Hirschsprung's disease
definition
Hirschsprung's disease is a rare congenital disease. It occurs at a frequency of about 1 in 3,000 to 5,000 affected newborns. The disease manifests itself in the gastrointestinal tract.
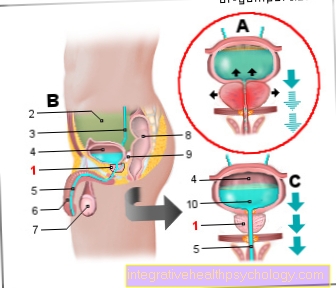
Nerve cells and nerve cell bundles (ganglia) are missing in part of the intestine. In technical terms, one speaks of aganglionosis. In addition to the intestine, the internal sphincter muscle, which is responsible for stool continence, is also affected by the lack of nerve cells. Due to the lack of nerve cells in sections of the intestine, the stool can no longer be transported in the direction of the anus by wave-like muscle movements (peristalsis), so that the intestinal contents / stool build up in front of the diseased section of the intestine because the muscles of the affected area can no longer relax, creating a constriction arises.

Hirschsprung's disease usually only affects the large intestine; the small intestine can only very rarely be affected by the disease. In about three quarters of cases, the sigmoid colon and rectum are affected, i.e. the two end sections of the large intestine. The entire colon is affected in less than ten percent of patients. The symptoms are more pronounced in these patients.
The condition occurs in newborns or infants. Only in very few cases can it only show up in adulthood. This is usually the case when the affected nerve-free section of the intestine is only very short and therefore has little weight.
Read more on the topic: Pain in the colon.
causes
Hirschsprung's disease is caused by impaired embryonic development that occurs between the fourth and twelfth week of pregnancy. The nerve cells (ganglia) cannot migrate into the nerve plexus of the so-called myenteric plexus, which is normally located within the intestinal wall muscles. To compensate for the lack of immigration of nerve cells into the intestinal wall, a neural network is connected upstream in the intestine, which releases the messenger substance acetylcholine to a greater extent. Acetylcholine increases the activity of the intestinal muscles, so that the constant tension (spasticity) of the intestinal muscles associated with the disease arises.
A genetic component definitely plays a role in the disease. The disease can be inherited as an autosomal dominant or an autosomal recessive trait. But there are also many children who do not carry any of the typical gene mutations and in whom the disease was not passed on through heredity.If parts of the intestine in the unborn child are insufficiently supplied with blood or if a viral infection occurs, this can also trigger the disease.
Find out more about the topic here: Autonomic Nervous System
Symptoms
The symptoms of Hirschsprung's disease show up in the newborn. The child attracts attention because of a very distended belly. On the other hand, the first thin stool (technically called meconium) should be secreted within the first 24 to 48 hours. In newborns with Hirschsprung's disease, the first stool is delivered late or usually not at all. In some cases this happens because an intestinal obstruction (ileus) has already formed. Sometimes bilious vomiting can also occur.
If the child is examined in the clinic as part of a rectal examination due to their symptoms, the doctor will notice an increased muscle tone of the sphincter, while there is a lot of stool in the abdomen, but the rectum is empty.
Also read the article: Meconium ileus.
Diagnosis
Based on the underlying symptoms, various diagnostic procedures are set in motion. At the beginning, the stomach is first examined by palpation and listening. In some cases, stool resistance can be felt, which is caused by the stool in front of the narrowed and affected intestinal area. This is usually followed by an ultrasound examination of the abdomen, in which you can see how full the intestine is and whether there are any widening. This is usually followed by an x-ray of the abdomen.
A mucosal biopsy of a section of the intestine ultimately leads to a definitive diagnosis, which can then be used to clearly determine which intestinal segments are affected. You can also stretch the rectum (rectal pressure measurement). Normally, following the stretching of the rectum, there should be a relaxation reflex of the internal sphincter, but this does not occur in the case of Hirschsprung's disease.
X-ray
The suspicion of an underlying Hirschsprung's disease can usually be confirmed by the X-ray. For the X-ray examination, contrast medium is introduced into the colon. Characteristically, if Hirschsprung's disease is present, a jump in the diameter of the intestine can be determined. The segment affected by the disease is narrow. In front of this point there is again a significantly enlarged section of the intestine, since the stool accumulates in front of the adjoining constriction. One speaks of the so-called megacolon, which can be seen on X-rays as a key feature of Hirschsprung's disease.
