Meniscus damage
Anatomy / definition
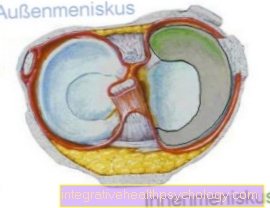
The meniscus is a crescent-shaped cartilage system in the area of our knee joint. In each knee there is a so-called External and internal meniscus. Due to their position between the thigh and lower leg bones, the menisci act as shock absorbers by cushioning the forces acting on the knee joint, for example when jumping from a great height.
They also ensure an even distribution of pressure and compensate for unevenness between the articular surfaces within the knee joint. They increase the contact surface of the joints. The menisci thus protect the articular cartilage and participate in the distribution of synovial fluid within the knee. The synovial fluid enables sliding painless movements.
The so-called outer meniscus, which is located laterally in the knee joint, has a greater range of motion than the relatively immobile inner meniscus. In contrast to this, it is not connected to the ligaments of the joint capsule. This fact explains the much more frequent injury to the medial meniscus. If there is an injury to the outer or inner meniscus, one speaks of so-called meniscus damage. This creates cracks in the fibrous cartilage system of the meniscus, which impair their functionality within the knee joint. Meniscus damage is a relatively common injury, with men being affected about twice as often as women.
causes
The main causes of meniscus damage are, on the one hand, an age-related regression of the cartilage tissue, the so-called Wear and tear, and secondly in an acute injury to the meniscus. The fibrous cartilage system of the meniscus suffers a loss of substance with increasing age and constant stress, which leads to its weakening. This results in a reduced resistance and elasticity to forces acting on the knee joint. The risk of meniscus damage increases.
Since the meniscus is nourished indirectly via synovial fluid, such damage is only partially capable of regeneration. The meniscus tissue becomes brittle, cracks form within the cartilage and the risk of tearing increases. This progressive loss of substance is completely normal from a certain age and occurs around the age of 40. However, there is an increased risk of premature wear for some professions, professional athletes or leisure activities. For example, tilers or skiers are exposed to increased knee strain. Meniscus damage due to an acute injury is usually caused by so-called "Twist and fall accidents“Caused, as they are often found in the sporting field with footballers or skiers. In most cases, the knee is fixed by the body weight while the foot is turned away. These pressures and forces acting at an angle from the side cannot be dampened well by the menisci and cause meniscus damage, especially if the meniscus has already been damaged.
Direct violence or jumping from a great height can also cause meniscus damage. A far less common cause of meniscus damage is genetic Disc meniscus. The meniscus is designed as a flat disc, in contrast to the normal crescent to sickle-like shape. This pathological deformation reduces the contact surface and increases the load on the meniscus. Because of this, the above-mentioned signs of wear and tear and a high susceptibility to meniscus damage occur prematurely.
Symptoms
Typical symptoms of meniscus damage are stabbing Pain in the kneewhich can occur even with the smallest movements and in severe cases even at rest. In acute injuries, the pain is sudden and shooting. In contrast, the age-related meniscus damage leads to a gradual increase in pain over a longer period of time. In addition, the knee joint may be restricted in movement. Depending on the location of the meniscus damage, an effusion in the knee joint is also possible. Especially the middle area of the meniscus is well supplied with blood and can lead to a tear Effusion to lead. The knee is then usually swollen and warm. However, not every tear in the meniscus necessarily causes symptoms and may go unnoticed, so that it will grow back on its own.
Appointment with a knee specialist?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Detect / diagnose

A precise one Diagnosis is important to determine the severity and the localization of the meniscus damage and is usually provided by a family doctor or orthopedic surgeon, a specialist in diseases of the musculoskeletal system. The doctor will conduct a thorough survey beforehand regarding the type, frequency and under which circumstances the pain in the knee joint occurs.
He will also be interested in your lifestyle, such as work and sporting activities, as well as knee operations that have already taken place. This is followed by special tests during the physical examination, including as Steinmann- or Payrtest labeled with her Knee joint carried out. The doctor uses a certain procedure to move the thigh in relation to the lower leg and thus stress the inner and outer meniscus. Depending on which movement causes pain, the doctor can narrow his suspicion of meniscus damage to the extent that it is an injury to the inner or outer meniscus.
The examiner will also check for pain on touch and problems with stretching the knee joint. The doctor diagnoses a knee joint effusion using the so-called "dancing kneecap".The kneecap is encircled in a C-shape with the thumb and middle finger and pressed in with the index finger. With an effusion, the examiner feels the kneecap floating in the liquid. If an accident was the cause of the meniscus damage, the doctor will advise you X-ray image of the knee joint to exclude injuries to the surrounding bony structures. Age-related changes in the knee joint, such as a Joint wear, can be made visible in the X-ray image.
