Lung transplant
introduction
The lung (Pulmo) is used for gas exchange and breathing.
Since it thus fulfills vital tasks, a lung transplant is only carried out if no other therapy promises a cure.
Strictly speaking, the lung consists of 2 lungs, a right and a left.
Depending on the severity and indication of a lung transplant, one lung, both lobes or several lung lobes are removed and then the functional lung from a donor is inserted.
Causes / indication

A lung transplant is only used for advanced lung diseases, as every transplant always involves a certain risk.
Before doing so, it must be ensured that all possible conservative therapies have not worked or are no longer effective.
However, if the patient suffers from shortness of breath at rest (Dyspnea) and if his life expectancy without a transplant is less than 18 months, a transplant will be performed.
There are various clinical pictures that can lead to a lung transplant.
These include the
- Muscoviscidosis (Cystic fibrosis) with bilateral bronchiectasis
- idiopathic pulmonary fibrosis
- a chronic obstructive pulmonary disease (COPD) with alpha-1 antitrypsin deficiency
and - emphysema of the lungs
such as - pulmonary hypertension caused by heart defects
and - sarcoid.
Other causes of a lung transplant can also be Langerhans cell histiocytosis (Histiocytosis X), Lymphangioleiomyomatosis, or bronchiolitis obliterans.
However, it is important to know that none of these diseases mean that a lung transplant is necessary.
Rather, the patient must be analyzed on the basis of his symptoms and laboratory values in order to determine whether therapy with medication can still lead to success, whether the damage has progressed too far and healing is impossible or whether it still makes sense to transplant a new lung because the patient would thereby gain several years of life.
For example, has a patient with Cystic fibrosis only a relative one-second capacity of 30% (FEV1 = 30%), this is definitely an indication for a lung transplant.
For a patient with a Chronic obstructive pulmonary disease, who also has a relative one-second capacity of 30%, it may be that this patient does not need a lung transplant, but can live well with the correct medication.
This example shows that a lung transplant always has to take into account many different factors and that there is no specific value from which one says that a transplant is absolutely necessary.
However, there are some characteristics when a lung transplant should definitely be considered.
A 6 or 12 minute session is used for this purpose Walking test, in which the patient is asked to run as far as he can in the given time.
One patient in need of a lung transplant is only lying in this time around 500m back there he out of breath at the slightest exertion device.
Patient selection
It is often difficult to decide which patient will receive a lung transplant and which will not. For one thing, there is a strong one Lack of donor lungs and therefore the number of possible transplants is very limited.
However, a patient must meet certain criteria to be eligible for a lung transplant.
On the one hand, the age of the patient is allowed 65 years do not exceed.
What is more important besides the age is the General condition of the patient.
A patient in good general condition, that is, at healthy nutritional status and one stable psyche such as no comorbidities is better suited for a lung transplant than a mentally unstable person or a person who already has major problems with other organs.
The better the general condition of the patient, the more likely it is that the complications after the transplantation will be survived well and that there is a real chance of recovery.
If the general condition of the patient worsens dramatically again and again, which means that the patient has to repeatedly go to the hospital because of breathing difficulties, he always gets one higher oxygen supply, suffers from increased Weight loss and always has heart problems, then the time has come for one Lung transplantation inevitable becomes.
It is then important that the patient is adequately informed about possible risks and the upcoming time after the operation.
This means the patient must be aware that a transplant is always with immunosuppressive drugs being treated and that it may increase after the lung transplant despite the medication Rejection reactions can come.
In addition, a lung transplant is not always the key to success and it may even be that, despite the transplant, the lungs do not function properly and the patient may need another lung transplant.
Waiting list
A patient and their pulmonologist, who specializes in lung disease, must make the decision that they would like to have a lung transplant.
Once that decision is made and the patient is all necessary criteria fulfilled, the patient must always be available, day and night, by phone or cell phone.
The patient leaves their number at a transplant center.
If a suitable donor lung is considered, the patient must immediately go to the hospital to undergo the operation.
The constant accessibility is extremely important, as otherwise the patient may miss the chance for a new lung.
Contraindications
Not every patient who wants a lung transplant can get it guaranteed. One reason for this is the Lack of donor organsOn the other hand, there are certain contraindications for which one should refrain from a lung transplant.
