. Because the patient moves a lot, he not only gets a mouthpiece but also wears a tightly fitting breathing mask. In addition, electrodes are applied for an EKG. The patient then has to move with different intensities on the treadmill or ergometer and, if necessary, has blood drawn from his ear in between to determine the lactate value.
Spiroergometry plays an important role in various specialist areas. In sports medicine, the doctor can examine the patient's performance and stamina. It gives the cardiologist statements about possible functional impairment of the heart. Pulmonologists use spiroergometry above all when the shortness of breath or breathing difficulties are performance-related, so the patient only has problems when he has to breathe hard. The great advantage of spiroergometry compared to spirometry is that you can find out whether the breathing mechanism is disturbed (so there is simply not enough air in the lungs) or whether the gas exchange is not working properly (So there is enough air, but the oxygen in it cannot be properly absorbed or the carbon dioxide cannot be released properly).
Further information
Further information on this topic can be found on the following pages
- bronchial asthma
- Endurance performance diagnostics
- COPD
- COPD diagnosis
- To run
- Performance diagnostics
- Pulmonary function test


.jpg)

















.jpg)