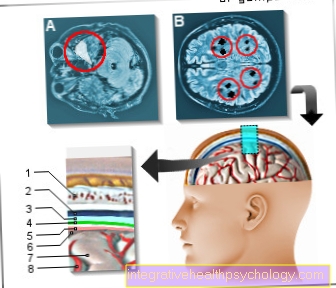
Meniscus damage itself cannot be shown in the X-ray image. That is why the most important imaging instrument when meniscus damage is suspected is the so-called X-ray-free Magnetic resonance imaging, also known as nuclear spin. Here, organs and soft tissue, such as the menisci, are shown in high resolution in sectional images. A healthy meniscus shows itself as a continuous black stripe, wear due to light spots and meniscus damage as a light tear in the image. This diagnostic agent can do that extent and the place the meniscus damage can be optimally identified.
An equally reliable method, which is associated with a minimal surgical procedure, is that Arthroscopy, so the Jointoscopy. Two small incisions are made in the knee joint under local anesthesia. The camera and light are inserted through one section and examination instruments are inserted into the other. The advantage of the jointoscopy is that the meniscus damage can be treated directly if the result is positive. A non-standard examination of meniscal damage is the Ultrasonic of the knee joint, which is only used if there is a suspicion of further damaged structures around the meniscus. This can be used to diagnose injuries to the ligamentous apparatus or effusions of the knee joint.
MRI for a meniscus tear
At a MRI The device is a tube which, through the use of magnetic fields, can show the structures of the knee joint well. The MRI examination is completely painless. The length of the examination varies depending on the number of images required. As a rule, half an hour can be assumed, during which the examined person should lie as still as possible in the tube so that the images do not blur and an assessment of the injury is possible.
In many cases, the suspected diagnosis of a meniscus tear can be made based on the patient's medical history and physical examination.
In order to be able to assess the exact extent of the disease and thus also the suitable therapy options, diagnostic imaging methods are usually used. The menisci of the knee joint can best be explored using a MRI examination be assessed.
Over 90% of meniscus tears can be reliably diagnosed on an MRI. Since this does not involve the use of potentially dangerous radiation, the examination is also suitable for younger people and pregnant women. The MRI examination is also advantageous in the case of acute injuries to the knee joint, since a large number of other soft tissue damages often occur and the MRI enables a comprehensive diagnostic assessment of the injuries.
The MRI examination falls under the non-invasive diagnostic possibilities of assessing knee joint injuries and is therefore usually preferred to a joint endoscopy in diagnostics.
It should be noted that certain factors can prevent an MRI scan from being performed. The MRI examination is particularly not possible if there are non-removable metal parts in the body.
These include metal implants that have remained in the body after bone fractures have been treated, as well as certain implanted pacemakers.
If there is claustrophobia (see also: MRI for claustrophobia) there is the possibility of pushing the affected person into the tube only up to the upper body during the MRI examination of the knee.
therapy
The type of therapy depends on the size of the meniscus damage, the pain and the injured structures. In the event of acute meniscus damage, first aid must be initiated. Self-treatment includes that Cool of the knee with cold compresses or ice packs. Never place the cooling element directly on bare skin. This can lead to dangerous icing! Put the affected leg still and, ideally, elevate it. Both of these reduce the swelling in the knee joint by restricting the blood supply. However, if you have severe pain, you should consult a doctor. There is a possibility that other structures besides the meniscus have been damaged.
Without surgery
Not all meniscus damage needs to be treated surgically. Often, non-surgical therapy is sufficient. Small cracks in the outer zone of the meniscus, which is well supplied with blood, heal optimally without surgery. The basis of this form of therapy is maintained by your doctor using appropriate pain medication. Additional anti-inflammatory cortisone can be injected into the affected knee joint. It is also important to protect the knee joint and to cool it. After a few weeks it is recommended physiotherapy to build muscle in the leg and knee joint. The success of this conservative treatment depends on the extent of the meniscus damage. In the event of failure, there is still the possibility of an operative correction.
With OP
The goal of surgery for meniscus damage is to restore mobility in the knee in order to preserve as much healthy meniscal tissue as possible. A distinction is made between two types of surgical intervention: arthroscopy or arthroscopy and open surgery.
In arthroscopy, only small incisions are made in the skin and the damage in the meniscus is sutured or removed using a camera and instruments. Advantages are less injury to the skin, faster healing tendency and one small scar.
