Mastoiditis
Synonyms in a broader sense
Mastoiditis, mastitis, ear, otitis media
English: Mastoiditis
Definitely mastoiditis
Mastoiditis is a purulent inflammation of the bony cells of the mastoid process, which pneumatizes, i.e. are filled with air.
These cells are connected to the tympanic cavity (Cavum tympani = part of the middle ear), which contains the ossicles.
Read more on the subject at: Pus in the ear

Cause / origin
Mastoiditis is a complication of acute otitis media that has not completely healed.
The reasons for the lack of healing are as follows:
- Difficult drainage of wound fluid from the ear
- Choosing the wrong antibiotic (wrong therapy) for otitis media
- very aggressive (virulent) pathogens or
- poor immune system of the patient
This complication of acute otitis media has become rare because antibiotic therapy is available and the determination of an antibiogram to identify the pathogen and its resistance level (checking the effectiveness of various bacteria-killing drugs (antibiotics)) enables the optimal drug to be selected.
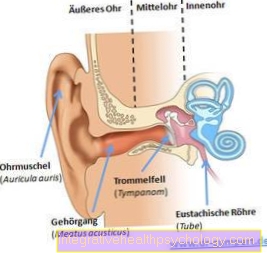
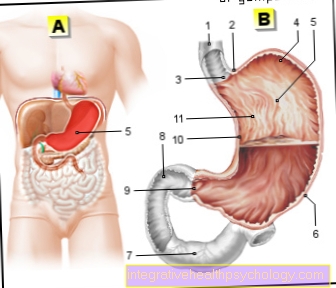
Figure ear
- Outer ear
- eardrum
- Balance organ
- Auditory nerve (nervus acousticus)
- tube
- Mastoid process
Pathogen
The causative agents of mastoiditis are always bacteria. Most often found here Pneumococci, but also Streptococcus pyogeneswhich Scarlet fever triggers or Haemophilus influenzae. In addition to these common germs, a wide range of other bacterial strains can be found as pathogens.
Although mastoiditis is always caused by bacteria, it can also as a result of a viral otitis media (Otitis Media) arise.In this case a so-called Superinfection. Bacteria settle in the mucous membrane of the middle ear that has been attacked by the virus, spread widely and finally penetrate the mastoid cavities.
Is mastoiditis contagious?
Mastoiditis is caused by germs of a bacterial nature, which as such are in principle contagious. However, the inflammation is not limited to the mastoid, but is usually the result of an otitis media, which in turn usually arises from the rise of an inflammatory process from the nose and throat area. These can be diseases such as colds or sore throat.
Since the mastoid cavities form a space that is closed off from the outside direct infection with the actual mastoiditis is almost impossible. However, the causative infectious disease, which was also the trigger for otitis media and mastoiditis, can very well spread to another person. However, this does not mean that the infected person will also develop otitis media or mastoiditis as the disease progresses. Normally, the person concerned suffers only the usual form of the original infectious disease, in the course of which, of course, a new otitis media with subsequent mastoiditis can occur.
Symptoms / complaints
The complaints of a Otitis media (Earache) do not subside, but continue to exist or increase in intensity.
fever occurs again and blood count changes / changes in the Laboratory values with an increase in the inflammatory values of C-reactive protein (CRP), sedimentation rate (ESR increase) and the white blood cells (Leukocytosis) are to be diagnosed.
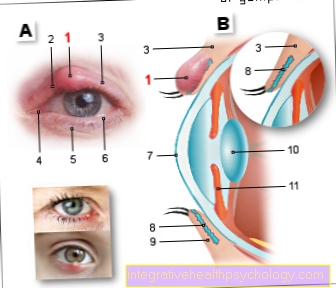
The auditory findings are characterized as follows:
- the rear upper wall of the Ear canal, to which the mastoid antrum (mastoid process) is adjacent, sinks as a result of inflammation and accumulation of secretions / pus
- Tenderness on the mastoid process (externally palpable bones behind the ear);
- in the X-ray image there are shadows that indicate inflammation with fluid (secretion);
- If there is an attack on the bone in the ventilated (pneumatized) bone space, this is in one Computed Tomography - Admission (CT) of the petrous bone (part of the temporal bone).
The breakthrough of the pus that forms in the ventilated cells of the mastoid process can occur in several ways:
- Subperiostal abscess
A pasty swelling appears on the mastoid process behind the ear, causing the posterior auricle to disappear.
As a result of a long-lasting otitis media (Otitis Media) it can also become a chronic form of mastoiditis come which only very unspecific symptoms shows. Therefore, in this case, one speaks of masked mastoiditis. Due to its gradual course, it can remain unnoticed for months. In particular, the main symptoms of mastoiditis such as fever or severe pain and reddening of the mastoid can be completely absent. The complaints are mostly unspecific, such as persistent headache or tiredness.
However, due to the proximity to the brain tissue, chronic mastoiditis is also one potentially very dangerous disease. In the case of a bad or not healing one Otitis Media therefore special care is required.
Diagnosis CT
For diagnosis and especially for preoperative presentation of mastoiditis CT is the cranial treatment of choice.
Compared to conventional X-rays, CT offers many advantages in mastoiditis. Dangerous intracranial complications, which occur when the inflammation breaks through into the skull, can be ruled out. By showing all adjacent structures, the surgeon can gain important information about the best course of action should an intervention be necessary.