Even if the diagnosis of Hirschsprung's disease can often already be made by means of the X-ray examination, it does not make the subsequent mucosal biopsy superfluous, because the typical megacolon cannot always actually be seen in an X-ray if the disease is present. Especially when only a short section of the intestine is affected.
Mucosal biopsy
The diagnosis of Hirschsprung's disease is confirmed by a biopsy of the intestinal mucosa. The biopsy can be used to prove that there are no ganglion cells within the muscles of sections of the colon and thus determine which sections of the colon are affected. This is important to know for the subsequent operation. Furthermore, one can detect an increased concentration of acetylcholinesterase, an enzyme that breaks down an important messenger substance, acetylcholine, which is excessively active in the disease. The biopsy is performed either under general anesthesia or under sedation (calming down).
You can find out more about this here: Biopsy.
Therapy of Hirschsprung's disease
The treatment of Hirschsprung's disease cannot be conservative, but must be performed surgically. At the beginning, an artificial anus is sometimes surgically created (anus praeter) so that bowel movements can occur. The artificial anus is created in front of the area affected by the disease. This means that the illness can be bridged for a certain period of time so that the state of health can stabilize again and the child can finally be operated on in a better condition.
In a second surgical step, the diseased intestinal segment is then removed (Resection) and the remaining sections of the intestine are connected to the still short part of the rectum. The operation does not take place in a large open abdominal operation, but usually the operation can be performed through the anus (transanal). Sometimes a minimally invasive procedure (laparoscopic) has to be used. The creation of an artificial anus can often be avoided at the beginning and the affected section of the intestine can be removed directly.
After the operation, regular bowel movements must be ensured. The frequency of emptying and consistency of the stool should return to normal within a few weeks to months after surgery. About 90% of the children are normal after the operation.
What do I have to pay attention to when eating?
The main problem after surgery for Hirschsprung's disease is a persistent tendency to constipation and gas. It is therefore important to pay attention to the following things when eating:
-
Avoid constipating foods: chocolate, cocoa drinks, banana, white bread, white rice, too many sweets.
-
Avoidance of flatulent foods: peas, beans, other legumes, foods that are too fatty
-
adequate hydration. The German Nutrition Society (DGE) recommends the following drinking quantities for healthy people:
baby | 400-600ml per day |
1 - 4 years | 820ml per day |
4 - 7 years | 940 ml per day |
7-10 years | 970 ml per day |
10 - 13 years | 1170ml per day |
13-15 years | 1330ml per day |
15-19 years | 1530ml per day |
Adults | 1410 ml per day |
Complications
Since newborns with Hirschsprung's disease often do not pass stool, an artificial stool must be cleared. If this is not done in time, a complication known as necrotizing enterocolitis can occur, which is an acute, life-threatening disease of the gastrointestinal tract.
If the stool is overly colonized with bacteria, it can lead to a toxic megacolon, i.e. acute intestinal inflammation. Dreaded and life-threatening complications are blood poisoning (sepsis) and inflammation of the peritoneum (peritonitis).
The megacolon as a complication
In Hirschsprung's disease, depending on the extent of the disease, most often the nerve cells of the rectum and the sigmoid loops are missing. Due to the lack of nerve cells in the large intestine, the intestine is very narrow in these areas. The stool can only pass through this narrow point in very small quantities or not at all. As a result, there is an expansion of the intestinal sections that are in front of the constriction. The enlargement of the large intestine is called megacolon in medicine (Greek for "large intestine").
This complication almost always occurs with Hirschsprung's disease if it is not discovered beforehand (e.g. due to the lack of loss of Kindspech). In 15% of the cases a toxic megacolon develops, the enlarged intestine is attacked by a bacterium called Clostridium.
For more information, read on: Toxic megacolon.
Hirschsprung's disease in babies
Hirschsprung's disease is a disease that typically affects babies. It usually manifests itself immediately after birth. If the disease only affects a short segment of the intestine, the children are often only noticed after weaning. Until the children are switched to the right food, the chair is usually thin, so that it can more easily overcome the constriction and the "Hirschsprung children" do not attract attention immediately after birth. After switching from pure breastfeeding to supplementary food, the children then usually show massive constipation and the other typical symptoms.
As already mentioned, the disease usually manifests itself a few hours / days after the birth.