For example, a contraindication is one Blood poisoning (sepsis).
Even with one Tumor in the lungs A lung transplant is not recommended, as life expectancy can hardly be increased.
Chronic dysfunction of other organs, such as a Kidney failure or severe liver damage can be a contraindication.
Probably the most serious contraindication is one Nervous system disorder or one severe mental illness.
Also to heavy use of drugs, alcohol or nicotine can be a contraindication.
Since a transplant is always associated with immunosuppression, are also chronic infectious diseases a contraindication.
Is the patient with a multi-resistant bacteriume.g. MRSA, infected, a lung transplant cannot be performed until the patient is free of germs.
Preparation time
A lung transplant is always with one certain risk connected.
In order to keep the risk as low as possible, the patient has to undergo some tests before his transplant.
First of all, the Thoracic area by means of X-ray and Computed Tomography (CT) carefully examined.
After detailed Pulmonary function tests and examinations of the heart by means of Echocardiography must also use the abdominal area Abdominal ultrasound must be carefully examined.
In addition, the patient must Blood drawn to rule out a tumor or infection.
There is also one Right heart catheter examination added, since the pressure conditions in the lungs have to be analyzed.
In addition, there must always be a psychology control as a transplant is always associated with great psychological stress.
When all of these tests and examinations are completed, the results are sent to a lung transplant center and a team of doctors then decides whether a transplant is necessary or how quickly the patient should have the chance of a new lung.
Since a lung is usually not available immediately, the patient has to respond every 3 months to a control examination appear at the transplant center.
The transplant

Once an appropriate donor lung is available, the patient will be notified by the transplant center and should avoid further eating and drinking.
Once the patient has arrived at the hospital, a decision is made as to whether the lung transplant or whether the patient has to go home without a new lungs.
If a patient is transplanted, however, they are usually taken directly to the operating room and the anesthesia Is initiated.
Usually both lungs are transplanted, since a lung transplant of only one lung often causes severe infections in the "old“Lungs arise.
A cross-section is made in the thorax to remove the lungs. Then the diseased lung is removed and the new donor lung is inserted. First the Lung bronchi and the Pulmonary veins connected to the new lung, finally the Pulmonary arteries.
As soon as the blood can circulate again, the lungs should start working.
The incision is closed and the patient is first placed on the Intensive care unit housed.
The stay in the intensive care unit should not be longer than a week in around 15% of all cases However, complications arise that result in a longer intensive stay.
In unproblematic cases, it includes after the stay in the intensive care unit about 3 weeks inpatient hospital stay at which the patient physiotherapeutic is intensively looked after.
After the transplant, the patient receives immunosuppressive drugs, the one prevent possible rejection of the lungs should.
However, these drugs suppress the whole immune system of the patient.
Therefore, after a lung transplant, patients are more prone to Mushroom- Viral or Bacterial diseases.
In order to keep this as low as possible, the patient is also given medication to prevent possible infection. So should possible risk of infection reduced and the patient now has the option of a new, more carefree life.
Figure lungs
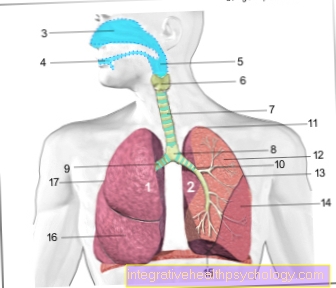
- Right lung -
Pulmodexter - Left lung -
Pulmo sinister - Nasal cavity - Cavitas nasi
- Oral cavity - Cavitas oris
- Throat - Pharynx
- Larynx - larynx
- Windpipe (approx. 20 cm) - Trachea
- Bifurcation of the windpipe -
Bifurcatio tracheae - Right main bronchus -
Bronchus principalis dexter - Left main bronchus -
Bronchus principalis sinister - Lung tip - Apex pulmonis
- Upper lobe - Superior lobe
- Inclined lung cleft -
Fissura obliqua - Lower lobe -
Inferior lobe - Lower edge of the lung -
Margo inferior - Middle lobe -
Lobe medius
(only on the right lung) - Horizontal cleft lung
(between upper and middle lobes on the right) -
Horizontal fissure
You can find an overview of all Dr-Gumpert images at: medical illustrations