The open surgery, which is preferably used for additional injuries to ligaments or the joint capsule, enables the meniscus damage to be repaired via an approximately five-centimeter-long skin incision, which is sutured at the end of the operation. Regardless of the method of access to the knee joint, there are three different techniques that can be used to repair the meniscus damage. With the meniscus suturing, the torn meniscus tissue is sewn back onto the undamaged tissue and thus brought into its original position. The sutures used are dissolved by the body after a while. The prerequisite for this method is an incomplete tear of the meniscus as well as an intact connection to the joint capsule, as this is the Blood supply guaranteed. The meniscus suture is the best possible method, as it is the most likely to restore the anatomical conditions. However, it only allows the load to build up slowly over several weeks after the operation so that the meniscus damage can grow together and heal.
Complete resumption of sporting activities is only possible after three months at the earliest. When removing the meniscus, the torn off portion or even the entire meniscus is surgically removed. This method is mainly used in the case of age-related wear of the meniscus or parts of the meniscus that have broken loose and separated from the blood supply. The Meniscus resection can be performed on an outpatient basis during a session without a subsequent hospitalization. Patients are given walking aids and can resume sitting activities after just one to two weeks. A corresponding one is also recommended physiotherapy. Of a Meniscus replacement one speaks when a new meniscus is inserted into the knee joint after the meniscus has been completely removed. As a rule, the implantation, i.e. the insertion, is carried out during a jointoscopy. The new meniscus is either a meniscus donation from a deceased person or a synthetic meniscus.
Not every meniscus fits into every joint, which is why a size adjustment is necessary. The donor meniscus from the dead is increasingly used by young people who suffer from severe knee problems due to early signs of wear and tear and frequent meniscus damage. The replacement of the meniscus is a lengthy process that requires a few months of follow-up treatment. The general risks of surgical therapy for meniscus damage are secondary bleeding, Infections in the knee joint and effusions. Continued pain or pain recurrence, implant loosening or renewed meniscus damage, which in turn can result in another operation, are also consequential risks.
Bandages
The care of meniscus damage with a bandage is ideal for follow-up treatment as part of a meniscus operation. This also applies to minor injuries, as it protects the meniscus from further damage. The bandage generally enables the recovery process to be accelerated by always exerting moderate pressure on the knee joint and thus slightly stimulating the muscles of the knee, especially when walking. A bandage for meniscus damage gives stability and security. In addition, it enables relief of the menisci. This promotes the healing process of the meniscus damage and is as extensive as possible Freedom from pain generated in motion. In consultation with your doctor, you can have your individual bandage adjusted by a medical supply store.
Figure meniscus
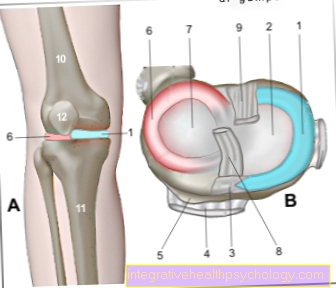
- Inner meniscus -
Meniscus medialis - Inner articular knot
(Shinb.) -
Medial condyle - Transverse ligament of the knee joint -
Lig. Transversum genus - Kneecap ligament - Lig. Patellae
- Bursa - Bursa
- External meniscus -
Lateral meniscus - Outer joint nodules
(Shinb.) -
Lateral condyle - Anterior cruciate ligament -
Lig. Cruciatum anterius - Posterior cruciate ligament -
Lig. Cruciatum posterius - Femur - Femur
- Shin - Tibia
- Kneecap - patella
You can find an overview of all Dr-Gumpert images at: medical illustrations
forecast
As a rule, injury-related meniscus damage heals relatively well. Especially if the lesion is in the area of the meniscus that is well supplied with blood. This promotes the healing process by supplying nutrients and removing metabolic products. Excluded from this, however, are professional groups or athletes who place increased stress on their knee joint. They are at increased risk of renewed meniscus damage.
Meniscus damage caused by age-related wear and tear is unfortunately progressive, that is, with increasing deterioration. If early treatment is not initiated, additional symptoms such as Effusions and Cartilage damage promote. Long-term wear and tear, known as osteoarthritis, can even occur in the knee joint. A meniscus tear can also become progressively larger if left untreated, up to a complete tear-off.
The duration of the healing process of a meniscus damage is of course always dependent on the accompanying symptoms, such as injuries to the ligamentous apparatus in the knee joint. If you continue to suffer from severe pain after initiating the first aid measures, it is essential to consult a doctor. The sooner the right treatment is started, the better the chances of healing your meniscus damage.
Sports
If the meniscus is damaged, sports such as football or skiing that put a lot of strain on the knee should be avoided as far as possible. Are to be recommended activities that are gentle on the jointslike swimming or cycling. In addition, regular gymnastic exercises keep the knee joints flexible. However, make sure you have a regular one Warm up training before exercise to prevent injuries. For sports that place increased strain on the knee, you should use appropriate protectors or joint guards. These counteract an injury to the meniscus in the event of an impending accident.