The mastoid cells appear cloudy in acute mastoiditis due to the purulent inflammatory process. If the inflammation attacks the bone, the fine septa, which form the individual small chambers of the Mastoid process subdivide, based. This can also be shown well in the CT and is known as bone fusion. On the other hand, it is much more difficult to diagnose a creeping chronic mastoiditis.
Diagnosis MRI
In addition to CT, another form of imaging is available with MRI. Because this technology is due to the way it works inferior to CT imaging of solid tissue such as bone is, she will rarely used specifically to rule out mastoiditis.
Even so, symptoms such as a headache may result in an MRI that will detect mastoiditis. The main indication here is a increased accumulation of fluid in the mastoid cells. However, this is not enough as clear evidence of mastoiditis. Further indications are, for example, a contrast enhancement of the mucous membrane or visible disturbances of the flow in the mastoid cavities.
Therapy mastoiditis
The inflammation-related melting of the bone in the air-filled system of the middle ear makes immediate surgical treatment necessary and cannot be treated with medication alone.
The inflamed cells are removed and the patency of the connection to the middle ear is ensured.surgery
If mastoiditis is already advanced, antibiotics and opening of the eardrum are no longer sufficient for treatment. In this case, mastoiditis is treated surgically.
Here is under general anesthesia of the Open bone behind the ear to remove infected areas and clear out the purulent inflammation. The pus gets through thin tubes, so-called Drainages derived. A distinction is made between simple and radical mastoidectomy.
In the simple mastoidectomy only the affected part of the bone is removed, while the surrounding structures remain intact.
If the mastoiditis is very purulent, this procedure alone may not be sufficient. In this case the surgeon performs a radical mastoidectomy by. In addition to the mastoid, parts of the tympanic cavity and the back wall of the external auditory canal are removed. This creates a larger cavity with a connection to the external auditory canal, which the doctor can more easily clean. However, since the structures of the Middle ear usually also have to be removed, this can result in severe hearing loss on the affected side. Thanks to modern surgical methods, normal hearing function can be maintained in certain cases, even with radical mastoiditis.
Regardless of the surgical technique required, there will always be one additional inpatient therapy with antibiotics carried out. This serves to kill any bacteria that may still be in the body.
Operation time
A mastoidectomy is always performed as an inpatient in the hospital. Even if the actual operation usually relatively short lasts and quickly leads to improvement is a Remain in the hospital for about a week necessary due to the postoperative treatment with antibiotics. Antibiotics are usually administered via a venous access and must be given in high doses in order to kill any bacteria that are still present. The surgical wound usually heals very quickly due to its small size. Most patients are symptom-free by the time they are discharged from the hospital.
Complications
Due to the destruction of the bones, it is possible that the ossicles are also destroyed and the sound conduction and sound amplification function of the middle ear is considerably restricted:
It can turn out to be a Hearing loss develop.The attack / inflammation of the bony mastoid process (Mastoiditis) can lead to duct formation to the semicircular canal system (Balance organ) lead to vertigo attacks (dizziness) can lead.
The inflammation can extend into that Inner ear as well as the Facial canal or even in that Cranial cavity (Meninigitis).
forecast
Since the cholesteatoma can lead to the above-mentioned serious complications with brain involvement (e.g. meningitis), one is surgical supplies necessary.
First, conservative treatment is used as preparation for the operation antibiotic ear drops (e.g. ciprofloxacin), which act against Pseudomonas aeruginosa, the common pathogen responsible for inflammation.
The goals of surgical treatment are the complete removal of the cholesteatoma, the healing of the bone healing, the prevention of otogenic complications (affecting the ear), the restoration of a functional ossicular chain and the closure of the eardrum defect to close the tympanic cavity in the direction of the external auditory canal.
There is both a closed and an open one Surgical technique.
In the open technology a bone cavity is created that includes the tympanic cavity, the mastoid cavity, and the mastoid cells affected by inflammation. The cholesteatoma is cleared out, i.e. the horn-forming skin cells are removed and a wide connection to the external auditory canal is also established.
In the closed technology a so-called mastoidectomy is carried out, i.e. the mastoid process, the cells of which are aerated and lined with mucous membrane, is completely cleared out, so that only its bony walls remain.
If the ossicles are also attacked by the pearl tumor, one can Tympanoplasty, the reconstruction of the sound conduction apparatus. This procedure is performed after the cholesteatoma has been removed.
A distinction is made between the five basic techniques according to Wullstein of tympanoplasty (restoration of the ossicular chain):
- Type I - myringoplasty (eardrum plastic)
If there is an eardrum defect and an intact, vibratory ossicular chain, the eardrum defect is covered / closed and a connection with the bones is established. - Type II - ossiculoplasty
In the case of a defective ossicular chain, missing parts are replaced or the missing parts are bridged. - Type III
If the transmission chain is defective and no longer functional, the operation allows for direct sound transmission from eardrum or an inserted transplant on the inner ear. - Type IV
The sound pressure transmission takes place without the ossicular chain. - Type V
Fencing operation: the eardrum and stapes are connected to one another in this method.
A hearing improvement can be achieved through this operation if the ear trumpet (tube) is continuous and the inner ear is functional.
- Type I - myringoplasty (eardrum plastic)