Inheritance in Hirschsprung's disease
Hirschsprung's disease is an inherited disease. Whereby not a specific gene can be determined as the trigger of the disease. Depending on which gene is affected, the disease is inherited as an autosomal dominant or an autosomal recessive trait. Autosomal dominant means that if the newborn is inherited a sick gene from one of its parents, it is automatically sick. With autosomal recessive inheritance, the child needs two diseased genes, i.e. a diseased gene from the mother and a diseased gene from the father, in order to develop the disease. Consequently, the risk of developing Hirschsprung's disease is significantly lower with autosomal recessive inheritance than with autosomal dominant inheritance.
Research has shown that the longer the diseased section of the intestine, the greater the risk of it being passed on to children. Boys are about four times more likely to be affected by the disease than girls. The disease is also more common in children with trisomy 21 (Down syndrome). About 12% of children with Down syndrome also have Hirschsprung's disease.
Is it possible to cure Hirschsprung's disease?
Hirschsprung's disease is an intestinal disease with a very good prognosis. 80 to 85% of patients with Hirschsprung's disease are only affected in the rectum and in the sigmoid loop. Surgical removal of the intestinal sections that are not equipped with nerve cells is therefore quite easy and due to the large proportion of remaining large intestine, the later complications are also less pronounced. Most patients have a normal quality of life after this operation and are to be considered "cured".
About 30% of those affected continue to suffer from a tendency to constipation and possibly other symptoms, which are mentioned below. Unfortunately, about half of the colon is affected in 10 to 15% of patients and the entire colon is affected by Hirschsprung's disease in about 5%. With these so-called “long-term aganglionoses” (aganglionosis is another technical term for Hirschsprung's disease), the prognosis is somewhat worse and complications occur more frequently. Possible complications are: incontinence, tendency to constipation, formation of scarred constrictions in the bowel, inflammation of the bowel caused by bacteria. Patients with a long-term extent of Hirschsprung's disease are then cured of Hirschsprung's disease, but have to struggle with these complications.
What is the life expectancy with Hirschsprung's disease?
Whether or not life expectancy is limited with Hirschsprung's disease depends on the accompanying malformations that also affect a patient. In 70% of the cases, the affected children are completely healthy except for Hirschsprung's disease. Life expectancy is not restricted and corresponds to that of other children.
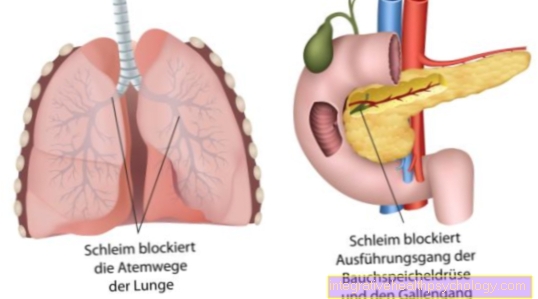
In 30% of cases, children with Hirschsprung's disease have other diseases. These include, for example, Down syndrome and other hereditary syndromes. Life expectancy depends on the syndrome the child is suffering from. In rare cases, Hirschsprung's disease occurs together with other malformations without a syndrome being present. Life expectancy can then be limited depending on the accompanying malformation (e.g. underdeveloped lungs).
What symptoms does Hirschsprung's disease show in adults?
Adults with Hirschsprung's disease have to be divided into two groups. The first group consists of adults who were diagnosed with Hirschsprung's disease as a child and who had an operation. Depending on the extent of the operation, these patients either have no symptoms at all or suffer from mild to severe complications.
Symptoms may include incontinence (patients cannot control bowel movements) or a tendency to be constipated. Scarred constrictions of the intestine can also develop, which can lead to digestive problems or an intestinal obstruction, which then has to be operated on. Some patients still suffer from frequent inflammation of the bowel caused by bacteria in adulthood.
The second group of patients with Hirschsprung's disease in adulthood consists of those who were not diagnosed as children. This only affects a small percentage of people with Hirschsprung's disease. Over 90% are diagnosed as a baby, the majority of the remaining patients in later childhood. Typically, patients who are not diagnosed until they are adults are those with only a short section of the intestine affected.
The typical symptom of these patients is constipation, which is difficult to control even with a high-fiber, healthy diet and adequate fluid intake and light laxative measures. Often, these patients can only pass a bowel movement with one enema and experience severe pain.
Constipation - What Can You Do About It? Read more here.


.jpg)












.jpg)








